Abstract
Living in the vicinity of nuclear power plants (NPP) is discussed here in terms of adverse health effects. A prospective population-based cohort study was conducted to evaluate whether the prevalence of birth defects in the vicinity of NPPs is elevated and scrutinize a possible distance correlation. A birth cohort born to mothers living within 10 km of two selected NPPs (study region) was compared to a region without NPP (comparison region), and an active surveillance of all live births, stillbirths, and induced abortions in the defined regions was performed. Between 01/2007 and 02/2008, all newborns were examined by specially trained study paediatricians according to the protocols of the Birth Registry Mainz Model. The cohort consisted of 5,273 infants (90% completeness). The outcome measure was an infant with birth defect(s). The prevalence of infants with birth defects was 4.5% in the study region and 4.7% in the comparison region, which corresponds to a relative risk (RR) of 0.94 (lower 95% confidence level (CL): 0.76). Thus, the prevalence of birth defects in the regions surrounding NPPs was not increased compared to those of the comparison region. Adjustment for potential confounders did not substantially change the result (RR 0.90, lower 95% CL 0.73). The adjusted and unadjusted distance approach (1/distance in km) did not show any correlation to vicinity to a NPP (p = 0.38). Specifically, within the study region, the prevalence of birth defects showed no upward trend with decreasing distance. Birth defect prevalence and most descriptive parameters in the comparison region were identical to those in the Birth Registry Mainz Model.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ionizing radiation is widely known to cause adverse health effects in animal experiments and humans, including the unborn infant (Wigle et al. 2007, Brent 1999; De Santis et al. 2007; Doll 1995; Kim et al. 2001a, b; Shepard 2001; Bridges (COMARE) (2004). Various types of birth defects (BDs), mainly chromosomal aberrations or anomalies of the central nervous system but also others, have been described (Dolk and Lechat 1993; EUROCAT Working Group 1988; Little 1993; Yamazaki 1966). This leads to the question whether living close to nuclear power plants (NPPs) could result in health effects such as BDs, because an association was found between living in the vicinity of NPPs and childhood leukaemia in a German study (Kaatsch et al. 2008; Spix et al. 2008). Although recalculations in a British cohort could not confirm these findings (Bithell et al. 2008), the question of adverse health effects remains.
Active population-based malformation registries consistently report 2–6% of BDs in newborns. The difference is mainly due to variations in definitions, standardization, inclusion/exclusion criteria (e.g. stillbirth, terminations of pregnancy), and to ascertaining only certain defects (Lynberg and Edmonds 1992).
To investigate BDs in infants born to mothers living close to NPPs, we set up a cohort study following mothers from conception to birth with the BD status of the newborn as outcome and residence at conception as proxy of exposure. The main question was whether a higher prevalence of BDs is diagnosed near NPPs (study region) compared to a region without NPP. The second question investigated the possibility of a trend with distance to the nearest NPP within the study region.
The active, population-based Birth Registry Mainz Model (MaMo) has experience with systematic registration of all births and BDs since 1990. Up to 2009, data on almost 70,000 births and pregnancies were collected. The MaMo monitors the region of the city of Mainz and its surroundings (Rheinhessen, Germany). All procedures (questionnaire, examination, etc.) and know-how about obstetric departments, perinatal centres and departments of pathology were adapted to the needs of the present study as implied by a feasibility study. The standardized MaMo procedures were described in detail analysing a data set of 40,083 infants for the registration period 1990–2001 (Queisser-Luft et al. 2002).
Materials and methods
The study design is a population-based, prospective cohort approach following mothers from conception to birth with the BD status of the infant as an outcome and residence at conception as a proxy for exposure. An “infant” was defined as a livebirth, stillbirth or aborted foetus. The aim was to determine the prevalence of BDs in a pre-defined region surrounding selected NPPs compared to that in a pre-defined comparison region without any NPPs. The second question investigated the possibility of a trend with distance to the nearest NPP within the study region. The study design and procedures were chosen after a preceding feasibility study (November 2006 to January, 2007; n = 532 infants) (Queißer-Luft 2007). The study region consisted of circles with a radius of 10 km around the selected two NPPs. The comparison region had to be more than 20 km away from any NPP and less than 100 km from the study region. Study and comparison regions were selected ensuring a sufficient number of births. Following these criteria, the selected study region included the two NPPs Biblis and Philippsburg and comprised all postal codes inside and tangent of the 10-km radius of the NPPs with 2,400 births per year. The comparison region consisted of the cities of Kaiserslautern, Pirmasens and Zweibrücken, and the counties of Kaiserslautern and South-West-Palatinate with 2,800 births per year based on postal codes. Calculations of expected number of births were based on hospital deliveries and federal state numbers from previous years. A BD registration had previously not been established in these regions. The field phase was conducted between 17th of January 2007 and 29th of February 2008.
Assuming an inclusion of 90% of the regional births and an almost 100% detection of BDs, the expected statistical power to compare the two regions for an increase in the BD prevalence from 5.0% in the comparison region to 7.0% in the study region—corresponding to a relative risk (RR) of 1.4—is greater than 90%. The power would still be around 80% for a RR of 1.2. The assumption of a 5.0% baseline prevalence is based on the experience of the MaMo, where the annual BD prevalence varies between 4.7 and 6.4%. Note, however, that the MaMo cohort differed somewhat from the present study population: inclusion of spontaneous abortions (≥16th week of gestation), routine screening for dislocation of hip and birth defects with causal relations (diabetic embryopathy due to maternal insulin-dependent diabetes mellitus), and the diagnosis “isolated microcephaly” is included in MaMo but was not counted in the present study [counted as minor variant by EUROCAT Dolk 1991)]. Recalculated numbers are presented for comparison and completeness.
Births and regions
Data were obtained from 31 hospitals and institutions (obstetric departments, children’s hospitals, centres for prenatal diagnosis and departments of pathology) in and around the study and comparison regions. Fifteen of these obstetric departments had more than 50 study-relevant births per year and were monitored on a daily/weekly basis, expected to cover about 90% of the relevant births. Special procedures applied in the following rare cases: In eight hospitals with fewer than 50 relevant births per year, a minimal data set (date of birth, recent address, gender, weight, length, head circumference, birth defect(s)) as noted in the clinical record of the infant was recorded at the end of the study. Similarly, this minimal data set was recorded following parentally diagnosed abortions and stillbirths collected from all prenatal centres or departments of pathology within or surrounding the monitored regions.
In the study period, a total of 6,038 infants were examined. Out of these, 3,154 infants belonged to the study region and 2,884 infants to the comparison region. Geocoding on the basis of exact house coordinates was available for 98.1% of the addresses in the study region, at the end of the field phase. Seven hundred and sixty-five infants were not included in the analyses, because the maternal residence was located outside the 10-km radius or did not meet the inclusion criteria. Out of the 5,273 data sets eligible for analyses, only 207 (3.9%) consisted of the minimal data set. Therefore, no further sensitivity calculations were performed concerning this matter under the reasonable assumption of an unselected sample.
As a consequence of the fact that the population coverage needed to be calculated from the residential address at conception, an adjustment was needed for any change of maternal residence during pregnancy (i.e., relevant mothers moving out of and study-irrelevant mothers moving into the study region), which was possible only after geocoding. After exclusion of 3.4% mothers relocating into the study region after the first trimester, 2,709 relevant births were estimated, based on the numbers of the Statistical Federal State Office for the year 2007 and for the 13.5-month study period (2,806 births). Out of these, 2,423 were included in the study (population coverage 89.4%). Within the same time period, 3,288 births were officially registered in the comparison region. Excluding the 3.4% leaves 3,176 as denominator, and the 2,850 infants eligible for analyses correspond to a coverage of 89.7%. There was no relevant difference in the participation rate (only live births) of answering the additional study questionnaire, between the study region (71.0%) and the comparison region (73.5%), and no further sensitivity analyses were therefore performed.
Ethics, consent and guidelines
All procedures were approved by the ethics committee of the responsible “Landesärztekammer Rheinland Pfalz” and met the criteria of the data protection rules of Rhineland-Palatinate. The “Landesärztekammer Rheinland Pfalz” is a State Authorisation Association for Medical Issues, including Ethics Committees, i.e., an Association for Physicians. A maternal consent for the scientific usage of obstetric routine data was included in the hospital–patient contract that allowed anonymous use of the data. Thus, all routine data—including BDs and anamnesis—were available for all infants. A separate maternal consent concerned the study-specific questionnaire (such as prenatal radiation exposure in early pregnancy) and usage of the residential address. The Guidelines of “Good Epidemiological Practice” (GEP) (IEA 2004) were respected. “STROBE” recommendations for the publication of cohort studies were regarded (Vandenbroucke et al. 2007).
Ascertainment procedures, inclusion criteria and examination
A mother was included in the study, provided her residential address at beginning of pregnancy belonged to the defined regions. All ongoing pregnancies ≥20 weeks of gestation and all foetuses aborted following prenatally diagnosed BDs within the covered regions were included in the study. In Germany, the registration of spontaneous abortions (<20th week of gestation) is not regulated and, therefore, these could not be included in the study.
In Germany, mothers usually present themselves at the obstetric department some weeks prior to birth. The relevant mothers were then provided with information concerning the study. A written consent concerning the child’s name, the extra questionnaire data and residential address was obtained by the involved midwives. To minimize recall bias, personal data relating to mother, father, pregnancy and foetus were also recorded at this point of time. Mothers had to understand German fairly well as all documents and consents where only in German language.
Eight study paediatricians were appointed for this project by the heads of the local paediatric hospitals. They were required to have at least 4 years of clinical and neonatological experience. The study paediatricians were equipped with a car, a portable ultrasound unit (Micromaxx, Sonosite, USA, with 7.5-MHz linear transducer) and a notebook (Macbook, Apple, USA) displaying the computer-assisted data entry software (CADE). Additionally, they were trained in standardized examination methods defined for the study in special seminars by members of the study centre. The paediatricians were retrained in the course of the field phase. They used the ward records at their daily/appointed visits and verified the mother’s residence at conception. Within the first week of life, all livebirths were examined in the maternity hospital following a detailed standardized protocol including a renal ultrasound scan. The data was completed during the hospital stay of the newborn/mother.
Routine data were available for all ascertained infants, including descriptive core variables such as weeks of gestation, biometric markers of the infant (e.g. length, weight), pregnancy risks (e.g. placental insufficiency, gestational diabetes), parity, socio-economic status (SES; analysed in three categories), smoking, ethnicity, pre-pregnancy body mass index (calculated from weight and height by the maternity protocol or ward file) and artificial reproductive techniques (ART). In ART, intra-cytoplasmatic sperm injection (ICSI) cases were counted separately from in vitro fertilization (IVF) cases, since ICSI is discussed to be associated with BDs and addressed as possible confounder (Hansen et al. 2005). Further potential confounders and known risk factors are birth defects in first-degree relatives (defined as parents and siblings), maternal age at birth, maternal medication in pregnancy (e.g. anticonvulsive therapy, folic acid), maternal insulin-dependent diabetes mellitus, consanguinity and maternal alcohol/drug addiction. The answers to the questionnaire on maternal diagnostic X-ray exposure, occupational exposure to ionizing radiation and/or exposure to pesticides/insecticides were only added if written consent was given. All data were transferred to the computerized version of the questionnaire (CADE; automatic plausibility checks) by the study paediatricians, completed by routine data and findings of the infant’s physical/ultrasound examinations.
Home deliveries were not included, as the number was estimated to be approximately 25 births during the study period and within the regions, involving only ca. 0.3% BDs (QUAG 2006).
Birth defects
The outcome “birth defect” was defined as a structural defect of the body and/or the organs, which affects viability and quality of life and which requires medical intervention according to the definition of the World Health Organisation (WHO 2005). A catalogue of birth defects was provided by the study centre and handed out to the study paediatricians at the training seminars. BDs were classified according to EUROCAT (EUROCAT Report 8 2002, EUROCAT Guide 1.3 2005). All BD cases were uniformly categorized case by case into established organ categories (musculoskeletal system, cardiovascular system, internal/external urogenital system, central nervous system, digestive system, chromosomal aberrations, facial clefts, eye, ear), into isolated or multiple birth defects (including sequences and associations, chromosomal or non-chromosomal syndromes), as well as into malformations, deformations, dysplasias and disruptions (Queißer-Luft and Spranger 2006). After the end of the field phase, an independent international expert panel—blinded for the region—assessed the diagnosed BDs and categorization of the infant. The panel consisted of four specialists in the fields of paediatrics, genetics and BD research.
Statistical analysis
Total prevalence of BDs is based on infants, not births. One infant can be affected by more than one BD. A sensitivity analysis was performed excluding deformations (Spranger et al. 1982). For the first question, a crude RR estimate comparing the study region and the comparison region was calculated as the ratio of the BD prevalence. The one-sided lower 95% confidence limit of the RR was determined. Further analyses required regression techniques, and proportions are usually analysed by log-linear regression (generalized models with canonical log link). In such models, the RR could alternatively be determined by including an indicator for “region”. The question of a trend within the study region was addressed by modelling 1/distance (Kaatsch et al. 2008) and the regression coefficient β calculated. All known potential confounders (i.e., birth defects in the first-degree relatives, maternal age ≥ 35 years, maternal BMI ≥ 30, maternal and paternal occupational exposure to ionizing radiation, maternal medical exposure to ionizing radiation, maternal β-agonist use, ICSI) were included in both regression models. For a subset of the mothers, no questionnaire data were available; therefore, “missing” was used as a separate category. A subset was selected by stepwise backwards elimination (p < 0.1). In the present paper, the crude RR and crude trend coefficient as well as the adjusted measures of the end model are reported.
All regional comparisons and distance relationships were assessed by one-sided tests (α = 5%) and the corresponding lower 95% confidence limit (CL). The lower CL has to be greater than unity to indicate significance, as only a potential increase was tested (no protective effect was assumed). Descriptive parameters and potential confounders are shown in absolute and relative numbers with missing values as a separate category. Furthermore, a sensitivity analysis was performed, calculating fractional polynomials [(1/r)3, (1/r)2, 1/r, (1/r)0.5, log (1/r), r 0.5, r, r 2, r 3] to describe possible distance correlation (Royston et al. 1999). For statistical analyses, the software package SAS 8.12., Cary, USA, was used.
Results
The final analysis included 2,423 infants in the study region and 2,850 in the comparison region (total 5,273) (Fig. 1). The final data set included 2,394 (98.8%) livebirths and 29 (1.2%) stillbirths/induced abortions in the study region. The comparison region included 2,824 (99.1%) live births and 26 (0.9%) stillbirths/induced abortions (Table 1).
A BD was diagnosed in 4.5% of the infants in the study region (108/2,423) and 4.7% of the infants in the comparison region (135/2,850), yielding a crude RR = 0.94 (lower CL: 0.76). The log-linear regression model yielded a RR = 0.89 (lower CL: 0.72) for the fully adjusted model and a RR = 0.90 (lower CL: 0.70) for the more parsimonious end model (stepwise backward elimination). The final model included only known birth defects within first-degree family members (RR = 4.44; confidence interval (CI): 3.0 to 6.5) and maternal occupational exposure to ionizing radiation in the first trimester of pregnancy (RR = 2.15; CI: 0.9 to 5.2) as potential confounders.
In Table 2, other potential confounders/risk factors for BDs are listed. ICSI was used more frequently in the study region (1.3%) than in the comparison region (0.4%). In both regions, the observed prevalence of birth defects was higher in ICSI conceived than in spontaneously conceived infants (study region 6%, 2/31; comparison region 18%, 2/11). More mothers in the study region than in the comparison region received unspecified medications (9.0% vs. 5.3%). Two drugs specifically known to induce birth defects (β2-agonists—ATC Code R03, and antiepileptic drugs—ATC Code N03) did not influence the results as only a few mothers took them (World Health Organisation (WHO) 2005). According to the questionnaires, more mothers in the study region than in the comparison region had been exposed to medical or occupational ionizing radiation. Both exposures were more frequently reported by the mothers of malformed infants (Table 2).
Excluding deformations from the analysis resulted in 100/2,415 infants with birth defects in the study region and 111/2,826 in the comparison region, corresponding to an RR of 1.05 (lower CL 0.84). The adjusted regression model, including the same two potential confounders as above, yielded an RR of 1.00 (lower CL 0.80) (Table 3).
None of the defined organ categories showed a relevant absolute or relative increase in the corresponding BDs in the study region. Isolated BDs occurred in 79/108 (73.1%) infants in the study region and 102/135 (75.6%) infants in the comparison region. Multiple congenital birth defects were diagnosed in 22 infants of the study region (0.9%) and 23 infants of the comparison region (0.8%). Five cases of trisomy occurred in the study region and eight cases in the comparison region. Neural tube defects (NTDs) were diagnosed twice in the study region and three times in the comparison region, respectively.
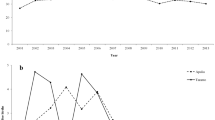
The association between the prevalence of BDs and distance of maternal residence at the beginning of pregnancy to the nearest NPP was analysed only in the study region. The distribution of BD prevalence by distance is demonstrated in Fig. 2. Neither the unadjusted β = 0.36 (lower CL: −1.59) nor the adjusted β = 0.37 (lower CL: −1.56) showed an increased BD risk with decreasing distance to the nearest NPP. In the adjusted model, only “known birth defects within the family” remained with an RR of 4.52 [CI 2.69, 7.59; p < 0.0001]. Fractional polynomials of the distance were analysed, with no indication of a trend in other shapes ((1/r)3, (1/r)2, 1/r, (1/r)0.5, log (1/r), r 0.5, r, r 2 (all p > 0.05), and r³ (p = 0.041)).
To address a possible selection bias between mothers answering and not answering the study-specific questionnaire, the BD prevalence in these groups was compared. The prevalence of BDs was higher in the non-participants (i.e., the fractions were 5.1% vs. 4.2% in the study region and 5.6% vs. 4.4% in the comparison region, respectively) (Fig. 1). Comparing the data of the study and comparison regions, most descriptive parameters did not show relevant differences. The proportion of German-born mothers was slightly lower in the study region than in the comparison region, while the number of women with gestational diabetes was 6.2% in the study region and 3.8% in the comparison region (Table 1).
Comparison region compared to the Birth Registry Mainz Model
In the comparison region, 141 of 2,850 infants (4.9%) had at least one BD. Six of these had a known cause (e.g. maternal insulin-dependant diabetes mellitus and diabetic embryopathy in the infant) and were excluded from the NPP-related analysis by expert panel decision. The birth defect prevalence was compared to the published data of the Birth Registry Mainz Model (n = 40,093; crude birth defect prevalence 6.4%) (Queißer-Luft and Spranger 2006). The MaMo prevalence was made comparable as described in the “Materials and methods”. The resulting BD prevalence in the MaMo was 5.0% (1,968 out of 39,292 infants), which is similar to the 4.7% BD prevalence in the comparison region. Additionally, the proportions of infants from multiple pregnancies, of males and of preterm infants (≤37 weeks of gestation) were almost identical. We conclude that transferring the MaMo protocols to the comparison region was successful, which was consequently also assumed for the study region.
Discussion
In Germany, ionizing radiation is measured on a routine basis by governmental institutions. According to the published data for 2007, the underlying natural radiation exposure is approximately 2.1 mSv/y. The man-made radiation exposure accounts for additional 1.9 mSv/year, of which nuclear installations are held responsible for less than 0.01 mSv/y (Bundesamt für Strahlenschutz 2008; Bieringer et al. 2008; Wildermuth and Bünger 2008). For 2005, detailed annual doses due to radioactivity in water and air are available for the surroundings of Biblis (0.0008 mSv) and Philippsburg (0.0031 mSv), which is less than the official requirements on annual effective whole-body dose of less than 0.3 mSv/y (Volkmer 2007; Bieringer et al. 2008; Wildermuth and Bünger 2008). Like in other European countries with official data, these dose rates are far below the believed threshold of 100 mSv per year for teratogenic effects (ICRP 2007). Furthermore, no specific events resulting in an excess dose rate were reported in the relevant region and time.
Birth defects
The prevalence of birth defects in the vicinity of NPPs (10-km radius) and that in the comparison region was almost identical (4.5% compared to 4.7%, RR = 0.94, adjusted RR = 0.90). A further analysis excluding deformations confirmed this result (RR = 1.05, adjusted RR = 1.00). Geocoding the distance of the maternal residence at the beginning of the pregnancy showed that the observed BD prevalences were evenly distributed across the distance from the nearest NPP and showed no trend. There was no indication of an increased risk for BDs caused by living in the proximity of NPPs.
In the present study, BDs previously associated with ionizing radiation, such as NTDs and trisomy, did not show an increased prevalence in the study region. Possible mutagenic/teratogenic effects of low-dose ionizing radiation in humans, however, are difficult to assert in epidemiological studies. Factors influencing possible effects include dose and gestational age at exposure. Published observations on teratogenic effects mainly come from high-dose animal models and man-made hazards such as the Hiroshima and Nagasaki atomic bombs (De Santis et al. 2007), or the Chernobyl accident (Kim et al. 2001b). Trisomy 21 and NTDs are the most common disorders thought to be caused by ionizing radiation, but early data were controversially discussed and not confirmed in recalculations (Caglayan et al. 1989; Hoffmann 2001; Huether et al. 1996; Mocan et al. 1990; Mocan et al. 1992; Ramsay et al. 1991). In 1999, Castronovo stated that detection and selection bias may have influenced those results (Castronovo 1999). More recently, controversially discussed data indicated an increased post-Chernobyl frequency of trisomy 21 in Belarus (Zatsepin et al. 2007) and Germany (Burkart et al. 1997; Sperling et al. 1994). Note that there are only a few population-based studies that met some epidemiological quality standards as outlined in GEP today (IEA 2004). For example, in a case–control study, Sever et al. (1988) found an increased frequency of NTDs in the offspring of workers of the Hanford nuclear site, Washington, USA, compared to controls selected from delivery room log books. In this study, the reported numbers were small and trisomy 21 was not ascertained. Obstetric outcomes including all types of congenital anomalies were investigated in an area close to the Sellafield nuclear site and compared to an “unexposed region” in West Cumbria, UK; increased rates were not identified (Jones and Wheater 1989). In Hungary, the BD rate within a 30-km distance of the Paks nuclear plant was not higher than in the Hungarian Congenital Abnormality Registry (Siffel et al. 1996). Neither the “Nuclear Industry Family Study” in the United Kingdom (1993 to 1996) nor a Canadian study (1979–1986) observed an increase in BDs in infants born to nuclear industry employees (Doyle et al. 2000; Green et al. 1997; Roman et al. 1996).
The regression analysis with potential confounders indicated BDs in first-degree relatives and maternal occupational exposure to ionizing radiation to be independent risk factors. However, these factors had no substantial influence on the main result of the present study (adjusted RR = 0.90).
Some results concerning other known or suspected causes of BDs deserve comments. The prevalence of birth defects after ICSI differed between the regions and was nearly threefold higher in the comparison region than in the study region. Small numbers may explain this observation. The risk factor “ICSI” for BDs was borderline significant in all steps of the model and was eliminated second to last (Green et al. 1997). The risk estimate never differed substantially from the start model (RR = 2.1; 95% CI: 0.77–5.64) and emphasizes that ICSI therapy might be an independent risk factor for BDs. These findings confirm data on ART and BDs (Hansen et al. 2005). Descriptive variables concerning the infant (length, weight, gestational age, etc.), maternal history (SES, drug use, IDDM, etc.) and pregnancy specifications (such as smoking, oligohydramnion and folic acid intake) were compared to assure internal validity and were found to be evenly distributed between the two regions. The prevalence of gestational diabetes differed because of the scientific interest of one hospital in this issue. Minor differences in some variables such as preconception BMI, or maternal age, may reflect socio-demographic differences. According to official statistics, more mothers and fathers with migration background lived in the study region than in the comparison region. The larger fraction of mothers not fluent in the German language explains the higher amount of “not known” answers in the study region (Table 1). According to the questionnaires, more parents in the study region than in the comparison region reported occupational exposure to ionizing radiation sources, which is due to parents employed in the NPPs (Table 2). Exposure to pesticides can be explained by the vineyards in the study region. The more frequent use of diagnostic ionizing radiation in the study region during pregnancy cannot be explained. Neither the maternal medical exposure to ionizing radiation or exposure to pesticides/insecticides at the beginning of the pregnancy nor the paternal occupational exposure to ionizing radiation (wearing a radiation dosimeter at the beginning of pregnancy) proved to be a risk factor for BDs. Results on maternal occupational exposure to ionizing radiation are evaluated elsewhere (Wiesel et al. 2011).
Completeness
To corroborate the validity and quality of the “new” birth cohort, the prevalence of BDs and selected descriptive markers in the comparison region were compared to those in the Birth Registry Mainz Model. These parameters are believed to provide a sound basis for comparison of BDs and risk factors, though they are susceptible to changes over time and local socio-economic conditions. The study region was excluded from this comparison because the vicinity to NPPs could have had an effect on the offspring. Completeness, validity and generalizability were evaluated. As a result, similar prevalence of BDs and other descriptive parameters such as proportions of aborted foetuses, stillbirths, gender distribution, multiple pregnancies and of preterm deliveries were found. This supports the assumption that the cohort of newborns of the present study and the result of the comparison region compared to the published MaMo data do not indicate a selection bias. In view of the identical study design, this conclusion can be extended to the study region surrounding the NPPs. Observed differences in anamnestic maternal- and/or pregnancy-related parameters can be explained by socio-demographic differences in the two populations. Especially, the diagnosis of maternal gestational diabetes in the comparison cohort has to be seen in the light of changing screening policies, benchmarks and obstetric guidelines. In the comparison region, more mothers smoked during pregnancy. Pregnancy in women 35 years or older has become common in the industrialized world, suggesting the difference between the comparison region and MaMo (19.5% vs. 13.3%) to be caused by the different observation periods.
Strengths and limitations of the study
The strengths of the present study is the complete, continuous and standardized registration of all live births, stillbirths and terminations of pregnancies (TOPs), and BDs. All types of BDs were registered allowing recognition of new patterns and combinations (e.g. thalidomide). Additional data about the pregnancies were collected before birth to avoid recall bias. Exact definitions of BDs, a population-based prospective study design, proven ascertainment methods, specially trained investigators and standardized examination procedures ensured reliable results. Planning this study, internal validity was a major issue, as this is always important for ecological studies. Because exactly the same methods were used in the exposed and unexposed regions, any lack of additional information or retrospective data (e.g. exposure questionnaires or terminations of pregnancy) should equivalently apply to both regions.
Limitations of the present study include the difficulty to record personal and study-specific questions from mothers who aborted a malformed foetus following prenatal diagnosis, or who experienced stillbirth, extreme preterm births, and other emergencies treated in an intensive care unit. In the hospitals with fewer than 50 births per year, the infants were ascertained retrospectively by clinical chart review. Because the study paediatricians could not perform the clinical examinations of these infants themselves, differences in the examination and/or coding procedures could theoretically have influenced the results. For those mothers, only the address at birth was used (<3.0%). A general limit of our study is the lack of knowledge about the time the mother actually spent at the given residence. Exposure misclassification may in principle cause a bias towards the null. This would affect the distance relationship within the study region more than the comparison region, as most daily mobility is short distance.
Conclusion
No association was found between a maternal residence at conception close to a nuclear power plant (≤10-km radius) and congenital birth defects in the offspring in the presented study. The risk did not increase with individual vicinity of the residence to the nearest NPP. None of the potential confounders affected the results, proving the robustness of the effect. The comparison of birth defects and further descriptive parameters in the comparison region of the study with those of the long-established MaMo showed identical prevalence, testifying to the validity of the ascertainment method.
References
Bieringer J, Dalheimer A, Dyck W, Steinkopff T (2008) Messnetze für Luft und Niederschlag. In: Bundesamt für Strahlenschutz (2008b) Umweltradioaktivität in der Bundesrepublik Deutschland 2006 und 2007. ISSN 1864-2810 chapter 5; pp 35–40
Bithell JF, Keegan TJ, Kroll ME, Murphy MF, Vincent TJ (2008) Childhood leukaemia near British nuclear installations: methodological issues and recent results. Radiat Prot Dosimetry 132:191–197
Brent RL (1999) Utilization of developmental basic science principles in the evaluation of reproductive risks from pre- and post conception environmental radiation exposures. Teratology 59:182–204
Bridges BA (2004) Chairman. COMARE 8th Report. Available at: http://www.comare.org.uk/press_releases/documents/COMARE8thReporteBook.pdf. Accessed 16 Aug 2010
Bundesamt für Strahlenschutz (2008) Umweltradioaktivität und Strahlenbelastung Jahresbericht 2007. Editor: Bundesministerium für Umwelt, Naturschutz und Reaktorsicherheit (BMU); Bundesamt für Strahlenschutz available at: www.bfs.de/de/bfs/druck/uus/jb07_Gesamtbericht.pdf. Accessed 16 Aug 2010
Burkart W, Grosche B, Schoetzau A (1997) Down syndrome clusters in Germany after the Chernobyl accident. Rad Res 147:321–328
Caglayan S, Kayhan B, Menteşoğlu S, Aksit S (1989) Changing incidence of neural tube defects in Aegean Turkey. Paed Perinat Epidemiol 3:62–65
Castronovo FP Jr (1999) Teratogen update: radiation and Chernobyl. Teratology 60:100–106
De Santis M, Cesari E, Nobili E, Straface G, Cavaliere AF, Caruso A (2007) Radiation effects on development. Birth Def Res C Embryo Today 81:177–182
Dolk H (1991) When in microcephaly an ‘informative morphogenetic variant? Paediatr Perinat Epidemiol 5(4):A10
Dolk H, Lechat MF (1993) Health surveillance in Europe: lessons from EUROCAT and Chernobyl. Int J Epidemiol 22:363–368
Doll R (1995) Hazards of ionising radiation: 100 years of observations on man. Br J Cancer 72:1339–1349
Doyle P, Maconochie N, Roman E, Davies G, Smith PG, Beral V (2000) Fetal death and congenital malformation in babies born to nuclear industry employees: report from the nuclear industry family study. Lancet 356:1293–1299
EUROCAT Central Registry (2005) EUROCAT Guide 1.3 and reference documents Instructions for the Registration and Surveillance of Congenital Anomalies. Available at: http://www.eurocat.ulster.ac.uk. Accessed 13 July 2008
EUROCAT report 8 (2002) Surveillance of congenital anomalies in Europe 1980–1999. Eurocat central registry, University of Ulster, Northern Ireland, also available at www.eurocat.ulster.ac.uk
EUROCAT Working Group (1988) Preliminary evaluation of the impact of the Chernobyl radiological contamination on the frequency of central nervous system malformations in 18 regions of Europe. Paed Perinat Epidemiol 2:253–264
Green LM, Dodds L, Miller AB, Tomkins DJ, Li J, Escobar M (1997) Risk of congenital anomalies in children of parents occupationally exposed to low level ionising radiation. Occup Environ Med 54:629–635
Hansen M, Bower C, Milne E, de Klerk N, Kurinczuk JJ (2005) Assisted reproductive technologies and the risk of birth defects—a systematic review. Hum Reprod 20:328–338
Hoffmann W (2001) Fallout from the Chernobyl nuclear disaster and congenital malformations in Europe. Arch Envir Health 56:478–484
Huether CA, Haroldson K, Ellis PM, Ramsay CN (1996) Impact of prenatal diagnosis on revised livebirth prevalence estimates of Down syndrome in the Lothian region of Scotland, 1978–1992. Gen Epidemiol 13:367–375
IEA Guidelines for proper conduct of epidemiological research (2004) available at http://www.dundee.ac.uk/iea/GoodPract.htm. Accessed 3 June 2008; in German available on http://www.gmds.de/publikationen/1b_LeitlinienUndEmpfehlungen_April2004.pdf
InfasGeoDat (2008) Available at: http://www.infas-geodaten.de/fileadmin/media/pdf/katalog/geodaten_katalog.pdf. Accessed July 3 2008
International Commission on Radiological Protection. Annals of the ICRP (2007) ICRP Publication 103—The 2007 recommendations of the international commission on radiological protection. Elsevier, Amsterdam 2007, ISBN 978-0-7020-3048-2, ISBN-13: 978-0-7020-3063-5, ISBN-10: 0-7020-3063-5, p 332
Jones KP, Wheater AW (1989) Obstetric outcomes in West Cumberland Hospital: is there a risk from Sellafield? J R Soc Med 82:524–527
Kaatsch P, Spix C, Schulze-Rath R, Schmiedel S, Blettner M (2008) Leukaemia in young children living in the vicinity of German nuclear power plants. Int J Cancer 122(4):721–726
Kim SH, Kim SR, Lee YS, Kim TH, Jo SK, Lee CS (2001a) Influence of gestational age at exposure on the prenatal effects of gamma-radiation. J Vet Sci 2(1):37–42
Kim SH, Lee JH, Oh H, Kim SR, Lee CS, Jo SK, Kim TH, Lee YS (2001b) Dependence of malformation upon gestational age and exposed dose of gamma radiation. J Rad Res 42:255–264
Little J (1993) The Chernobyl accident, congenital anomalies and other reproductive outcomes. Paed Perinat Epidemiol 7:121–151
Lynberg MC, Edmonds LD (1992) Surveillance of birth defects. In: Halperin W, Baker EL (eds) Public health surveillance, vol 12. Van Nostrand Reinhold, New York, pp 157–177
Mocan H, Bozkaya H, Mocan MZ, Furtun EM (1990) Changing incidence of anencephaly in the eastern Black Sea region of Turkey and Chernobyl. Paed Perinat Epidemiol 4:264–268
Mocan H, Aydemir V, Bozkaya H, Mocan MZ, Ozbay G (1992) Incidence of neural tube defects (NTD) in Ankara, Turkey, prior to and after the Chernobyl disaster. Paed Perinat Epidemiol 6:111–114
QUAG (2006) Außerklinische Geburtshilfe in Deutschland—Qualitätsbericht 2004/2005 (Gesellschaft für Qualität in der außerklinischen Geburtshilfe e.V. (QUAG web site) available at: http://www.quag.de. Accessed Oct 17 2008
Queißer-Luft A (2007) Machbarkeitsstudie für eine Fall-Kontroll-Studie zu angeborenen Fehlbildungen in der Umgebung von Kernkraftwerken; Strahlenschutzforschung Programmreport 2005/2006. BfS 4334; ISSN 0937-4469, ISBN 978-3-86509-766-8
Queißer-Luft A, Spranger J (2006) Fehlbildungen bei Neugeborenen. Deutsches Ärzteblatt 38:A2464–A2471
Queisser-Luft A, Stolz G, Wiesel A, Schlaefer K, Spranger J (2002) Malformations in newborn: results based on 40, 940 infants and foetuses from the Mainz congenital birth defect monitoring system (1990–1998). Arch Gyn Obstet 266:163–167
Ramsay CN, Ellis PM, Zealley H (1991) Down’s syndrome in the Lothian region of Scotland 1978–1989. Biomed Pharmacother 45:267–272
Roman E, Doyle P, Ansell P, Bull D, Beral V (1996) Health of children born to medical radiographers. Occup Environ Med 53:73–79
Royston P, Ambler G, Sauerbrei W (1999) The use of fractional polynomials to model continuous risk variables in epidemiology. Int J Epidemiol 28:964–974
Sever LE, Gilbert ES, Hessol NA, McIntyre JM (1988) A case-control study of congenital malformations and occupational exposure to low-level ionizing radiation. Am J Epidemiol 127:226–242
Shepard TH (2001) Katalog of teratogenic agens, 10th edn, No. 2108. Radiation John Hopkins University press, pp 365–368
Siffel C, Otos M, Czeizel AE (1996) Congenital abnormalities and indicators of germinal mutations in the vicinity of the Paks nuclear plant, Hungary. Mutagenesis 11:299–303
Sperling K, Pelz J, Wegner RD, Dörries A, Grüters A, Mikkelsen M (1994) Significant increase in trisomy 21 in Berlin nine months after the Chernobyl reactor accident: temporal correlation or causal relation? Brit Med J 309:158–162
Spix C, Schmiedel S, Kaatsch P, Schulze-Rath R, Blettner M (2008) Case-control study on childhood cancer in the vicinity of nuclear power plants in Germany 1980–2003. Eur J Cancer 44(2):275–284
Spranger J, Benirschke K, Hall JG, Lenz W, Lowry RB, Opitz JM, Pinsky L, Schwarzacher HG, Smith DW (1982) Errors in morphogenesis: concepts and terms. J Pediat 100:160–165
Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M (2007) STROBE initiative. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Epidemiology 18:805–835
Volkmer M (2007) Kernenergie Basiswissen. ISBN 3-926956-44-5, pp 84–85. Available at http://www.kernfragen.de/kernfragen/documentpool/018basiswissen2007.pdf. Accessed 6 June 2009
Wiesel A, Spix C, Mergenthaler A, Queißer-Luft A (2011) Maternal occupational exposure to ionizing radiation and birth defects. Radiat Environ Biophys doi:10.1007/s00411-010-0350-9
Wigle DT, Arbuckle TE, Walker M, Wade MG, Liu S, Krewski D (2007) Environmental hazards: evidence for effects on child health. J Toxicol Environ Health B Crit Rev 10:3–39
Wildermuth H, Bünger T (2008) Ableitung radioaktiver Stoffe aus Atomkraftwerken. In: Bundesamt für Strahlenschutz (2008b) Umweltradioaktivität in der Bundesrepublik Deutschland 2006 und 2007. ISSN 1864-2810 chapter 4; pp 27–34
World Health Organisation (WHO) (2005) Available at: http://www.whocc.no/atc_ddd_index/. Accessed 13 July 2005
Yamazaki JN (1966) A review of the literature on the radiation dosage required to cause manifest central nervous system disturbances from in utero and postnatal exposure. Pediatrics Suppl 37:877–902
Zatsepin I, Verger P, Robert-Gnansia E, Gagnière B, Tirmarche M, Khmel R, Babicheva I, Lazijuk G (2007) Down syndrome time-clustering in January 1987 in Belarus: link with the Chernobyl accident? Reprod Toxicol 24:289–295
Acknowledgments
Granted by the “Bundesministerium für Umwelt, Naturschutz und Reaktorsicherheit” through the “Bundesamt für Strahlenschutz” (Grant No. StSch. 4493). The Birth Registry Mainz Model is funded by the Ministry of Work, Social Affairs, Health, Family, and Women of Rhineland-Palatinate and the Department of Medicine of the Johannes Gutenberg University of Mainz, Germany. The scientists were free in design and conduct of the study, as well as the interpretation of the results. Geocoding of the addresses was performed by INFAS GeoDat GmbH (InfasGeoDat 2008). We thank all participating institutes and are very grateful to the efforts of the study paediatricians: Thomas Fabian, Kirsten Henn, Cornelia Joiko, Isabella Munk, Stefan Schmitt, Lucca Seipenbush, Marcel Sena-Pritsch and all co-workers such as midwives, nurses and secretaries. Furthermore, we thank the expert panel for their expertise: Professor Anna Latos-Bielenska, Professor Karl Sperling, Professor Jürgen Spranger and Professor Stefan Wirth. Last but not least, we are most grateful to Professor Jürgen Spranger for his motivating and committed support.
Author information
Authors and Affiliations
Corresponding author
Additional information
The birth defect catalogue, a list of all recorded BDs, and the questionnaire are available from the corresponding author.
Rights and permissions
About this article
Cite this article
Queißer-Luft, A., Wiesel, A., Stolz, G. et al. Birth defects in the vicinity of nuclear power plants in Germany. Radiat Environ Biophys 50, 313–323 (2011). https://doi.org/10.1007/s00411-010-0349-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00411-010-0349-2