Abstract
Introduction
Obstructive sleep apnoea (OSA) is characterised by a low-grade systemic and airway inflammation; however, the regulatory mechanisms of inflammation are poorly explored. Survivin (Birc5) is an anti-apoptotic protein which inhibits Type 1 inflammation; however, this molecule has not been investigated in OSA.
Methods
Forty-five patients with OSA and 31 non-OSA control subjects were involved. Venous blood was collected for plasma survivin measurements before and after diagnostic overnight polysomnography. Plasma survivin levels were compared between the two groups and correlated to OSA severity and comorbidities.
Results
Plasma survivin levels were lower in OSA in the evening (27.6 ± 89.9 vs. 108.3 ± 161.2 pg/ml, p < 0.01) and in the morning (17.4 ± 48.6 vs. 36.4 ± 69.2 pg/ml, p = 0.02) compared to the control group. This OSA-related decrease was also present when only the non-obese patients were analysed. Significant indirect relationships were observed between plasma survivin levels and measures of OSA severity such as the apnoea–hypopnoea index (r = − 0.45) or oxygen desaturation index (r = − 0.40, both p < 0.01); however, when adjusting to BMI, these became insignificant (p > 0.05). Low plasma survivin concentrations were associated with high BMI (r = − 0.35), high CRP (r = − 0.31), low HDL cholesterol (r = 0.24) and high triglyceride levels (r = − 0.24, all p < 0.05).
Conclusion
Plasma survivin levels are reduced in OSA, relate to disease severity, and are associated with high CRP levels. This suggests an impaired immunoregulation in this disorder which needs to be studied in further detail.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnoea (OSA) is a common disorder which is characterised by the partial or complete collapse of the upper airways during sleep, subsequent intermittent hypoxia and fragmented hypnogram. OSA is also accompanied by a low-grade systemic inflammation, which is reflected by the elevation of circulating pro-inflammatory mediators, such as C-reactive protein (CRP), tumour necrosis factor alpha (TNF-α), interleukin 6 (IL-6) [1], IL-33, pentraxin [2] or complement factors [3]. On the contrary, mechanisms which regulate systemic inflammation in OSA are poorly described. Previous studies reported lower levels of immunosuppressive IL-10 [4], transforming growth factor beta (TGF-β) [5] and vitamin D [6], suggesting that impaired immunoregulation may contribute to enhanced inflammation.
Obstructive sleep apnoea is characterised by the disturbed diurnal rhythm of several inflammatory molecules [7,8,9] and the magnitude of these perturbations may relate to disease severity [8]. Therefore, for a better understanding and not to miss relevant alterations, mediators of interest need to be checked at various time points. This approach is important for methodological considerations, namely when to sample. Secondly, acute effects of sleep on biomarkers can be monitored. However, this has been performed only in the minority of the studies.
Baculoviral IAP Repeat Containing 5 (Birc5), commonly known as survivin, is a member of the inhibitor-of-apoptosis family which inhibits the caspase-regulated apoptotic pathway. For brevity, we will henceforth refer to Birc5/survivin as survivin. This molecule is essential in physiological embryogenesis [10] and is involved in fibrinolysis by inducing the expression of urokinase [11]. It is also responsible for physiological leukocyte development, haematopoiesis and vasculogenesis, is required for hepatocyte and neuronal survival [12] and has a complex immunoregulatory role. Survivin promotes the differentiation of T cells towards Th2 line and enhances the production of some type 2 cytokines, including IL-4 and IL-13 [13]. It decreases the number and suppresses the function of CD8 + T cells, skewing immunity towards the Th2 direction, but not altering the regulatory T cell and Th17 ratios [13]. In addition, IFN-γ and IL-2 levels are decreased, while IL-4 and IL-13 concentrations are increased in the presence of survivin [13]. In line with this, altered survivin levels were reported in chronic inflammatory diseases such as rheumatoid arthritis, psoriasis, systemic sclerosis, inflammatory bowel diseases [14] or bronchial asthma [15]. It is also overexpressed in various malignancies, including lung cancer, prostate, gastric, colon, bladder and oesophageal carcinomas, osteosarcomas and lymphomas [16].
Survivin has not been investigated in OSA before, despite the fact that it may play a pivotal role in immunoregulation. Therefore, the aim of this study was to analyse plasma survivin levels in OSA, investigate evening to morning changes and compare them to disease severity.
Methods
Study Subjects and Design
Forty-five Caucasian patients with OSA (60 ± 11 years) and 31 non-OSA control volunteers (53 ± 16 years) were included in the study. Patients with diagnosed malignant or autoimmune disorder were excluded and none of the subjects had an infection within 4 weeks prior to the study. OSA was newly diagnosed and none of the patients had used continuous positive airway pressure, a mandibular advancement device, or had surgery against OSA before the study. Based on apnoea–hypopnoea index (AHI), subjects with OSA were divided into mild (n = 15, AHI of 5–14.9/h), moderate (n = 14, AHI of 15–29.9/h), and severe (n = 16, AHI of ≥ 30/h) groups. None of the volunteers had daytime hypoxemia but 14 patients with OSA had nocturnal hypoxaemia (total sleep time with saturation below 90%, TST90% > 10%).
For all participants medical history was taken, blood pressure was measured, venous blood was collected into EDTA tubes, and the Epworth Sleepiness Scale (ESS) was self-completed in the evening (7–8 p.m.). This was followed by attended overnight polysomnography. Blood collection for plasma survivin, serum glucose, total cholesterol, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglyceride, CRP and creatinine measurements was repeated under fasting conditions and before taking medications the following morning (7–8 a.m.). Glomerular filtration rate (GFR) was estimated using the Modification of Diet in Renal Disease equation \(\left( {{\text{GFR}}~({\text{mL/min/}}1.73~{{\text{m}}^2})=175 \times {{({\text{serum~creatinine}})}^{ - 1.154}} \times {{({\text{Age}})}^{ - 0.203}}( \times \,0.742~{\text{if}}~{\text{female}})} \right)\).
The study was approved by the Scientific Research Ethics Committee (Semmelweis University TUKEB, 30/2014), and patients gave their informed consent.
Polysomnography
Polysomnography was performed using Somnoscreen Plus Tele PSG (Somnomedics GmbH, Germany) as was described previously [8, 9, 17] and according to the American Academy of Sleep Medicine guidelines [18]. Total sleep time (TST), sleep period time (SPT), AHI, oxygen desaturation index (ODI), TST90%, minimal saturation (minSat) and arousal index (AI) were registered and used as indices for OSA severity.
Plasma Survivin Measurements
Plasma survivin levels were determined as described previously [19]. After collection, EDTA tubes were processed within 2 h and centrifuged at 1500 RPM and 4 °C. Plasma was separated and stored at − 70 °C until analysis. Commercially available ELISA kits (DSV00, R&D Systems, Abingdon, UK) were used for survivin measurements. The detection limit was 4.44 pg/ml, as it was reported by the manufacturer. The intra-assay coefficient of variation estimated by 152 parallel measurements was 19%. Plasma survivin levels were measured in duplicates and their average was used.
Statistical Analyses
Statistical analyses were carried out with GraphPad Prism 5.0 (GraphPad Software Inc., San Diego, CA, USA). The normality of the data was assessed using the Kolmogorov–Smirnov test. Clinical characteristics were compared using the t test, Mann–Whitney and Chi-square tests between the OSA and control groups. Plasma survivin was compared between the two groups with the Mann–Whitney test at each time point. The Wilcoxon test was used to investigate evening to morning changes in plasma survivin levels. Survivin concentrations were correlated to clinical and demographic variables using the Spearman test. Plasma survivin levels were compared along OSA severities with the Kruskal–Wallis test followed by Dunn’s test. The effect of BMI as a co-variate was investigated with the general mixed linear model. The OSA group was divided into obese (BMI ≥ 30 kg/m2, n = 21) and non-obese (BMI < 30 kg/m2, n = 24) groups and plasma survivin concentrations were compared to those of non-obese controls (n = 30) with the Kruskal–Wallis test followed by Dunn’s test. Patients with OSA were also divided into hypoxemic (n = 14) and non-hypoxemic (n = 31) subgroups which were compared with the Mann–Whitney test.
The sample size was estimated to detect the differences in plasma survivin concentrations between the groups, with an effect size of 0.65 and a power of 0.80 [20]. This effect size was based on intra-assay variability of survivin measurements and variation of plasma survivin values in healthy subjects [19]. A p value < 0.05 was considered significant.
Results
Comparison of OSA and Control Groups
Subjects’ characteristics are summarised in Table 1. In general, patients with OSA were older, had higher weight, BMI, systolic blood pressure and serum CRP, and lower GFR, total cholesterol and HDL-C levels (all p < 0.05). In addition, the proportion of both males, and patients with hypertension, was higher in OSA (both p < 0.05), while no difference was observed in the prevalence of smoking or diabetes. There was no difference in fasting blood glucose, LDL-C or triglyceride concentrations, but diastolic blood pressure tended to be higher in OSA (p = 0.06). Regarding the sleep study, patients with OSA had higher AHI, ODI and TST90%, and lower MinSat (all p < 0.01). They also tended to have longer SPT (p = 0.08), while there was no difference in ESS, TST or AI (all p > 0.05).
Comparison of Plasma Survivin Levels Between the Groups and Its Correlations with Clinical Variables
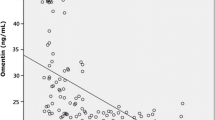
Plasma survivin was lower in OSA in the evening (27.6 ± 89.9 vs. 108.3 ± 161.2 pg/ml, p < 0.01, OSA and controls, respectively) and in the morning (17.4 ± 48.6 vs. 36.4 ± 69.2 pg/ml, p = 0.02). There was no change in the evening to morning plasma survivin concentrations in OSA (p = 0.79); however, morning plasma survivin levels were decreased in controls compared to the evening concentrations (p < 0.01, Fig. 1). Comparing plasma survivin levels to subjects’ characteristics and clinical variables, we found a direct relationship with HDL-C (r = 0.24, p = 0.04) and MinSat (r = 0.26, p = 0.04), as well as indirect relationships with weight (r = − 0.42, p < 0.01), BMI (r = − 0.35, p < 0.01), CRP (r = − 0.31, p < 0.01), triglyceride (r = − 0.23, p = 0.04), AHI (r = − 0.45, p < 0.01), ODI (r = − 0.40, p < 0.01) and TST90% (r = − 0.33, p = 0.01). There was no relationship between plasma survivin concentration and age, the presence of hypertension, diabetes or smoking, the levels of fasting blood glucose, total cholesterol or LDL-C, TST, SPT or AI (all p > 0.05).
Evening and morning plasma survivin levels in OSA and controls. Plasma survivin concentration was significantly lower in OSA in the evening (*p < 0.05) and in the morning (*p < 0.05). Plasma survivin levels significantly decreased from evening to morning in controls (*p < 0.05) without any difference in OSA (p = 0.79)
Plasma Survivin Levels Along Disease Severities
There was a significant difference among different severity subgroups both in the evening (p = 0.01, Fig. 2a) and in the morning (p = 0.04, Fig. 2b), with a significant difference between the control and severe subgroups (p < 0.05 at both time points). When analysing only non-obese subjects (n = 30 control, n = 13 mild, n = 6 moderate, n = 5 severe), the four groups were still significantly different in the morning (p = 0.04) and tended to be different in the evening (p = 0.05). BMI increased progressively along OSA severities (25.4 ± 3.6, 26.8 ± 3.0, 31.5 ± 7.8 and 34.6 ± 5.3 kg/m2, controls, mild, moderate and severe, respectively, p < 0.01). When adjusting the disease severity–plasma survivin model to BMI, the difference in plasma survivin concentrations between the four subgroups became insignificant (p > 0.05 at both time points).
The Effect of Obesity
There was a significant difference in plasma survivin levels among the three groups of subjects (non-obese controls, non-obese patients with OSA and obese patients with OSA, p < 0.01, Fig. 3). Compared to controls (119.7 ± 172.9 pg/ml) both non-obese (27.2 ± 94.9 pg/ml) and obese (28.2 ± 85.9 pg/ml) patients had lower survivin levels (both p < 0.05), while there was no difference between the obese and non-obese patients with OSA (p > 0.05).
Survivin Levels in Hypoxemic and Non-hypoxemic Patients with OSA
There was no difference between the survivin levels measured in hypoxemic (2.2 ± 7.7 pg/ml) and non-hypoxemic patients (39.1 ± 106.7 pg/ml, p = 0.17) in the evening; however, morning survivin levels of hypoxemic patients tended to be lower (0.4 ± 1.2 vs. 25.1 ± 7.2, pg/ml, p = 0.05). Of note, OSA was more severe in patients with nocturnal hypoxemia (AHI of 45.8 ± 26.5/h vs. 19.7 ± 12.8/h, p < 0.01, hypoxic vs. non-hypoxemic groups, respectively).
Discussion
We investigated circulating survivin levels in obstructive sleep apnoea for the first time. We found reduced plasma survivin concentrations in OSA suggesting impaired immunoregulation in this disorder.
Although it has primarily been investigated in cancers, survivin is also produced in normal cell types, including lymphocytes, neutrophils, hepatocytes, arterial smooth muscle cells, epithelial cells, neuronal cells, endometrial cells, oocytes and spermatocytes [12]. In cancer, it is actively released by malignant cells to suppress the anti-cancer inflammatory response [16]. However, it is not clear whether the circulating protein levels detected in physiological circumstances reflect active release or destruction of the parent cells. Nevertheless, survivin has been detected in peripheral blood, although in very low concentrations [19, 21,22,23,24].
The exact reason for the OSA-related reduction of circulating survivin is not clear. It is known that chronic hypoxia induces survivin expression in cancer and endothelial cells in vitro [12]; however, the association between markers of hypoxia and survivin expression in cancer has not been confirmed in vivo [25]. Only one Chinese study has examined the effect of intermittent hypoxia on hippocampal survivin production and found a significant increase in rats [26]. In contrast, in an ischaemia–reperfusion model resembling intermittent hypoxia, survivin expression reduced in liver tissue following ischaemia [27]. Our results showing that survivin levels are inversely related to markers of intermittent hypoxia are in line with the latter study. The lack of relationship with sleep duration or arousal index suggests that hypoxia rather than fragmented sleep reduces survivin production in OSA.
Reduced survivin levels may be both direct and indirect consequences of intermittent hypoxia. Intermittent hypoxia induces the production of CRP by hepatocytes via IL-6 induction [28]. It is known that CRP inhibits the expression of survivin in myocytes [29] which is in line with the current study showing an indirect relationship between CRP and survivin concentrations. In addition, it is known that TGF-β may potentiate the expression of survivin in cancer cells [30] and the production of TGF-β is decreased in OSA [5].
Apart from the enhanced systemic [1,2,3, 8] and airway [9, 31, 32] inflammation, OSA is associated with altered production of hormones, such as cortisol, insulin, aldosterone, sex hormones [33] or leptin [34]. Cortisol [35] and progesterone [36] decrease, while oestrogen [37] and leptin [38] increase survivin gene expression. As the levels of cortisol and leptin are elevated, while oestrogen or progesterone concentrations are decreased in OSA [33], the effect of hormones on survivin production in sleep apnoea are contradictory. Therefore, parallel measurement of circulating survivin and hormones are warranted in the future.
The reduced survivin levels observed in OSA may have a pathophysiological role. On one hand, survivin has an immunoregulatory role by decreasing CD8 cells and skewing T helper lymphocytes towards Th2. Hence, decreased survivin may contribute towards the increased CD8 prevalence [39] and activation [40], as well as Th1:Th2 ratio [41] seen in OSA. On the other hand, survivin is involved in the coagulation cascade via inducing the production of urokinase [11] of which concentrations were reduced in OSA [5].
Interestingly, we found a significant overnight change in plasma survivin levels only in controls. Physiologically, cortisol is produced during the latter stages of sleep [42], which is frequently disturbed in OSA. Glucocorticoids down-regulate survivin expression [35] which may explain evening to morning reduction in controls. The lack of change in survivin concentrations seen in OSA may be explained by dysregulated sleep. However, as the levels of survivin in OSA were close to the limit of detection, such alterations may not be captured due to methodological factors.
Around 70% of patients with OSA are obese [43], with 40–50% of obese people suffering from OSA [44]. Obesity itself may trigger systemic inflammation and may aggravate OSA-induced inflammatory alterations [28]. Because obesity is a frequent cofounder in OSA, it is often hard to distinguish OSA- or obesity-induced changes in human studies [28]. To avoid the effect of obesity, subjects with OSA were divided into obese and non-obese subgroups. We did not observe a significant difference between the two OSA subgroups, while survivin levels were significantly reduced in OSA irrespective of obesity, compared to the controls. This suggests that the observed differences are related to OSA and not obesity. However, when adjusting to the BMI, the association between survivin concentrations and OSA severity became insignificant, suggesting that BMI is a major cofactor. Of note, the study was not powered to analyse subgroups or the independence of the relationship between disease severity and survivin levels from covariates.
None of the subjects had received any specific therapy against OSA prior to the study, which enabled us to avoid the obvious bias from the treatment. Continuous positive airway pressure therapy is highly effective in reducing AHI, but its effect on systemic inflammation is contradictory [28]. Therefore, although a potentially significant change after therapy would support our findings [8], negative results would not exclude the casual relationship between OSA and systemic inflammation [45]. Of note, the current study could serve as a potential source for power calculations in designing an interventional trial on inflammatory molecules in OSA. The effect of treatment on markers of inflammation should be investigated in further trials.
We found a significant relationship between circulating survivin levels and serum lipid concentrations, suggesting that this molecule could be associated with dyslipidaemia. As dyslipidaemia is related to OSA [46], the independence of the survivin–lipid associations should be investigated in a specifically designed broader cohort which would consider OSA as a cofounder.
In summary, plasma survivin levels are decreased in OSA and relate to disease severity. Chronic intermittent hypoxia, rather than fragmented sleep, is responsible for these changes. Although our study implicates impaired immunoregulation in OSA, this needs to be investigated in detail in further studies.
References
Nadeem R, Molnar J, Madbouly EM, Nida M, Aggarwal S, Sajid H, Naseem J, Loomba R (2013) Serum inflammatory markers in obstructive sleep apnea: a meta-analysis. J Clin Sleep Med JCSM: Off Publ Am Acad Sleep Med 9(10):1003–1012. https://doi.org/10.5664/jcsm.3070
Sozer V, Kutnu M, Atahan E, Caliskaner Ozturk B, Hysi E, Cabuk C, Musellim B, Simsek G, Uzun H (2018) Changes in inflammatory mediators as a result of intermittent hypoxia in obstructive sleep apnea syndrome. Clin Respir J 12(4):1615–1622. https://doi.org/10.1111/crj.12718
Horvath P, Tarnoki DL, Tarnoki AD, Karlinger K, Lazar Z, Losonczy G, Kunos L, Bikov A (2018) Complement system activation in obstructive sleep apnea. J Sleep Res. https://doi.org/10.1111/jsr.12674
Leon-Cabrera S, Arana-Lechuga Y, Esqueda-Leon E, Teran-Perez G, Gonzalez-Chavez A, Escobedo G, Velazquez Moctezuma J (2015) Reduced systemic levels of IL-10 are associated with the severity of obstructive sleep apnea and insulin resistance in morbidly obese humans. Mediat Inflamm 2015:493409. https://doi.org/10.1155/2015/493409
Steffanina A, Proietti L, Antonaglia C, Palange P, Angelici E, Canipari R (2015) The plasminogen system and transforming growth factor-beta in subjects with obstructive sleep apnea syndrome: effects of CPAP treatment. Respir Care 60(11):1643–1651. https://doi.org/10.4187/respcare.03571
Kheirandish-Gozal L, Peris E, Gozal D (2014) Vitamin D levels and obstructive sleep apnoea in children. Sleep Med 15(4):459–463. https://doi.org/10.1016/j.sleep.2013.12.009
Entzian P, Linnemann K, Schlaak M, Zabel P (1996) Obstructive sleep apnea syndrome and circadian rhythms of hormones and cytokines. Am J Respir Crit Care Med 153(3):1080–1086. https://doi.org/10.1164/ajrccm.153.3.8630548
Bikov A, Kunos L, Pallinger E, Lazar Z, Kis A, Horvath G, Losonczy G, Komlosi ZI (2017) Diurnal variation of circulating microvesicles is associated with the severity of obstructive sleep apnoea. Sleep Breath 21(3):595–600. https://doi.org/10.1007/s11325-017-1464-y
Kunos L, Bikov A, Lazar Z, Korosi BZ, Benedek P, Losonczy G, Horvath I (2015) Evening and morning exhaled volatile compound patterns are different in obstructive sleep apnoea assessed with electronic nose. Sleep Breath 19(1):247–253. https://doi.org/10.1007/s11325-014-1003-z
Shiozaki A, Kataoka K, Fujimura M, Yuki H, Sakai M, Saito S (2003) Survivin inhibits apoptosis in cytotrophoblasts. Placenta 24(1):65–76
Baran M, Mollers LN, Andersson S, Jonsson IM, Ekwall AK, Bjersing J, Tarkowski A, Bokarewa M (2009) Survivin is an essential mediator of arthritis interacting with urokinase signalling. J Cell Mol Med 13(9b):3797–3808. https://doi.org/10.1111/j.1582-4934.2009.00721.x
Fukuda S, Pelus LM (2006) Survivin, a cancer target with an emerging role in normal adult tissues. Mol Cancer Ther 5(5):1087–1098. https://doi.org/10.1158/1535-7163.mct-05-0375
Jutzy JM, Khan S, Asuncion-Valenzuela MM, Milford TA, Payne KJ, Wall NR (2013) Tumor-released survivin induces a type-2 t cell response and decreases cytotoxic T cell function, in vitro. Cancer Microenviron: Off J Int Cancer Microenviron Soc 6(1):57–68. https://doi.org/10.1007/s12307-012-0096-9
Gravina G, Wasen C, Garcia-Bonete MJ, Turkkila M, Erlandsson MC, Toyra Silfversward S, Brisslert M, Pullerits R, Andersson KM, Katona G, Bokarewa MI (2017) Survivin in autoimmune diseases. Autoimmun Rev 16(8):845–855. https://doi.org/10.1016/j.autrev.2017.05.016
Ungvari I, Hadadi E, Virag V, Bikov A, Nagy A, Semsei AF, Galffy G, Tamasi L, Horvath I, Szalai C (2012) Implication of BIRC5 in asthma pathogenesis. Int Immunol 24(5):293–301. https://doi.org/10.1093/intimm/dxs007
Cheung CH, Huang CC, Tsai FY, Lee JY, Cheng SM, Chang YC, Huang YC, Chen SH, Chang JY (2013) Survivin—biology and potential as a therapeutic target in oncology. OncoTargets Ther 6:1453–1462. https://doi.org/10.2147/ott.s33374
Kunos L, Lazar Z, Martinovszky F, Tarnoki AD, Tarnoki DL, Kovacs D, Forgo B, Horvath P, Losonczy G, Bikov A (2017) Overnight changes in lung function of obese patients with obstructive sleep apnoea. Lung 195(1):127–133. https://doi.org/10.1007/s00408-016-9957-1
Kushida CA, Littner MR, Morgenthaler T, Alessi CA, Bailey D, Coleman J Jr, Friedman L, Hirshkowitz M, Kapen S, Kramer M, Lee-Chiong T, Loube DL, Owens J, Pancer JP, Wise M (2005) Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep 28(4):499–521
Bikov A, Bocskei R, Eszes N, Bohacs A, Losonczy G, Rigo J, Horvath I, Tamasi L (2014) Circulating survivin levels in healthy and asthmatic pregnancy. Reprod Biol Endocrinol 12:93. https://doi.org/10.1186/1477-7827-12-93
Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41(4):1149–1160. https://doi.org/10.3758/brm.41.4.1149
Sugahara K, Uemura A, Harasawa H, Nagai H, Hirakata Y, Tomonaga M, Murata K, Sohda H, Nakagoe T, Shibasaki S, Yamada Y, Kamihira S (2004) Clinical relevance of survivin as a biomarker in neoplasms, especially in adult T-cell leukemias and acute leukemias. Int J Hematol 80(1):52–58
Yang M, Liu Y, Lu S, Wang Z, Wang R, Zi Y, Li J (2013) Analysis of the expression levels of survivin and VEGF in patients with acute lymphoblastic leukemia. Exp Ther Med 5(1):305–307. https://doi.org/10.3892/etm.2012.769
El-Attar HA, Kandil MH, El-Kerm YM, El-Ghandour MK (2010) Comparison of serum survivin and alpha fetoprotein in Egyptian patients with hepatocellular carcinoma associated with hepatitis C viral infection. Asian Pac J Cancer Prev 11(4):897–903
Bokarewa M, Lindblad S, Bokarew D, Tarkowski A (2005) Balance between survivin, a key member of the apoptosis inhibitor family, and its specific antibodies determines erosivity in rheumatoid arthritis. Arthritis Res Ther 7(2):R349–R358. https://doi.org/10.1186/ar1498
Bache M, Holzapfel D, Kappler M, Holzhausen HJ, Taubert H, Dunst J, Hansgen G (2007) Survivin protein expression and hypoxia in advanced cervical carcinoma of patients treated by radiotherapy. Gynecol Oncol 104(1):139–144. https://doi.org/10.1016/j.ygyno.2006.07.011
Wang L, Zhang P, Wang H, Yu J, Zhang M, Han X, Li L, Liu C (2015) Intermittent hypoxia promotes the expressions of rat hippocampal neuronal hypoxia-inducible factor-1 and survivin. Chin J Cell Mol Immunol 31(3):338–341
Lu QP, Cao TJ, Zhang ZY, Liu W (2004) Multiple gene differential expression patterns in human ischemic liver: safe limit of warm ischemic time. World J Gastroenterol 10(14):2130–2133
Unnikrishnan D, Jun J, Polotsky V (2015) Inflammation in sleep apnea: an update. Rev Endocr Metab Disord 16(1):25–34. https://doi.org/10.1007/s11154-014-9304-x
Lee BS, Kim SH, Oh J, Jin T, Choi EY, Park S, Lee SH, Chung JH, Kang SM (2014) C-reactive protein inhibits survivin expression via Akt/mTOR pathway downregulation by PTEN expression in cardiac myocytes. PLoS ONE 9(5):e98113. https://doi.org/10.1371/journal.pone.0098113
Lee J, Choi JH, Joo CK (2013) TGF-beta1 regulates cell fate during epithelial-mesenchymal transition by upregulating survivin. Cell Death Dis 4:e714. https://doi.org/10.1038/cddis.2013.244
Dragonieri S, Porcelli F, Longobardi F, Carratu P, Aliani M, Ventura VA, Tutino M, Quaranta VN, Resta O, de Gennaro G (2015) An electronic nose in the discrimination of obese patients with and without obstructive sleep apnoea. J Breath Res 9(2):026005. https://doi.org/10.1088/1752-7155/9/2/026005
Dragonieri S, Quaranta VN, Carratu P, Ranieri T, Resta O (2016) Exhaled breath profiling in patients with COPD and OSA overlap syndrome: a pilot study. J Breath Res 10(4):041001. https://doi.org/10.1088/1752-7155/10/4/041001
Ruchala M, Brominska B, Cyranska-Chyrek E, Kuznar-Kaminska B, Kostrzewska M, Batura-Gabryel H (2017) Obstructive sleep apnea and hormones—a novel insight. Arch Med Sci 13(4):875–884. https://doi.org/10.5114/aoms.2016.61499
Pan W, Kastin AJ (2014) Leptin: a biomarker for sleep disorders? Sleep Med Rev 18(3):283–290. https://doi.org/10.1016/j.smrv.2013.07.003
He L, Liu YP, Hou KZ, Li D, Zhu ZT, Zhang JD (2006) Expression of survivin gene in apoptosis induced by dexamethasone in CEM cells. Chin J Contemp Pediatr 8(3):173–176
Formby B, Wiley TS (1999) Bcl-2, survivin and variant CD44 v7-v10 are downregulated and p53 is upregulated in breast cancer cells by progesterone: inhibition of cell growth and induction of apoptosis. Mol Cell Biochem 202(1–2):53–61
Nabilsi NH, Broaddus RR, McCampbell AS, Lu KH, Lynch HT, Chen LM, Loose DS (2010) Sex hormone regulation of survivin gene expression. J Endocrinol 207(2):237–243. https://doi.org/10.1677/joe-10-0128
Jiang H, Yu J, Guo H, Song H, Chen S (2008) Upregulation of survivin by leptin/STAT3 signaling in MCF-7 cells. Biochem Biophys Res Commun 368(1):1–5. https://doi.org/10.1016/j.bbrc.2007.04.004
Domagala-Kulawik J, Osinska I, Piechuta A, Bielicki P, Skirecki T (2015) T, B, and NKT cells in systemic inflammation in obstructive sleep apnoea. Mediat Inflamm 2015:161579. https://doi.org/10.1155/2015/161579
Dyugovskaya L, Lavie P, Lavie L (2005) Lymphocyte activation as a possible measure of atherosclerotic risk in patients with sleep apnea. Ann N Y Acad Sci 1051:340–350. https://doi.org/10.1196/annals.1361.076
Tan HL, Gozal D, Wang Y, Bandla HP, Bhattacharjee R, Kulkarni R, Kheirandish-Gozal L (2013) Alterations in circulating T-cell lymphocyte populations in children with obstructive sleep apnea. Sleep 36(6):913–922. https://doi.org/10.5665/sleep.2724
Takahashi Y, Kipnis DM, Daughaday WH (1968) Growth hormone secretion during sleep. J Clin Investig 47(9):2079–2090. https://doi.org/10.1172/jci105893
Romero-Corral A, Caples SM, Lopez-Jimenez F, Somers VK (2010) Interactions between obesity and obstructive sleep apnea: implications for treatment. Chest 137(3):711–719. https://doi.org/10.1378/chest.09-0360
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9):1006–1014. https://doi.org/10.1093/aje/kws342
Stradling JR, Craig SE, Kohler M, Nicoll D, Ayers L, Nunn AJ, Bratton DJ (2015) Markers of inflammation: data from the MOSAIC randomised trial of CPAP for minimally symptomatic OSA. Thorax 70(2):181–182. https://doi.org/10.1136/thoraxjnl-2014-205958
Roche F, Sforza E, Pichot V, Maudoux D, Garcin A, Celle S, Picard-Kossovsky M, Gaspoz JM, Barthelemy JC (2009) Obstructive sleep apnoea/hypopnea influences high-density lipoprotein cholesterol in the elderly. Sleep Med 10(8):882–886. https://doi.org/10.1016/j.sleep.2008.07.017
Acknowledgements
The study was supported by the Hungarian Respiratory Society (Andras Bikov, Peter Horvath and David Laszlo Tarnoki) and Semmelweis University (Laszlo Kunos). The authors are also grateful to the Elektro-Oxigén Inc. for providing the polysomnographic devices. This publication was supported by the Janos Bolyai Research Scholarship of the Hungarian Academy of Sciences to Andras Bikov. The authors are grateful to Mrs. Monika Banlaky for her technical assistance with PSG, Victoria Dean for English corrections, as well as Bianka Forgo, Luca Fesus, Fruzsina Martinovszky and Daniel Kovacs for their assistance in data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kunos, L., Horvath, P., Kis, A. et al. Circulating Survivin Levels in Obstructive Sleep Apnoea. Lung 196, 417–424 (2018). https://doi.org/10.1007/s00408-018-0120-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-018-0120-z