Abstract
The aim of this study was to compare serum insulin-like growth factor (IGF-1) levels in patients with obstructive sleep apnea syndrome (OSAS) with those of nonapneic controls and to determine the risk factors of low IGF-1 levels in patients with OSAS. The study included 39 newly diagnosed moderate-to-severe OSAS patients and 36 nonapneic controls. Overnight polysomnography (PSG) was performed in all patients. The circulating levels of IGF-1 in the OSAS group were significantly lower than those of the control group (p < 0.05). There was a significant negative correlation between IGF-1 and logarithmic transformation (Ln) of the apnea-hypopnea index (AHI), duration of apnea-hypopnea, arousal index, average desaturation, and oxygen desaturation index (ODI). The result of stepwise regression analyses showed that OSAS (p = 0.001) was a risk factor for a low IGF-1 level, independent of age, gender, and body mass index (BMI). Our findings demonstrated that there was a significant negative correlation between IGF-1 and Ln AHI and that OSAS reduced the circulating levels of IGF-1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea syndrome (OSAS) is defined as repeated episodes of upper airway occlusion during sleep with consequent excessive daytime sleepiness. These episodes are often accompanied by nocturnal intermittent hypoxia and repetitive action of the sympathetic nervous system. The prevalence of OSAS in adults aged 20–100 years was reported in a community-based study as 3.9% in males and 1.2% in females [1, 2]. Obesity increases the risk of OSAS developing by approximately tenfold from a range of 2–4% in the general adult population up to 20–40% in those with a body mass index (BMI) > 30 [3].
Growth hormone (GH) stimulates the synthesis of insulin-like growth factor-1 (IGF-1) in the liver and in other target tissues. IGF-1 is considered to be the main mediator of the growth-promoting actions of GH [4]. Circulating concentrations of IGF-1 and IGF-binding protein-3 (IGFBP-3) are strongly related to diurnal GH secretion, reflecting mean daily GH levels, and seem to correlate well with physiologic changes in GH secretion [5]. GH secretion is affected by age, gender, obesity, food intake, blood glucose, serum free fatty acids, body composition, and sleep quality [6, 7]. Oxygen content of inspirated air appears to contribute to the secretion of GH and IGF-1. Chronic hypoxemia is associated with a decrease in IGF-1 without any changes observed in GH [8, 9]. Furthermore, recent studies suggest that the IGF system is involved in the development of cardiovascular disease [10].
In the present study we hypothesized that OSAS might reduce serum IGF-1 level, regardless of age, gender, and obesity, and that it might result in the development of cardiovascular diseases. To investigate this hypothesis, we compared serum IGF-1 levels of OSAS patients and nonapneic controls.
Materials and Methods
Patients
Seventy-seven consecutive patients referred for polysomnographic evaluation of suspected OSAS were recruited for participation in the study. Premenopausal women who used estrogen or insulin were excluded from this study. Seventy-five (39 newly diagnosed moderate-to-severe OSAS patients and 36 non-apneic controls) of 77 eligible patients met the inclusion criteria for enrollment. There were 3 patients with diabetes, 12 patients with hypertension, and 4 patients with cardiac disease in OSAS patients and 3 patients with diabetes, 9 patients with hypertension, 1 patient with cardiac disease in the nonapneic controls. There were no significant differences for diabet, hypertension, cardiac disease between the two groups. In addition to the Epworth Sleepiness Scale (ESS), a questionnaire was administered to each patient in the presence of their sleeping partner which inquired about a history of snoring, witnessed apnea, and excessive daytime sleepiness. Demographic information (age, gender, and smoking habits) and anthropometric measurements (height, weight, and BMI [weight/height kg/m2]) were obtained upon presentation to the sleep center. None of the subjects had cancer or pulmonary or neuromuscular disease.
The Ethics Committee of Uludag University approved the study protocol and all patients gave written informed consent to participate.
Sleep Study
Overnight polysomnography (PSG) was performed in all patients using a Compumedics Sleepwatch System (Compumedics P-series, Compumedics, Melbourne, Australia). All participants reported to the sleep laboratory at approximately 8:30 p.m. and PSG was initiated at approximately 10:30 p.m. Polysomnographic recordings included two electroencephalography (EEG) channels (C3/A2 and O2/A1), two electro-oculogram (EOG) channels, one submental electromyogram (EMG) channel, and one electrocardiography (ECG) channel. Ventilatory monitoring included recordings of oronasal airflow (with an oronasal thermistor), hemoglobin oxygen saturation by pulse oximetry (SaO2 was measured via a finger oximeter), respiratory chest movement (with inductive plethysmography), and abdomen and body position.
Sleep staging was performed according to the standard criteria of Rechtschaffen and Kales [11]. To assess ventilation during sleep, nasal airflow was carefully analyzed. Apnea was defined as an episode of airflow cessation lasting at least 10 s. Hypopnea was defined as an episode lasting at least 10 s with reductions of thermistor signal amplitude of least 50% and an associated fall of at least 3% in oxygen saturation, or an arousal. The sums of apnea and hypopnea episodes were divided by the total sleep time to obtain the apnea-hypopnea index (AHI). Patients with AHI ≥ 5 were considered to have OSAS. Subjects with AHI < 5 were included in the control group.
Circulating IGF-1 Assay
Single blood samples were drawn between 8:00 a.m. and 9:00 a.m. following the sleep study. Subjects were required to be fasting when blood was collected. The blood samples were centrifuged, 1 h after they were drawn, at 3000g at 4°C for 10 min. Serum samples were stored at −70°C until assay. Serum IGF-1 was measured using a solid-phase chemiluminescent enzyme immunoassay system (Immulite 2000® , Diagnostic Product Corp., Los Angeles, CA, USA) using a commercially available kit (Diagnostic Product Corp., Los Angeles, CA, USA). Samples were assayed in a single large batch and quality assessment samples were well within the manufacturers’ defined ranges.
Statistical Analysis
Statistical analysis was performed using the SPSS for Windows, v13.0 (SPSS Inc., Chicago, IL, USA). Concordance of normal distribution of all variables was calculated using the Shapiro-Wilk test before they were compared between OSAS and control groups. If the data were not normally distributed, we used nonparametric tests for dependant variables. Comparisons of data between the OSAS and control groups were performed with Student’s t test, χ2 test, and Mann-Whitney U test. A logarithmic transformation (ln) of AHI and average oxygen desaturation were used to achieve a normal distribution of residuals. We performed stepwise regression analysis to identify significant relationships between sleep disorder parameters and IGF-1. The results are expressed as mean ± SD. A value of p < 0.05 was considered statistically significant.
Results
Baseline characteristics of the OSAS and control groups are shown Table 1. There was no significant difference in age, gender, BMI, smoking habit, snoring, hypertension, and coronary heart disease between the two groups. There were 25 (64.1%) subjects in the OSAS group and 17 (47.2%) subjects in the control group who had BMI ≥ 30 kg/m2. In the OSAS group, excessive daytime sleepiness and ESS score were significantly higher than those of the control group (p < 0.001).
Polysomnographic characteristics of the OSAS and control groups are summarized in Table 2. There were no significant differences in the total sleeping time, sleep efficiency, and baseline oxygen saturation between the two groups. Significant differences in sleep stages 3 and 4, arousal (per h), AHI, duration of apnea-hypopnea, average oxygen saturation during sleep, average oxygen desaturation, and oxygen desaturation index (ODI) were observed when the OSAS group was compared to control group (p < 0.001).
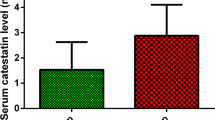
The circulating levels of IGF-1 in the OSAS group (89.8 ± 39.2 ng/ml) were significantly lower than those of the control group (140.1 ± 54.5 ng/m) (p < 0.001). There was a significant negative correlation between IGF-1 and ln AHI (r = −0.42, p < 0.001) (Fig. 1). A negative correlation was also noted between IGF-1 and the duration of apnea-hypopnea (r = −0.36, p < 0.001), arousal index (r = −0.23, p < 0.05), average desaturation (r = −0.29, p < 0.05) (Fig. 2), and oxygen desaturation index (ODI) (r =−0.224, p < 0.05). There was no significant correlation between IGF-1 and REM or slow-wave sleep.
The result of stepwise regression analyses [IGF-1 = gender (22.03) – age (0.427) – BMI (0.691) + AHI (0.727), r 2 = 0.232, p = 0.001] showed that AHI (p= 0.001) was a risk factor for low IGF-1, independent of age, gender, and BMI.
Discussion
The results of the present study demonstrated that the circulating levels of IGF-1 in the OSAS group were significantly lower than those of the control group. There was a significant negative correlation between IGF-1 and AHI, and OSAS was a risk factor for a low level of IGF-1, regardless of obesity.
Some studies suggest that OSAS patients have low GH and IGF-1 levels without any specific causes of GH deficiency. Xu et al. [12] reported that serum IGF-1 levels of patients with OSAS were significantly lower than those of the controls. McArdle et al. [13] indicated that patients with OSA had higher 24-h and nocturnal (12-h) urinary norepinephrine excretion and plasma leptin levels and lower IGF-1 levels. Multiple linear regression, adjusting for central obesity, age, and alcohol consumption, confirmed an independent association between OSA and metabolic risks, with a trend for IGF-1. Gianotti et al. [14] studied the GH response to GHRH plus arginine and the IGF-1 and IGF-binding protein-3 responses to very-low-dose recombinant human (rh) GH treatment in OSAS patients, simple obese, and normal subjects. Basal IGF-1 levels in OSAS patients were lower than in obese and normal subjects. As opposed to obese and normal subjects, in OSAS patients a very low level of rhGH did not affect IGF-1. They suggested that OSAS is connoted by a concomitant impairment of GH secretion and sensitivity. In our study circulating levels of IGF-1 in the OSAS group were significantly lower those of the control group.
Several studies have demonstrated that GH synthesis and secretion are reduced in the presence of obesity [7], whereas the influence of the latter on peripheral IGF-1 levels is controversial, with reports of increased, normal, or even low levels [7, 15]. For each 1.5-kg/m2 increase in BMI, there is a 50% decrease in the 24-h secretion of GH [16]. Maccario et al. [17] investigated IGF-1 concentrations in 286 obese people and 326 age-matched controls. They showed that IGF-1 concentrations were inversely and independently related to age and BMI. A recent cross-sectional study confirmed that IGF-1 levels are lower in obese women compared to nonobese women and are inversely related to central adiposity [18]. There is a strong correlation between obesity and OSAS. Young et al. [19] reported that every 6-kg/m2 increase in BMI increases OSAS risk more than fourfold, and approximately 70% of OSAS patients are obese. Low levels of IGF-1 in OSAS patients may be related to accompanying obesity. However, in the present study we showed that OSAS (p = 0.001) was a risk factor for low IGF-1, independent of age, gender, and BMI, according to the stepwise logistic regression analysis.
GH secretion occurs mostly during sleep, and 70% of nocturnal GH pulses are associated with slow-wave sleep [20]. In OSAS, GH and IGF-1 secretion are decreased due to sleep fragmentation, which decreases the amount of slow-wave sleep. Not only sleep fragmentation, but also repetitive hypoxemia can reduce IGF-1 secretion in OSAS. Oxygen content of breathing air appears to contribute to the secretion of IGF-1. Chronic hypoxemia may reduce the IGF-1 level without any changes observed in GH [8, 9]. However, repetitive hypoxemia may affect GH and IGF-1 secretion. In animal, hypoxia inhibits GH release or biosynthesis [21]. Hyperoxia increases the expression of IGF-1 and its type I receptors in rats [22]. In the present study a negative correlation was noted between IGF-1 and AHI, duration in apnea-hypopnea, arousal index, average desaturation, and oxygen desaturation index (ODI).
Nasal continuous positive airway pressure (CPAP) is the most efficient therapy for maintaining upper-airway patency during sleep. Its efficacy to control sleep apnea and hypopnea starts the very first night of the therapy. CPAP treatment improves sleep architecture and oxygen saturation [23]. It increases GH [24] and IGF-1 [25] secretion. Lindberg et al. [26] reported that after 3 weeks of CPAP therapy there was a reduction in fasting serum insulin, decrease in insulin resistance, and an increase in IGF-1.
A greater risk of coronary artery disease in OSAS patients is suggested by several retrospective and cross-sectional studies. The prevalence of OSAS was 37% in men and 30% in women with angiographically verified coronary artery disease [27, 28]. Mechanisms to explain this relationship have included sympathetic nervous system activation and systemic endothelial dysfunction [29]. Low levels of IGF-1 may contribute to an increased risk for cardiovascular disease among sleep apneics. IGF-1 has endocrine, paracrine, and autocrine actions. It increases endothelial cell nitric oxide production. Low tissue IGF-1 levels have been identified in early and advanced atherosclerotic lesions, and it has been speculated that they contribute to processes leading to plaque weakening, plaque rupture, and acute coronary events [30]. Laughlin et al. [31] investigated the relationship between serum IGF-1 level and ischemic heart disease mortality in 633 men and 552 women during 9–13 years of follow-up. They concluded that low baseline levels of IGF-1 increase the risk of fatal ischemic heart disease, independent of relevant ischemic heart disease and cardiovascular risk factors. Furthermore, GH/IGF-1 axis and insulin interact at multiple levels and in diabetes mellitus the GH/IGF-1 axis is grossly disturbed, with increased secretion of GH, reduced plasma levels of IGF-1, and complex tissue-specific changes in IGF-binding proteins. It has been demonstrated that lower IGF-1 levels predict the subsequent development of impaired glucose tolerance, type 2 diabetes [32]. Poykko et al. [33] reported that there is a negative and independent association between ghrelin and IGF-1 concentrations in middle-aged subjects. The interaction between IGF-1 and ghrelin is modified by obesity, insulin resistance, and type 2 diabetes. We speculate that low IGF-1 levels may contribute to cardiovascular complications and insulin resistance in OSAS patients. Measurement of the circulating IGF-1 level may prove to be a useful marker to identify the risk of fatal ischemic heart disease in OSAS patients.
In conclusion, there was a significant negative correlation between IGF-1 and Ln AHI, and OSAS reduced circulating levels of IGF-1, independent of obesity. We believe that the negative correlation determined between obesity and IGF-1 levels in previous studies is related to OSAS present in the majority of obese patients. In accordance with the results of our study, the determination of OSAS as a risk factor independent from obesity supports the idea that low levels of IGF-1 are really dependent on OSAS in obese patients. Further studies are needed to clarify the complex relation between OSAS, obesity, cardiovascular complications, and IGF-1.
References
Hedner J, Grote L (1998) Cardiovascular consequences of obstructive sleep apnea. Eur Respir Mon 10:227–265
Bixler EO, Vgontzas AN, Lin HM, Ten Have T, Rein J, Vela-Bueno A, Kales A (2001) Prevalence of sleep disordered breathing in women; effects of gender. Am J Respir Crit Care Med 163:608–613
Kyzer S, Charuzi I (1998) Obstructive sleep apnea in the obese. World J Surg 22:998–1001
Tapanainen P, Knip M (1992) Evaluation of growth hormone secretion and treatment. Ann Med 24:237–247
Blum WF, Albertsson-Wikland K, Rosberg S, Ranke MB (1993) Serum levels of insulin like growth factor I (IGF-I) and IGF binding protein 3 reflects spontaneous growth hormone secretion. J Clin Endocrinol Metab 76:1610–1616
Engström BE, Karlsson FA, Wide L (1999) Gender differences in diurnal growth hormone and epinephrine values in young adults during ambulation. Clin Chem 45:1235–1239
Minuto F, Barreca A, Del Monte P, Fortini P, Resentini M, Morabito F, Giordano G (1988) Spontaneous growth hormone and somatomedin-C/insulin like growth factor-I secretion in obese subjects during puberty. J Endocrinol Invest 11:489–495
Bernstein D, Jasper JR, Rosenfeld RG, Hintz RL (1992) Decreased serum insulin like growth factor-I associated with growth failure in newborn lambs with experimental cyanotic heart disease. J Clin Invest 89:1128–1132
Gronfier C, Luthringer R, Follenius M, Schaltenbrand N, Macher JP, Muzet A, Brandenberger G (1996) A quantitative evaluation of the relationships between growth hormone secretion and delta wave electroencephalographic activity during normal sleep and after enrichment delta waves. Sleep 19:817–824
Bayes-Genis A, Conover CA, Schwartz RS (2000) The insulin like growth factor axis: A review of atherosclerosis and restenosis. Circ Res 86:125–130
Rechtschaffen A, Kales A (eds) (1973) A Manual of Standardized Terminology, Techniques and Scoring System for Sleep Stages of Human Subjects, 3rd ed. Los Angeles: Brain Research Institute, pp 1–13
Xu Y, Li S, Huang X, Cong B (2002) Insulin like growth factor-I and cognitive function in patients with obstructive sleep apnea syndrome. Zhonghua Yi Xue Za Zhi 82:1388–1390
McArdle N, Hillman D, Beilin L, Watts G (2007) Metabolic risk factors for vascular disease in obstructive sleep apnea: a matched controlled study. Am J Respir Crit Care Med 175:190–195
Gianotti L, Pivetti S, Lanfranco F, Tassone F, Navone F, Vittori E, Rossetto R, Gauna C, Destefanis S, Grottoli S, De Giorgi R, Gai V, Ghigo E, Maccario M (2002) Concomitant impairment of growth hormone secretion and peripheral sensitivity in obese patients with obstructive sleep apnea syndrome. J Clin Endocrinol Metab 87:5052–5057
Caufriez A, Golstein J, Lebrun P, Herchuelz A, Furlanetto R, Copinschi G (1984) Relations between immunoreactive somatomedin C, insulin and T3 patterns during fasting in obese subjects. Clin Endocrinol (Oxford) 20:65–70
Veldhuis JD, Iranmanesh A (1996) Physiologic regulation of the human growth hormone (GH)-insulin like growth factor type I (IGF-I) axis: predominant impact of age, obesity gonadal function, and sleep. Sleep 19(10 Suppl):S221–S224
Maccario M, Ramunni J, Oleandri SE, Procopio M, Grottoli S, Rossetto R, Savio P, Aimaretti G, Camanni F, Ghigo E (1999) Relatioship between IGF-I and age, gender, body mass, fat distribution, metabolic and hormonal variables in obese patients. Int J Obes Metab Disord 23:612–618
Gram IT, Norat T, Rinaldi S, Dossus L, Lukanova A, Tehard B, Clavel-Chapelon F, van Gils CH, van Noord PA, Peeters PH, Bueno-de-Mesquita HB, Nagel G, Linseisen J, Lahmann PH, Boeing H, Palli D, Sacerdote C, Panico S, Tumino R, Sieri S, Dorronsoro M, Quiros JR, Navarro CA, Barricarte A, Tormo MJ, Gonzalez CA, Overvad K, Paaske Johnsen S, Olsen A, Tjonneland A, Travis R, Allen N, Bingham S, Khaw KT, Stattin P, Trichopoulou A, Kalapothaki V, Psaltopoulou T, Casagrande C, Riboli E, Kaaks R (2006) Body mass index, waist circumference, and waist-hip ratio and serum levels of IGF-I and IGFBP-3 in European women. Int J Obes (Lond) 30:1623–1631
Young T, Shahar E, Nieto FJ, Redline S, Newman AB, Gottlieb DJ, Walsleben JA, Finn L, Enright P, Samet JM, Sleep Heart Health Study Research Group (2002) Prediction of sleep disordered breathing in community-dwelling adults: the Sleep Heart Health Study. Arch Intern Med 162:893–900
Issa FG, Sullivan CE (1986) The immediate effects of nasal continuous airway pressure treatment on sleep pattern in patients with obstructive sleep apnea syndrome. Electroencephalogr Clin Neurophysiol 63:10–17
Zhang Y-S, Du J-Z (2000) The response of growth hormone and prolactin of rats to hypoxia. Neurosci Lett 279:137–140
Han RN, Han VK, Buch S, Freeman BA, Post M, Tanswell AK (1998) Insulin-like growth factor binding proteins in air and 85% oxygen-exposed adult rat lung. Am J Physiol 274:L647–L656
Polo O, Berthon-Jones M, Douglas NJ, Sullivan CE (1994) Management of obstructive sleep apnoea/hypopnoea syndrome. Lancet 344:656–660
Grunstein RR, Handelsman DJ, Lawrence SJ, Blackwell C, Caterson ID, Sullivan CE (1989) Neuroendocrine dysfunction in sleep apnea: reversal by continuous positive airway pressure therapy. J Clin Endocrinol Metab 68:352–358
Cooper BG, White JE, Ashworth LA, Alberti KG, Gibson GJ (1995) Hormonal and metabolic profiles in subjects with obstructive sleep apnea syndrome and acute effect of continuous positive airway pressure (CPAP) treatment. Sleep 18:172–179
Lindberg E, Berne C, Elmasry A, Hedner J, Janson C (2006) CPAP treatment of a population-based sample—what are the benefits and the treatment compliance? Sleep Med 7:553–560
Mooe T, Rabben T, Wiklund U, Franklin KA, Eriksson P (1996) Sleep-disordered breathing in men with coronary artery disease. Chest 109:659–663
Mooe T, Rabben T, Wiklund U, Franklin KA, Eriksson P (1996) Sleep-disordered breathing in women: occurrence and association with coronary disease. Am J Med 101:251–256
Kraiczi H, Caidahl K, Samuelsson A, Peker Y, Hedner J (2001) Impairment of vascular endothelial function and left ventricular filling: association with the severity of apnea-induced hypoxemia during sleep. Chest 119:1085–1091
Okura Y, Brink M, Zahid AA, Anwar A, Delafontaine P (2001) Decreased expression of insulin-like growth factor-1 and apoptosis of vascular smooth muscle cells in human atherosclerotic plaque. J Mol Cell Cardiol 33:1777–1789
Laughlin GA, Barrett Connor E, Crıquı MH, Kritz-Silverstein D (2004) The prospective association of serum insulin-like growth factor I (IGF-I) and IGF-I binding protein-1 levels with all-cause and cardiovascular disease mortality in older adults: The Rancho Bernardo Study. J Clin Endocrinol Metab 89:114–120
Sandhu MS (2005) Insulin-like growth factor-I and risk of type 2 diabetes and coronary heart disease: molecular epidemiology. Endocr Dev 9:44–54
Poykko SM, Ukkola O, Kauma H, Kellokoski E, Horkko S, Kesaniemi A (2005) The negative association between plasma ghrelin and IGF-I is modified by obesity, insulin resistance and type 2 diabetes. Diabetologia 48:309–316
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ursavas, A., Karadag, M., Ilcol, Y.O. et al. Low Level of IGF-1 in Obesity May Be Related to Obstructive Sleep Apnea Syndrome. Lung 185, 309–314 (2007). https://doi.org/10.1007/s00408-007-9026-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-007-9026-x