Abstract
The aim of this study was to investigate and identify the relationship between urinary cysteinyl leukotriene E4 levels and clinical response to antileukotriene treatment in patients with asthma. Forty-eight patients with stable mild to moderate asthma were treated with montelukast in a four-week trail. Asthmatic symptom score, β2-agonist usage, percentage of eosinophil, total serum IgE concentration, forced expiratory volume in the first second (FEV1), peak expiratory flow rate (PEFR), and urinary leukotriene E4 (uLTE4) were measured before and after treatment. Clinical response was assessed by the improvement of asthma symptom scores, β2-agonist usage, and FEV1. Responders were defined as patients who had to fit the following three criteria: a reduction of more than 20% in mean symptom score; a reduction of more than 20% in β2-agonist usage, and a mean improvement of FEV1 of more than 10% from baseline value. Others were classified as nonresponders. Logistic analysis was used to access the various clinical factors correlated with the clinical response. There were 25 responders and 23 nonresponders. The mean uLTE4 level from the responders was higher than that from the nonresponders (224.5 ± 34.4 vs. 175.3 ± 37.1 pg/mg creatinine, p < 0.05). There was a significant correlation between the clinical response and the uLTE4 level but not demographic features, percentage of eosinophils, serum IgE concentration, or spirometry (p > 0.05). Subjects with a uLTE4 level of ≥ 200 pg/mg creatinine were 3.5 times more likely to respond to montelukast than those with less than 200 pg/mg creatinine (95% confidence interval [CI] = 1.7–15.8). The uLTE4 level is closely correlated with antileukotriene treatment. uLTE4 is a good biomarker for selecting this drug to treat asthma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
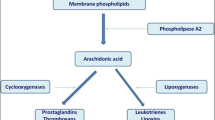
Asthma is a complex syndrome with many clinical phenotypes characterized by variable airflow obstruction, chronic airway inflammation, and bronchial hyperresponsiveness [5]. The initiation and propagation of airway inflammation arises from many factors and mediators generated by resident airway cells and recruited leukocytes. Cysteinyl leukotrienes (cysteinyl leukotriene C4, D4, E4, CysLTs) are biologically active fatty acids derived from arachidonic acid [31]. The role of CysLTs in the pathogenesis of asthma has been identified by the pleiotropic biological activities of CysLTs that mimic those features of clinic asthma; the rising level of CysLTs in plasma, urine, sputum, and bronchoalveolar lavage fluid (BALF) from patients with asthma; and the therapeutic effects of antileukotriene treatment [11, 17, 22, 24, 27]. The Global Initiative for Asthma (GINA) report has listed this class of drugs as a possible alternative to inhaled corticosteroids as the preferred therapy for adult patients with mild persistent asthma [23].
Clinical research and experience have shown that not all patients respond to this treatment and that the clinical response to those drugs is normally distributed and variable. Perhaps as many as 50% of patients may have disappointing responses [15, 30]. Some clinical studies have shown a substantial heterogeneity in individual patient response to specific antiasthma medications. Future development in asthma may result in asthma treatment that is more tailored to each patient’s response to specific medications. To our knowledge, there are still no factors that have been reliably identified to predict the clinical response, including gender, age, atopic state, serum IgE level, white blood cell (WBC) count, blood eosinophil, β2-agonists usage and inhaled corticosteroids, or CysLTs levels. If we could know the exact indication, patients would get most benefits from this class of drugs.
We postulate that the urinary leukotriene E4 (uLTE4) level, the stable metabolite of CysLTs, would have a close correlation with the therapeutic response to treatment with montelukast (Singulair, Merck & Co., Inc., Whitehouse Station, NJ). We hypothesize that those asthmatics with higher uLTE4 levels would have a better clinical response than those with lower uLTE4 levels to the treatment. To test the hypothesis, the morning urine samples were obtained from asthmatic patients before and after treatment. In particular, this study also tests the relationship between the uLTE4 levels and the magnitude of bronchoconstriction. Clinical response was assessed by the improvement of asthma symptom scores, β2agonist usage, and forced expiratory volume in the first second (FEV1).
Materials and Methods
Subjects
From December 2004 to September 2005, 61 consecutive nonsmoking patients with stable mild to moderate asthma were recruited from the outpatient pulmonary department of the Renmin Hospital, Wuhan University. The criteria for inclusion of patients in the study were as follows: (1) age between 16 and 65 years old, (2) a history of episodic dyspnea and wheezing for at least one year, (3) reversible airway obstruction characterized by an increase in FEV1 of no less than 15% after inhalation of 200 μg of albuterol, or a provocation concentration of methacholine to produce a 20% fall in FEV1 of no more than 8 mg/ml according to the standard of GINA [23], (4) no concomitant treatment with systematic corticosteroids or leukotriene modifiers, (5) no history of other pulmonary, cardiac, hepatic, or renal disease or pregnancy. Patients were excluded if they had a fever (i.e., temperature ≥ 38°C) or an unresolved upper respiratory tract infection within 3 weeks before the study. Asthma was defined as stable if none of the following occurred during the last ten days before the study: diurnal variation of more than 20% in the peak expiratory flow rate (PEFR) on 2 consecutive days; use of four or more inhalations of β2 agonists per day on 2 consecutive days; awakening due to asthma on 2 consecutive nights; or the need to use oral corticosteroids. All participants had expressed willingness and given informed, signed consents before the study. The study protocol was approved by the Renmin Hospital of Wuhan University, Ethical Committee.
Study Protocol
This study consisted of a two-week screening period and a four-week active study period. All subjects provided complete medical histories and underwent general physical examinations and baseline measurements for safety assessments entering the trial. The patients would receive a peak flowmeter and a practice diary card at the prestudy visit. The patients also would receive training of PEFR measurement manipulation and asthmatic symptom records. The record results would be assessed by the research team. Subjects recorded disease-related information daily, including β2-agonist usage and a symptom score from 0 (no symptoms) to 3 (severe symptoms) in each of the domains: shortness of breath, chest tightness, wheezing, cough, mucus production, and nocturnal awaking.
The subjects were also asked to perform PEFR (Micro/Micro plus Spirometers, Rochester, Kent, UK) in the morning upon awakening and in the evening before the evening dose of study medication throughout the study. The best of three successive values was recorded on the diary card in accordance with the technique of the manufacturer. The baseline PEFR was defined as the mean value in the morning during the last ten days of the screening period and the last day of treatment. Daily PEFR monitoring can help detect early signs of worsening before symptoms occur.
FEV1 measurement was assessed in the clinic throughout the study, achieving the reproducibility and acceptability criteria of GINA. At scheduled clinic visits and telephone contacts every week, diary cards were reviewed and FEV1 was measured. All participants continued their usual asthma treatments, including oral theophylline, inhaled β2-agonists, or inhaled corticosteroids throughout the course. The average values (asthma symptom scores, β2-agonist usage, and FEV1 results) from the last ten days of the screening period served as the baseline values. Patients were then prescribed montelukast (10 mg tablet once at bedtime) for four weeks. The average values (asthma symptom scores, β2-agonist usage, and FEV1 results) from the last ten days of the four-week treatment period served as the post-treatment values. The clinical response was evaluated from the results of symptom assessments, β2-agonist usage, and FEV1 results. Most studies have examined the effect of medications on one or more parameters of asthma, e.g., on reduction in chronic symptoms, reduction in β2-agonist usage, improvement in lung function, decrease in airway hyperresponsiveness, and improvement in the patient’s quality of life. Responders were defined as patients who had to fit the following three criteria: a reduction of more than 20% in mean symptom score, a reduction of more than 20% in β2-agonist usage, and a mean improvement of FEV1 of greater than 10% from baseline value; others were classified as nonresponders [10, 18]. The tolerability profile of this treatment was determined by adverse experience reports, physical examination, and laboratory safety tests.
Samples Collection and Analysis
The 20–30 ml urine samples were obtained by using a sterile potty at about 8:00 a.m. on the first and last day of the active medication. The samples were immediately centrifuged at 10,000g for 10 min to remove cellular debris. The supernatant was then removed, coded, and stored in aliquots of 5 ml at −70°C until analysis. The uLTE4 concentration was measured in unprocessed samples by ACETM Enzyme Immunoassay Kit according to the protocol of the manufacturer (Cayman Chemical, Ann Arbor, MI), which has been previously validated against measurements after high-performance liquid chromatography purification [19]. All measurements were done in triplicate and the mean value was calculated. The detection limit in the assay was less than 8 pg/ml. The interassay coefficient of variation was less than 10% in our laboratory. Urinary creatinine was measured using a modified Jaffe reaction method by the Dade Behring Dimension analyzer (Dade Behring, Deerfield, IL) and uLTE4 levels were expressed as pg/mg creatinine to allow corrections for diuresis variations.
All venous blood samples were obtained before the study medication. Peripheral blood counts, including differential leukocyte counts, were evaluated from the leukocyte counter measurement. Total serum IgE was assayed by the paper radioimmunosorbent technique (Pharmacia, Uppsala, Sweden) and expressed as IU/ml.
All subjects were skin-prick tested entering the study using a positive histamine control (1%), negative control (phenol/saline, 0.9%), grass mix (2.5%), cat dander (150%), dog dander (150%), cockroach (10%), mixed green pollen (20%), house dust mite (1.2%), cow’s milk (50%), egg white (6%), and Aspergillus fumigatus (5%). Prick tests were considered positive if the wheal diameter 20 min after allergen injection reached at least half the wheal diameter induced by codeine phosphate and more than the wheal diameter induced by saline. The diagnosis of atopy was allowed if at least one skin prick test from the above extracts was positive [32].
Evaluations and Statistical Analyses
After all data were collected, the Sha-Piro-Wilk test was used to test for normality and Levene’s test for homogeneity of variance. Demographic data from the two groups were compared by χ2 analysis. Clinical data before and after treatment were compared by paired t tests. Pearson coefficients of correlation between uLTE4 and percentage predicted FEV1 were computed. The data on uLTE4 were skewed, so the analysis of uLTE4 levels was performed after applying a log transformation. In this article an exploratory analysis using a logistic model was performed to study the influence of some asthmatic baseline factors on the probability of treatment response. Therefore, a binary logistic regression analysis model was used to test the correlation between the clinical factors and therapeutic response. These clinical factors were subjected to multivariate discriminant analysis based on stepwise addition of the factors that contribute to the largest increase in predicted clinical response. Each selected factor was then correlated with outcome to determine a single cutoff point for that factor that maximized predictive significance. A p value of less than 0.05 using a two-tailed test was taken as being statistically significant for all tests. All analyses were performed with SPSS v10.0 (SPSS Inc., Chicago, IL).
Results
A total of 61 asthmatic subjects agreed to participate in the study and 48 subjects completed the study. There were eight dropouts in the screening phase: four withdrew because of protocol deviations, two withdrew consent, and two dropped out because of other respiratory distress. There were five dropouts in the active treatment phase: three stopped treatment because of worsening asthma and two were lost to followup. The baseline of the dropouts had no apparent consistent difference in those of subjects completing the study.
There was a reduction in asthma symptom scores (>20%) in 34 patients, a reduction in β2-agonist usage (>20%) in 36 patients, and an increase in FEV1 (>10%) in 32 patients after four weeks of treatment. Twenty-five subjects fit all three criteria mentioned above. The total percentage of responders was 52.1%, which was relatively low [28]. In this trial montelukast was well tolerated, and there were no unexpected adverse events. However, additional clinical trials are needed to understand the long-term safety profile.
The baseline demographic and asthma characteristics of the 48 subjects are presented in Table 1. There were no clinically important differences of demographic and asthma characteristics between the two groups. However, there was a predominance of females and allergy in both groups. Most subjects were using inhaled corticosteroids, but there was no significant difference in the proportion of using inhaled corticosteroids in the responder group and in the nonresponder group (80.0% vs. 82.6%).
The baseline clinical and laboratory data are presented in Table 2. The differences in baseline clinical data between the two groups were minor and nonsignificant. All patients enrolled in the study had mild to moderate asthma and were symptomatic at baseline. The mean FEV1 at baseline was 1.95 L, corresponding to 77.5% of the predicted value. WBC counts, percentage of eosinophils, and serum IgE levels showed no significant differences between the two groups. The uLTE4 level of the responders was significantly higher than that of the nonresponders (224.5 ± 34.4 vs. 175.3 ± 37.1 pg/mg creatinine, p < 0.05).
There was clear improvement in the asthma symptom scores, β2-agonist usage, and FEV1 measurements in the responders after treatment (p < 0.05). However, in the nonresponders the improvement was small and not insignificantly different compared with the baseline value according to the standards above (Table 3). There were statistically significant differences of these data after treatment between the two groups (p < 0.05).
The distribution range of uLTE4 levels in this trial was wide and skewed (mean = 220.4 ± 89.5 pg/mg creatinine; 50% percentile = 199.6 pg/mg creatinine; range = 352.9 pg/mg creatinine). Comparison between the subgroups of mild to moderate asthmatics in the responders revealed no significant difference in uLTE4 at baseline levels (207.6 ± 36.8 vs. 218.2 ± 31.5 pg/mg creatinine, p = 0.34). The uLTE4 levels in the responders after treatment had some reduction compared with the baseline values, which did not reach statistical significance (213.6 ± 38.5 vs. 224.5 ± 34.4 pg/mg creatinine, p = 0.45). Regression analysis of uLTE4 levels and percentage predicted FEV1 at baseline showed that uLTE4 increased as FEV1 decreased, but the degree of negative correlation was weak in this trial (r = −0.352; 95% CI = −0.23 to −0.56) (Fig. 1).
A logistic regression model was set up to test the correlation between the clinical factors and the therapeutic response to montelukast. We had classified all subjects into two subgroups according to the transformed variables that maximized predicted significance (Table 4). The clinical response had a clearly significant correlation with uLTE4 levels (p < 0.05), but not with age, WBC counts, percentage of eosinophils, percentage predicted FEV1, PEFR, or serum IgE levels. Patients who had a uLTE4 concentration of ≥ 200 pg/mg creratinine were 3.5 times more likely to respond to montelukast than those with less than 200 pg/mg creratinine (95% CI = 1.7–15.8, p < 0.05). While the predicted cut value is defined as 0.50, the correct predicted probability of the responder group is about 88.0%.
Discussion
To the best of our knowledge, this clinical investigation is the first to explore the relationship between the clinical factors and response to antileukotriene treatment with montelukast in patients with asthma. We found that uLTE4 levels of the responders were higher than those of the nonresponders, and the clinical response had a clearly significant correlation with uLTE4 levels but not with age, WBC counts, percentage of eosinophils, percentage predicted FEV1, PEFR, or serum IgE levels. This expected response, observed in some but not all subjects (52.1%), suggested that there may be a subpopulation of asthma for which CysLTs were main factors in stimulating airway inflammation and that these drugs may have potent effects in only a subpopulation with high levels of CysLTs [8, 34].
We reasoned that the variable clinical response to antileukotriene treatment would result from intrinsic differences in features of asthma clinic manifestations, magnitude of cysteinyl leukotriene generation, genetic polymorphisms in leukotriene receptors, or immunologic pathway. Regrettably, no significant differences in other clinical features between the two groups were found except for the uLTE4. Drazen et al. [9] found that the proportion of responders to inhaled albuterol with high uLTE4 excretion was higher than that of nonresponders with low uLTE4 excretion (81.2% vs. 33.3%). Hasday et al. [13] reported that treatment with the 5-lipoxygenase inhibitor zileuton resulted in a reduction in postantigen BALF eosinophil count by 68% in the high leukotriene producers but there was no detectable effect in the low leukotriene producers. Their data suggested that leukotriene inhibition would be more effective in a subset in which CysLTs were a major contributory factor. It seems likely that in the responders the mechanism of airway inflammation is mediated mainly by the CysLTs-dependent inflammation. In contrast, in the nonresponders the mechanism is probably due to other mediators such as histamine and virus infection, and CysLTs may have minor responsibility for the chronic inflammation (CysLTs-independent inflammation). Another possible explanation is genetic variation in 5-lipoxygenase (5-LO) pathway enzymes. Studies have suggested a significant contribution of genetic variation in 5-LO pathway enzymes to various asthma phenotypes [6, 12]. Asano et al. [2] found that there were mutations in the GC-rich recognition sites for the transcription factor Sp1 described in the human 5-LO gene. They found that subjects with homozygotes for mutant 5-LO alleles were relatively resistant to treatment with the 5-LO inhibitor ABT-761 [2]..The mutant 5-LO alleles may therefore help to indicate individuals with specific asthma phenotypes that are relatively independent of CysLTs. Although our data showed the heterogeneous states of antileukotriene therapy, additional studies are needed to understand the pathophysiology of asthma (i.e., cytokine profile and mediator predominance) before extrapolating the result to practice.
There were no significant differences in uLTE4 at baseline between the subgroup of mild to moderate asthmatics in the responders and no statistical reduction of uLTE4 levels after treatment compared with baseline. Because all patients enrolled in this trial were in stable mild to moderate states, there was no more “reduction degree” observed than that in severely ill states. Montelukast is just a specific and selective receptor antagonist drug, which blocks only the action of CysLTs but not the synthesis. In patients with asthma, eosinophils, mast cells, and basophils are the predominant cell types expressing the requisite enzymes for CysLTs synthesis [1, 7]. The antileukotriene drugs have antiiflammatory activity, interrupt the inflammatory cells’ influx, and hence prevent the release of CysLTs in the longer observation after resolution.
There are potent explanations for the negative correlation between uLTE4 levels and percentage predicted FEV1 at baseline observed in this trial. The result is consistent with the mild to moderate baseline airway obstruction. The change magnitude in FEV1 and uLTE4 would be less obvious than those in severe asthmatics. Hasday et al. [13] reported a 15.4% improvement in FEV1 during zileuton therapy in subjects with moderate asthma, whereas Riccioni et al. [28] failed to show any significant effect of treatment with zafirlukast on FEV1 in subjects with milder asthma. It was also possible that the nonresponders were very sensitive to the contractile effect of CysLTs and that even small amounts could contribute to a substantial contractile effect [16]. Other methodologic factors may explain this result, including the short duration of observation, small sample size, and the method of trial design. Considering the mild to moderate baseline, this negative relationship and the improvement in FEV1 suggest the important roles of CysLTs as key mediators in the clinical spectrum of asthma.
The pulmonary metabolism of CysLTs in vivo results in a rapid and exclusive formation of LTE4 without further conversion and is recovered in the urine as LTE4 (2%–6%) [20, 25, 29]. The uLTE4 excretion rates were known to increase during asthma [11]. CysLTs measurement in urine has more advantages than that in blood [18]. Therefore, uLTE4 measurement can be considered an appropriate biomarker for an integrated measure of CysLTs production. Kumlin et al. [18, 35] reported that there was close correlation between the results in crude samples obtained from enzyme immunoassay and those from radioimmunoassay; our method is reliable and reproducible.
We recognize that some limitations of the current study deserve comment. First, the choice of referred standards of responders and nonresponders must be questioned. Perhaps it is not surprising that the indexes of symptom scores, β2-agonist usage, and FEV1 measurement are rather inadequate surrogate markers of airway obstruction and airway inflammation as measured by laboratory tests and pathologic biopsy. However, measurements of symptoms and lung function are important parameters for assessing the characteristics of asthma. Various symptom scores have been validated to quantify asthma control. A wide range of methods to assess airflow limitation exists, but two methods have found widespread acceptance for use in patients, i.e., FEV1 and PEFR. Leone et al. [21] reported that no single factor of this disease status should be used as a predictive indicator of treatment results. In addition, the multifactorial assessment using the three criteria can rigorously reflect the different aspects of altered physiology in asthma and more accurately predict the treatment response. The standard in this trial can reflect the real efficacy of montelukast [10, 21, 33]. The improvements from baseline are suitable and valuable in clinical practice [4, 14]. In this trial the correct predicted probability of the responder group is about 88.0%.
Second, the improvements attributable to montelukast might be confounded by the concomitant therapies between the two groups. In fact, no significant differences in concomitant therapies (i.e., inhaled corticosteroids or inhaled β2-agonist usage) were observed between the two groups. The effects of inhaled corticosteroids on the CysLTs are controversial. Most patients in this trial received inhaled corticosteroids as part of treatment. However, Leigh et al. [20] showed that inhaled corticosteroids do not suppress either leukotriene production or release into circulation. Moreover, there were no differences in the ratio of inhaled corticosteroids between the two groups.
Finally, all subjects enrolled in this study had mild to moderate stable asthma and severely ill p atients were excluded. The improvements in the referred standards would be less obvious than those in severe asthmatics. The variations in responders to the concomitant therapies were not considered in this study, which would be potential confounding factors. However, previous studies demonstrated that the proportions of variations in responders to inhaled β2 agonists or inhaled corticosteroids were very low and rarely seen [3, 26]. Our results would appear to be representative of mild to moderate stable asthma in adults.
In summary, our study further confirms the activations of leukotriene pathways and the efficacy of antileukotriene treatment in a subset of asthmatics. Moreover, we demonstrated the correlation between clinical responses and uLTE4 concentrations. The uLTE4 could be used as an effective and promising biomarker to predict the clinical response in subpopulations of asthma. It is necessary to carry out extensive characterization of asthma in a larger sample size. This may identify general characteristics of patients that predict a response to this drug and enable clinicians to the right drug for the right patient.
References
Abadoglu O, Mungan D, Aksu O, Erekul S, Misirligil Z (2005) The effect of montelukast on eosinophil apoptosis: induced sputum findings of patients with mild persistent asthma. Allergol Immunopathol 33:105–111
Asano K, Shiomi T, Hasegawa N, et al. (2002) Leukotriene C4 synthase gene A(-444)C polymorphism and clinical response to a CYS-LT(1) antagonist, pranlukast, in patients with moderate asthma. Pharmacogenetics 12:565–570
Ayres JG, Miles JF, Barnes PJ (1998) Brittle asthma. Thorax 53:315–321
Baumgartner RA, Martinez G, Edelman JM, et al. Montelukast Asthma Study Group (2003) Distribution of therapeutic response in asthma between montelukast and inhaled beclomethasone. Eur Respir J 21:123–128
Bousquet J, Chenz P, Lacoste JP, et al. (1990) Eosinophilic inflammation in asthma. N Engl J Med 323:1033–1039
Cookson WO (2002) Asthma genetics. Chest 121:7S–13S
Cowburn A, Sladek K, Soja J, et al. (1998) Over-expression of leukotriene C4 synthase in bronchial biopsies of aspirin-intolerant asthmatics. J Clin Invest 101:834–846
Creticos P, Knobil K, Edwards LD, Rickard KA, Dorinsky P (2002) Loss of response to treatment with leukotriene receptor antagonists but not inhaled corticosteroids in patients over 50 years of age. Ann Allergy Asthma Immunol 88:401–409
Drazen JM, O’Brien J, Sparrow D, et al. (1992) Recovery of leukotriene E4 from the urine of patients with airway obstruction. Am Rev Respir Dis 146:104–108
Drazen JM, Israel E, O’Bryne PM (1999) Treatment of asthma with drugs modifying the leukotriene pathway. N Engl J Med 340:197–206
Green SA, Malice MP, Tanaka W, Tozzi CA, Reiss TF (2004) Increase in urinary leukotriene LTE4 levels in acute asthma: Correlation with airflow limitation. Thorax 59:100–104
Hakonarson H, Wjast M (2001) Current concepts on the genetics of asthma. Curr Opin Pediatr 13:267–277
Hasday JD, Meltzer SS, Moore WC, et al. (2000) Anti-inflammatory effects of zileuton in a subpopulation of allergic asthmatics. Am J Respir Crit Care Med 161:1229–1236
Hoffjan S, Nicolae D, Ober C (2003) Association studies for asthma and atopic diseases: a comprehensive review of the literature. Respir Res 4:14–25
Horwitz RJ, McGill KA, Busse WW (1998) The Role of leukotriene modifiers in the treatment of asthma. Am J Respir Crit Care Med 157:1363–1371
Jayaram L, Pizzichini E, Lemière C, et al. (2005) Steroid naive eosinophilic asthma: anti-inflammatory effects of fluticasone and montelukast. Thorax 60:100–105
Kenji M, Yasurou K, Hideko M, et al. (2002) Reduction of eosinophic inflammation in the airways of patients with asthma using Montelukast. Chest 121:732–738
Kumlin M (2000) Measurement of leukotrienes in humans. Am J Respir Crit Care Med 161:102s–106s
Kumlin M, Stensvad F, Larsson L, Dahlén B, Dahlén SE (1995) Validation and application of a new simple strategy for measurements of urinary leukotriene E4 in humans. Clin Exp Allergy 25:467–479
Leigh R, Vethanayagam D, Yoshida M, et al. (2002) Effects of montelukast and dudesonide on airway responses and airway inflammation in asthma. Am J Respir Crit Care Med 166:1212–1217
Leone FT, Mauger EA, Peters SP, et al. (2001) The utility of peak flow, symptom scores, and ß-agonist use as outcome measures in asthma clinical research. Chest 119:1027–1033
Lídia ML, Carlos Alberto MF, Eliezer JB (2004) Cysteinyl leukotriene receptor antagonists & thromboxane synthase inhibitors: new targets to treat asthma. Curr Med Chem 3:9–18
National Asthma Education and Prevention Program (2002) GINA expert panel report guidelines for the diagnosis management of asthma. Bethesda, MD: National Heart, Lung and Blood Institute, NIH Publication 02-5075
Norris CR, Decile KC, Berghaus LJ, et al. (2003) Concentrations of cysteinyl leukotrienes in urine and bronchoalveolar lavage fluid of cats with experimentally induced asthma. J Vet Res 64:1449–1453
O’Sullivan S, Roquet A, Dahlén B, Dahlén SE, Kumlin M (1998) Urinary excretion of inflammatory mediators during allergen induced early and late phase asthmatic reactions. Clin Exp Allergy 28:1332–1339
Zeiger RS, Baker JW, Kaplan MS, et al. and MIAMI Study Research Group (2004) Variability of symptoms in mild persistent asthma: baseline data from the MIAMI study. Respir Med 98:898–905
Oommen A, Grigg J (2003) Urinary leukotriene E4 in preschool children with acute clinical viral wheeze. Eur Respir J 21:149–154
Riccioni G, Della VR, Diilio C, Orazio ND (2004) Effect of the two different leukotriene receptor antagonists, montelukast and zafirlukast, on quality of life: a 12-week randomized study. Allergy Asthma Proc 25:445–458
Sala A, Voelkel N, Maclouf J (1990) Leukotriene E4 elimination and metabolism in normal human subjects. J Biol Chem 265:21771–21778
Salvi SS, Krishna MT, Sampson AP, Holgate ST (2001) The anti-inflammatory effects of leukotriene-modifying drugs and their use in asthma. Chest 119:1533–1543
Samuelsson B, Dahlen SE, Lindgren JA, Rouzer CA, Serhan CN (1987) Leukotrienes and lipoxins: Structures, biosynthesis, and biological effects. Science 237:1171–1176
Sousa AR, Parikh A, Scadding G, Corrigan CJ, Lee TH (2002) Leukotriene-receptor expression on nasal mucosal inflammatory cells in aspirin-sensitive rhinosinusitis. N Engl J Med 347:1493–1499
Storms W, Michele TM, Knorr B, et al. (2001) Clinical safety and tolerability of montelukast, a leukotriene receptor antagonist, in controlled clinical trials in patients aged>or = 6 years. Clin Exp Allergy 31:77–87
Szefler SJ, Phillips BR, Martinez FD, et al. (2005) Characterization of within-subject responses to fluticasone and montelukast in childhood asthma. J Allergy Clin Immunol 115:233–242
Vachier I, Kumlin M, Dahlen SE, et al. (2003) High levels of urinary leukotriene E4 excretion in steroid treated patients with severe asthma. Respir Med 97:1225–1229
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cai, C., Yang, J., Hu, S. et al. Relationship Between Urinary Cysteinyl Leukotriene E4 Levels and Clinical Response to Antileukotriene Treatment in Patients with Asthma. Lung 185, 105–112 (2007). https://doi.org/10.1007/s00408-006-0001-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-006-0001-8