Abstract
Many patients do not respond to the first antipsychotic drug prescribed, but require multiple trials with different drugs before response is achieved. Current treatment guidelines vary substantially in their recommendations as to how long clinicians should wait before an antipsychotic treatment attempt should be considered as failed and the compound switched. It has, however, recently been shown that poor early response to an antipsychotic is associated with continuous poor later response in the course of the same treatment attempt. This finding suggests that patients who do experience poor early response might benefit from a switch in antipsychotic medication as early as 2 weeks after treatment initiation. In the SWITCH trial, 350 patients suffering from an acute episode of schizophrenia are randomly assigned to double-blind treatment with either olanzapine or amisulpride. The primary endpoint is symptomatic remission at week 8. Patients not experiencing at least minor response after 2 weeks are randomized again to either staying on the initially assigned drug or being switched to the alternative compound for another 6 weeks. In case early switching proves superior to maintaining treatment, time wasted for unsuccessful treatment attempts could be minimized, patients’ outcomes improved, duration of hospital stays reduced, and thus overall treatment expenses saved. The current report will present the methods of the trial, focusing on various specific features which could be adopted by future studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The time course of antipsychotic drug effect
The meaningful question by when to consider an antipsychotic treatment attempt as having failed and thus consequently demanding a switch in medication remains a major challenge in the pharmacological treatment of schizophrenia. For decades, textbooks stated that there is a delayed onset of action of antipsychotic drugs of several weeks. Two recent meta-analyses have clearly rejected the delayed onset of action hypothesis [1, 34]. In fact, the antipsychotic drug effect onset rather starts at least as early as in the first week of treatment, although substantially more time is needed until the full magnitude of the antipsychotic effect is reached. Even within the first 24 h of antipsychotic drug exposure, patients showed a measurable effect of treatment [2]. So, the delayed-onset hypothesis changed into an early-onset hypothesis.
The meaning of the early-onset hypothesis for clinical practice
The early onset of antipsychotic action makes response detection possible at a very early stage in the course of a treatment attempt and may also enable us to predict later non-response when early response is not achieved. Several studies using receiver operating characteristic (ROC) curve analyses in large data sets originating from antipsychotic drug trials found that later non-responders (measured at study endpoints at 4–8 weeks after treatment initiation) can be identified as early as 2 weeks after start of treatment [4, 11, 27, 35, 39]. While the exact cut-off in symptom reduction after 2 weeks of treatment predicting later individual non-response varied in the cited studies, they all consistently showed that those patients initially experiencing only poor reduction in symptoms were unlikely to respond profoundly in the same treatment attempt later on. For the SWITCH study, a 25 % cut-off in PANSS reduction at week 2 was chosen. This decision was drawn based on a previous study of our group [35] and recently corroborated by a diagnostic test review demonstrating that the best trade-off between sensitivity and specificity of a broad range of cut-offs (0–50 % PANSS/BPRS reduction at 2 weeks) lies around a cut-off of 20–25 % reduction [46].
Noteworthily, the current guidelines for the treatment of schizophrenia do vary substantially in the recommended time as to how long clinicians should wait before an antipsychotic treatment attempt should be considered as failed and the compound switched [17, 18, 32]. So, identifying a time span as short as possible that represents a meaningful cut-off for accurately predicting later poor response is of high clinical relevance and is therefore addressed in the current trial.
Pooling the evidence, from both the early-onset hypothesis plus the prediction of subsequent poor overall treatment benefit indicated by early poor response, led to the idea for the current trial. The resulting question is whether an early change of the antipsychotic compound to a different drug in case of poor initial response leads to an overall better outcome at the end of an 8-week antipsychotic treatment attempt. In our view, this question can only be answered by a randomized study in which initial poor responders at 2 weeks of treatment are either switched to another compound with a different receptor binding profile (cf. method section) in the intervention group or maintained on the same drug in the control condition.
Randomized studies having examined the meaning of the early-onset hypothesis in clinical practice so far
Up to date, all studies published on the antipsychotic switch issue outlined above have investigated the effects of antipsychotic drug switches (a) at later stages in the treatment process and (b) do suffer from different methodological limitations in our view. In the following, we briefly summarize our major points of concern:
The earliest study was done by Kinon et al. [29] in which 115 patients were treated with fluphenazine 20 mg/d for 4 weeks. Subsequently, poor responders were randomized to either double-blind continuation of fluphenazine at 20 mg/d, a dose increase in fluphenazine to 80 mg/d, or a switch to haloperidol. A limitation is the rather late switch performed from one high-potency first-generation antipsychotic (FGA) to another FGA (i.e. comparable D2 receptor affinity).
In the study by Shalev et al., 60 patients were randomized to treatment with haloperidol, perphenazine, or chlorpromazine [48]. Poor responders after 4 weeks were randomly switched to open-label treatment with one of the two remaining alternative antipsychotics and, if still not responding, again after another 4 weeks. In summary, 67 % of the patients responded to the first treatment attempt, another 55 % to the second, and finally 67 % to the third. Here, methodological limitations are the late switch, the small sample size, the open-label setting, and the lack of a control group.
In an open-label trial of Suzuki et al., 78 patients were randomized to olanzapine, quetiapine, or risperidone [52]. After 8 weeks, poor responders were randomized to one of the two remaining drugs. Finally, 16 patients did not respond to both treatment attempts. Again the open-label design, the lack of a control intervention, and the late switch are critical.
In another small-sized trial, Kinon et al. [28] switched patients having minimally improved after 2 weeks of risperidone to olanzapine, leading then to a statistically significantly better outcome compared to risperidone maintenance.
Hatta et al. [22] randomized non-improvers after 2 weeks of risperidone or olanzapine to staying on the same drug or switching to the alternative one. Switching did not lead to higher response rates, but the authors emphasize that the trial was underpowered for this question.
In conclusion, the existing evidence supports our hypothesis that an early switch of antipsychotic treatment might be beneficial to patients in case of early poor response.
Study design
Study objectives
The primary outcome of the SWITCH study is the number of patients having poorly responded to the initial antipsychotic treatment (at week 2) and later on reaching symptomatic remission [3] at the end of the trial (at week 8). Patients having experienced poor initial response plus having undergone a randomized switch in their antipsychotic medication after 2 weeks of treatment (switch group) will be compared to patients having been randomized to staying with their initially assigned antipsychotic drug after poor initial response (non-switch group). The study hypothesis is that at the end of the study, significantly more patients in the switch group will be in symptomatic remission compared to the non-switch group.
Amongst others, secondary endpoints comprise the comparison in changes in different dimensions of psychopathology [21, 26], side effects, social functioning [40], subjective well-being under antipsychotic treatment [43], the attitude towards antipsychotic treatment [24], and the treatment costs between the switch and the non-switch group. All outcomes will also be analysed for all patients responding to the initial antipsychotic treatment (responder group).
In addition, results from pharmacogenetic examinations of polymorphisms of the cytochrome P450 enzyme and other mutations that may be associated with treatment response in schizophrenia (e.g. mutations of transporter mechanisms for neurotransmitters or intracellular signal processing or of neuroreceptors) will be analysed.
Antipsychotic treatment strategies (“switch versus non-switch”)
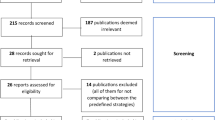
The SWITCH study is a randomized, controlled, double-blind comparison of two treatment strategies in an acute episode of schizophrenia or schizoaffective disorder involving the antipsychotics amisulpride and olanzapine. Participants having signed informed consent forms will first enter an optional screening phase of up to 3 days (washout). Phase I starts with the baseline visit (day 1) and ends with the subsequent visit at day 14. At the start of phase I, patients will be randomly (1st randomization) assigned to double-blind treatment with either amisulpride or olanzapine for the entire 2 weeks of phase I (Fig. 1).
At the end of phase I (day 14), patients having sufficiently responded to the initial treatment (i.e. ≥25 % improvement in the PANSS; “responders”) will continue double-blind treatment with the same compound also in phase II for additional 6 weeks.
Patients not having experienced sufficient response at the end of phase I (“non-responders”) will undergo a second randomization. They will either be randomized to the control group (“non-switch group”) and continue on the same compound as in phase I also now in phase II, or alternatively enter the intervention group (“switch group”) and undergo a cross-titration phase. In phase II of the trial, they will then be treated with the alternative compound they have not been treated with in phase I.
In order to control for any potential difference in antipsychotic efficacy of the two compounds per se, we chose this “crossover” design with two randomizations. Thus, in the final analysis, both switch groups of phase II (i.e. those patients switched from olanzapine to amisulpride and vice versa) will merge. Likewise, both “non-switch” groups of phase II will merge. In essence, the primary outcome compares solely the two strategies (i.e. switch versus non-switch) in poorly responding patients.
All antipsychotic treatment will be performed under double-blind conditions. Capsules containing amisulpride or olanzapine do not differ in appearance or weight. This procedure shall minimize any bias arising from patients’ or doctors’ expectations as to whether one of the two drugs or the switch itself might be beneficial or not.
Finally, patients having completed the entire 56-day trial may be switched to any antipsychotic medication available after study drug discontinuation.
Study population
Patients aged 18–65 meeting DSM-IV criteria for schizophrenia, schizoaffective disorder, or schizophreniform disorder as confirmed by the M.I.N.I. International Neuropsychiatric Interview Plus can be enrolled in the trial. Participants must give written informed consent in agreement with the principles of the Declaration of Helsinki and the International Committee on the Harmonization of Good Clinical Practice (ICH-GCP). Consent to the pharmacogenetic sampling in the trial is optional. The protocol must be approved by local ethical committees or review boards according to country-specific laws.
Both at screening and at baseline, the PANSS total score must be ≥75 points, and at least two items of the PANSS “positive component factor cluster” (P1, G9, P3, P6, P5, G12) must be scored at least 4 (moderate). At study inclusion, the CGI-S rating must be ≥4 and an increase in the level of care (admission to inpatient or day care, admission from day care to inpatient care) must have taken place within 5 working days prior to enrolment.
Patients will not be eligible for the trial if they do not meet all the inclusion criteria listed above or if they are known to be intolerant to one of the study drugs or meet contraindications according to package inserts. Patients cannot be enrolled in case of a documented non-response to a 6- to 8-week treatment attempt in the past or continuous treatment with one of the study drugs in the 2 weeks preceding study entry (olanzapine 10–20 mg/d, amisulpride 400–800 mg/d; sufficient compliance provided). Inclusion should not be considered if the current episode shows no clinical change in the 4 weeks preceding study entry despite adequate antipsychotic treatment and sufficient compliance provided. If a patient experiences a ≥25 % reduction in PANSS total score from screening to baseline, the patient must be discontinued. Involuntarily treated patients must not participate in the study, and patients are not allowed to participate in another trial simultaneously.
Further exclusion criteria are imminent risk of suicide, hazard risk for others, depot antipsychotic treatment within one injection cycle, current pregnancy or lactation, the plan to become pregnant within the next 3 months, the diagnosis of substance dependency according to DSM-IV TR criteria in the 3 months preceding study entry (excluding nicotine and caffeine), any somatic diseases or abnormal test results that are relevant in the study doctor’s opinion, and previous enrolment in the trial.
Choice of compounds
Olanzapine and amisulpride are both second-generation antipsychotics (SGAs) and have demonstrated comparable efficacy in the treatment of schizophrenia within several large randomized, controlled trials (e.g. the EUFEST study) [25, 31, 41, 54] and meta-analyses [37] [12, 38]. They belong to the group of second-generation antipsychotics (SGAs), including a positive safety profile and a low incidence of extrapyramidal side effects [14]. However, the receptor binding profiles are distinctly different with amisulpride being a selective dopamine antagonist and olanzapine blocking central serotonergic 5-HT-2a receptors more than dopamine receptors [8, 9, 44].
The underlying idea to choose compounds with a differing receptor binding profile derives partly from findings in phase II of the Clinical Antipsychotic Trial of Intervention Effectiveness (CATIE) trial. A post hoc analysis showed that a switch to a drug with a different receptor binding profile might be beneficial [51].
Regarding other SGA, there is some evidence from meta-analyses [36, 37] that suggest that, for example, quetiapine, aripiprazole, or ziprasidone are inferior to olanzapine and amisulpride with regard to their antipsychotic efficacy.
We decided not to use clozapine due to its side effects, blood count controls, and the necessity of slowly up-titrating the drug.
Finally, we decided against a FGA because the distinctly different side effect profiles most FGAs demonstrate compared to a SGA (e.g. with regard to EPS) might have unmasked the blinding of the study. Some FGAs, e.g. perphenazine, would have qualified as robust comparators, especially taking into account the idea of utilizing different receptor binding profiles, but they are too seldom prescribed in acute treatment in Germany or Romania and therefore are not representative for the actual clinical routine. Additionally, the use of FGAs has caused serious recruitment problems in a recent trial [19].
Dosing of study medication
In phase I, antipsychotic treatment will be titrated from day 1 in a flexible manner with doses of 600–800 mg/d of amisulpride or 15–20 mg/d of olanzapine as target dose to be reached on day 3. Thereafter, flexible doses of amisulpride 200–800 mg/d or olanzapine 5–20 mg/d are allowed [6, 45]. All decreases in dose should only be considered in case of poor tolerability. In week 3, non-responders randomized to “switch” will be cross-tapered to the alternative compound in a set manner.
Definition of the primary endpoint remission
A major criticism of schizophrenia trials is that they often use outcomes such as differences in the PANSS total score which are difficult to interpret clinically. Such a choice may be justifiable in registrational studies, but in studies such as SWITCH which aim to inform on clinical decisions, their usefulness can be criticized. We therefore chose symptomatic remission (RSWG) [3] as primary outcome. Several studies were able to show a strong correlation between patients reaching remission and other important outcomes (better quality of life, social functioning, cognitive performance, subjective well-being, and a more stable state of health [10, 13, 15, 16, 23, 33, 47, 53]; for summary, please see [30]). So, the striking clinical relevance of all these important outcomes reflected indirectly by reaching the remission status leads us to choosing this outcome parameter as our primary endpoint. Analyses of large databases have confirmed that remission is a realistic goal within clinical schizophrenia studies [33]. Noteworthily, we cannot address the 6-month time criterion in this short-term trial and so have to limit the outcome to symptomatic remission only.
Randomization
Patients will be randomized in order to avoid a systematic bias. Thus, patients with certain characteristics (e.g. gender, age, symptoms at baseline) should be equally allocated to treatment arms. Drug treatment will be blinded to reduce bias resulting from doctors’ and patients’ expectations towards treatment. To our knowledge, this is the first antipsychotic treatment trial using a two-time randomization design. Computer-assisted randomization will be performed by the Institut fuer Medizinische Statistik und Epidemiologie (IMSE) at the Technische Universitaet. The treatment randomization listings are generated using Rancode Professional 3.6, stratified by study centre and with block size of 4. The actual assignment is done on the phone by an independent person using the pre-generated listings.
At baseline, patients will be randomized (1st randomization) to either amisulpride or olanzapine double-blind treatment in a 1:1 ratio by centre-specific randomization lists with pre-specified block lengths. Group allocation (i.e. drug allocation) will be done by the manufacturer of the study drugs, the pharmacy of the university in Mainz, Germany, so that allocation will be concealed at all stages.
At the 2nd randomization (day 14), all patients who did not respond sufficiently to treatment in phase I (i.e. <25 % reduction in PANSS total) will be randomized in a 1:1 ratio to either receive the compound of phase I for another 6 weeks or be switched to the alternative compound.
Patients who responded to antipsychotic treatment of phase I will not be randomized and continue on the same compound as in phase I undergoing a pseudo-randomization to maintain the blind. In emergency cases, allocation to study drugs can be unblinded through sealed envelopes.
Concomitant therapy
To avoid study results being biased by concomitant medication and to prevent patients from drug interactions, certain drugs (e.g. additional antipsychotics, recently initiated antidepressants, or mood stabilizers) must not be given to patients. Rescue medication for symptomatic treatment of agitation, sleep disturbances, or side effects is permitted according to the regulations of the study protocol. These are lorazepam (max. 6 mg/d), diazepam (max. 60 mg/d), zolpidem (max. 10 mg/d), lormetazepam (max. 2 mg/d), zopiclone (max. 7.5 mg/d), temazepam (max. 20 mg/d), and biperiden (max. 6 mg/d).
Outcome measures
The PANSS will be used to assess remission. All investigators will be trained repeatedly prior and throughout the trial on the adequate use of this scale. Further scales used are the CGI-S/CGI-I, the SWN scale [42], the DAI-10 scale [24] (Table 1).
The “Personal and Social Performance Scale” (PSP) [40] measures patients’ performance on several levels of social and daily life; extrapyramidal side effects will be monitored by the “Simpson–Angus Scale” (SAS) [49] and the “Barnes Akathisia Scale” (BAS) [5]; and other side effects will be assessed by the “Dosage Record and Treatment Emergent Symptoms Scale” (DOTES) [20]. In the treatment costs analysis, it shall be investigated whether patients with a poor initial response cause higher expenses than patients with an early response and whether an early switch of antipsychotic treatment in case of a poor initial response reduces treatment costs compared to the non-switch scenario [4]. Basis for the cost calculation will be the per-day hospital treatment costs for inpatient stays or day care treatment. The measurement of plasma drug concentration at several visits aims for checking patients’ compliance as well as assessing the correlation of plasma levels and treatment response.
Sample size calculation
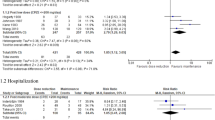
For the primary outcome, a sample size of 82 in each group will have 80 % power to detect a difference of 20 % in remission rates (two-sided, Chi-square test, α < 0.05), assuming a 40 % remission rate in the switch group and a 20 % rate in the non-switch group.
A pooled analysis of four randomized, double-blind, controlled studies involving 1481 patients over a minimum of 8 weeks has shown that 20 % of the “non-responders” (<25 % PANSS total reduction) at 2 weeks and undergoing no change in their treatment thereafter actually reached symptomatic remission at 8 weeks [39]. There are two minor, randomized, but non-blinded studies suggesting remission rates of 36 and 55 %, respectively, when patients are switched in case of non-response [48, 52]. We therefore decided to see a difference of 20 % in remission rates as clinically relevant.
To obtain 164 study completers for the primary outcome, we expect 350 patients to be randomized in phase I (including 30 % dropouts and accounting for responders not entering the primary analysis). Patients randomized into phase II (“non-responder”) constitute the intention-to-treat (“ITT”) population, and overall 500 patients need to be screened.
Compliance/“dropout” rates
Kemmler and colleagues reported a dropout rate of 28 % in recent short-term (up to 12 weeks) randomized controlled trials. These studies were registrational studies conducted by pharmaceutical companies. Although our current trial is not for registrational purposes and uses marketed drugs that should result in lower dropout rates, we still take into account an overall 30 % dropout rate.
Statistical analysis
The primary analysis will include those patients who were “non-responders” during phase I and were then randomized to a switch or non-switch arm for phase II. The switch and non-switch arms will be compared and tested for superiority in terms of the proportion of patients in remission at visit 7 (week 8). The primary analysis model will be a logistic regression model with “remission” as the dependent variable and “switch” of treatment (yes/no) and PANSS total score at visit 3 as independent variables. The focus of the primary analysis will be the estimate of the “switch” coefficient. Centre will not be included in our primary analysis model, but the impact of its inclusion will be assessed in a secondary analysis.
A secondary analysis will assess whether the effect of switching differs depending on the drug assigned in phase I. To achieve this, the drug allocated at first randomization will be added to the logistic regression model together with an interaction term for “switch” and the drug allocated at first randomization.
An intention-to-treat approach will be taken for the analysis with several approaches taken to deal with missing primary outcome data. The primary analysis will be conducted using multiple imputation (using the R package mice) [50]. Multiple imputation, under the assumption that data are missing at random, will be performed separately for the switch and non-switch arms. Logistic regression imputation models for remission will contain the PANSS total scores from all visits from baseline (visit 2) onwards, remission at visit 7, and phase I arm allocation. The PANSS score at two weeks (visit 3, second randomization) will be included in the primary analysis model. Missing values for the PANSS total scores will be imputed using predictive mean matching. Twenty imputed data sets will be produced, with results from the imputed data sets pooled using Rubin’s rules. A last observation carried forward (LOCF) analysis and a completers-only analysis, including only those patients who provided primary outcome data at visit 7, will also be performed. In addition, a per-protocol analysis will be performed in which patients with major protocol violations will be excluded. Patients will be classified as major protocol violators if they do not provide primary outcome data at visit 7, are unblinded during the course of the study, received the incorrect medication, or are non-compliant. Results from the plasma tests at visit 3, visit 5, and visit 7 will be used to identify non-compliers; if the plasma levels do not test positive for the correct study medication at any time point, the patient will be defined as a non-complier.
Differences in remission rates at week 8 between responders and non-responders of phase I will also be assessed using logistic regression analyses.
Exploratory analyses will be performed to assess changes in the secondary outcome variables between the switch and non-switch groups during phase II. The secondary outcome variables include the total PANSS score and summary measures of the CGI, PSP, SWN, and SAS scales. The changes in these continuous variables, between visit 3 and visit 7, in each group will be summarized by their mean, median, standard deviation, and quartiles. The secondary outcome variables will be assessed graphically for normality via histograms and q–q plots and inspected for outliers. When appropriate, mixed models [7] will be fit to the secondary outcome data recorded during phase II (visits 3–7). The independent variables will include visit number as a factor variable and indicator variables for group assignment at each visit from visit 4 onwards. The focus of these analyses will be the estimated difference between groups at visit 7.
Mixed models will be fit using the gls function within the nlme library in the statistical program R. Unstructured covariance matrices will be used to model the within-subject error.
Participating countries
Sites in Germany (17) and Romania (15) will enrol patients in the trial.
Quality control and assurance
Study sites and associated investigators will be carefully selected, and all study team members will be trained regarding Good Clinical Practice (GCP), all study procedures, and the required examinations and documentation. The quality of data acquisition will be ensured by regular monitoring visits, data entered into the database will be checked for completeness and plausibility, and discrepancy solved by queries. Monitoring will be performed according to national laws/ICH-GCP guidelines and follow a monitoring plan.
Abbreviations
- FGAs:
-
First-generation antipsychotics
- SGAs:
-
Second-generation antipsychotics
- SD:
-
Standard deviation
References
Agid O, Kapur S, Arenovich T, Zipursky RB (2003) Delayed-onset hypothesis of antipsychotic action: a hypothesis tested and rejected. Arch Gen Psychiatry 60:1228–1235
Agid O, Kapur S, Warrington L, Loebel A, Siu C (2008) Early onset of antipsychotic response in the treatment of acutely agitated patients with psychotic disorders. Schizophr Res 102:241–248
Andreasen NC, Carpenter WT Jr, Kane JM, Lasser RA, Marder SR, Weinberger DR (2005) Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry 162:441–449
Ascher-Svanum H, Nyhuis AW, Faries DE, Kinon BJ, Baker RW, Shekhar A (2008) Clinical, functional, and economic ramifications of early nonresponse to antipsychotics in the naturalistic treatment of schizophrenia. Schizophr Bull 34:1163–1171
Barnes TRE (1989) A rating scale for drug induced akathisia. Br J Psychiatry 154:672–676
Beasley CM, Hamilton SH, Crawford AM, Dellva MA, Tollefson GD, Tran PV, Blin O, Beuzen J-N (1997) Olanzapine versus haloperidol: acute phase results of the international double-blind olanzapine trial. Eur Neuropsychopharmacol 7:125–137
Bell ML, Kenward MG, Fairclough DL, Horton NJ (2013) Differential dropout and bias in randomised controlled trials: when it matters and when it may not. BMJ 346:e8668
Bymaster F, Perry KW, Nelson DL, Wong DT, Rasmussen K, Moore NA, Calligaro DO (1999) Olanzapine: a basic science update. Br J Psychiatry 174(Suppl. 37):36–40
Bymaster FP, Nelson DL, DeLapp NW, Falcone JF, Eckols K, Truex LL, Foreman MM, Lucaites VL, Calligaro DO (1999) Antagonism by olanzapine of dopamine d1, serotonin(2), muscarinic, histamine h-1 and alpha(1),-adrenergic receptors in vitro. Schizophr Res 37:107–122
Ciudad A, Alvarez E, Bobes J, San L, Polavieja P, Gilaberte I (2009) Remission in schizophrenia: results from a 1-year follow-up observational study. Schizophr Res 108:214–222
Correll CU, Malhotra AK, Kaushik S, McMeniman M, Kane JM (2003) Early prediction of antipsychotic response in schizophrenia. Am J Psychiatry 160:2063–2065
Davis JM, Chen N, Glick ID (2003) A meta-analysis of the efficacy of second-generation antipsychotics. Arch Gen Psychiatry 60:553–564
de Hert M, van Winkel R, Wampers M, Kane J, van Os J, Peuskens J (2007) Remission criteria for schizophrenia: evaluation in a large naturalistic cohort. Schizophr Res 92:68–73
Duggan L, Fenton M, Dardennes RM, El-Dosoky A (2004) Olanzapine for schizophrenia (cochrane review). In: The cochrane library. John Wiley & Sons Ltd, Chichester
Dunayevich E, Sethuraman G, Enerson M, Taylor CC, Lin D (2006) Characteristics of two alternative schizophrenia remission definitions: relationship to clinical and quality of life outcomes. Schizophr Res 86:300–308
Emsley R, Medori R, Koen L, Oosthuizen PP, Niehaus DJ, Rabinowitz J (2008) Long-acting injectable risperidone in the treatment of subjects with recent-onset psychosis: a preliminary study. J Clin Psychopharmacol 28:210–213
Falkai P, Wobrock T, Lieberman J, Glenthoj B, Gattaz WF, Moller HJ (2006) World federation of societies of biological psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, part 2: long-term treatment of schizophrenia. World J Biol Psychiatry 7:5–40
Gaebel W, Falkai P, Weinmann S, Wobrock T (2006) Behandlungsleitlinie schizophrenie. Steinkopff, Darmstadt
Gaebel W, Riesbeck M, Wolwer W, Klimke A, Eickhoff M, von Wilmsdorff M, Jockers-Scherubl MC, Kuhn KU, Lemke M, Bechdolf A, Bender S, Degner D, Schlosser R, Schmidt LG, Schmitt A, Jager M, Buchkremer G, Falkai P, Klingberg S, Kopcke W, Maier W, Hafner H, Ohmann C, Salize HJ, Schneider F, Moller HJ (2007) Maintenance treatment with risperidone or low-dose haloperidol in first-episode schizophrenia: 1-year results of a randomized controlled trial within the german research network on schizophrenia. J Clin Psychiatry 68:1763–1774
Guy U (1976) Ecdeu assessment manual for psychopharmacology. National Institute of Mental Health, Rockville, MD
Guy W (1976) Clinical global impression. Ecdeu assessment manual for psychopharmacology, revised (dhew publ no adm 76-338). National Institute of Mental Health, Rockville, MD, pp 218–222
Hatta K, Otachi T, Sudo Y, Hayakawa T, Ashizawa Y, Takebayashi H, Hayashi N, Hamakawa H, Ito S, Nakase R, Usui C, Nakamura H, Hirata T, Sawa Y, JAST Study Group (2011) Difference in early prediction of antipsychotic non-response between risperidone and olanzapine in the treatment of acute-phase schizophrenia. Schizophr Res 128:127–135
Helldin L, Kane JM, Karilampi U, Norlander T, Archer T (2007) Remission in prognosis of functional outcome: a new dimension in the treatment of patients with psychotic disorders. Schizophr Res 93:160–168
Hogan TP, Awad AG, Eastwood R (1983) A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychol Med 13:177–183
Kahn RS, Fleischhacker WW, Boter H, Davidson M, Vergouwe Y, Keet IP, Gheorghe MD, Rybakowski JK, Galderisi S, Libiger J, Hummer M, Dollfus S, Lopez-Ibor JJ, Hranov LG, Gaebel W, Peuskens J, Lindefors N, Riecher-Rossler A, Grobbee DE, EUFEST Study Group (2008) Effectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trial. Lancet 371:1085–1097
Kay SR, Fiszbein A (1987) The positive and negative symptome scale (PANSS) for schizophrenia. Schizophr Bull 13:261–275
Kinon BJ, Chen L, Ascher-Svanum H, Stauffer VL, Kollack-Walker S, Sniadecki JL, Kane JM (2008) Predicting response to atypical antipsychotics based on early response in the treatment of schizophrenia. Schizophr Res 102:230–240
Kinon BJ, Chen L, Ascher-Svanum H, Stauffer VL, Kollack-Walker S, Zhou W, Kapur S, Kane JM (2010) Early response to antipsychotic drug therapy as a clinical marker of subsequent response in the treatment of schizophrenia. Neuropsychopharmacology 35:581–590
Kinon BJ, Kane JM, Johns C, Perovich R, Ismi M, Koreen A, Weiden P (1993) Treatment of neuroleptic-resistant schizophrenic relapse. Psychopharmacol Bull 29:309–314
Lambert M, Karow A, Leucht S, Schimmelmann BG, Naber D (2010) Remission in schizophrenia: validity, frequency, predictors, and patients’ perspective 5 years later. Dialogues Clin Neurosci 12:393–407
Lecrubier Y, Quintin P, Bouhassira M, Perrin E, Lancrenon S (2006) The treatment of negative symptoms and deficit states of chronic schizophrenia: olanzapine compared to amisulpride and placebo in a 6-month double-blind controlled clinical trial. Acta Psychiatr Scand 114:319–327
Lehman AF, Lieberman JA, Dixon LB, McGlashan TH, Miller AL, Perkins DO, Kreyenbuhl J (2004) Practice guideline for the treatment of patients with schizophrenia, second edition. Am J Psychiatry 161:1–56
Leucht S, Beitinger R, Kissling W (2007) On the concept of remission in schizophrenia. Psychopharmacology 194:453–461
Leucht S, Busch R, Hamann J, Kissling W, Kane JM (2005) Early-onset hypothesis of antipsychotic drug action: a hypothesis tested, confirmed and extended. Biol Psychiatry 57:1543–1549
Leucht S, Busch R, Kissling W, Kane JM (2007) Early prediction of antipsychotic nonresponse among patients with schizophrenia. J Clin Psychiatry 68:352–360
Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, Samara M, Barbui C, Engel RR, Geddes JR, Kissling W, Stapf MP, Lassig B, Salanti G, Davis JM (2013) Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet 382:951–962
Leucht S, Komossa K, Rummel-Kluge C, Corves C, Hunger H, Schmid F, Asenjo Lobos C, Schwarz S, Davis JM (2009) A meta-analysis of head-to-head comparisons of second-generation antipsychotics in the treatment of schizophrenia. Am J Psychiatry 166:152–163
Leucht S, Pitschel-Walz G, Engel RR, Kissling W (2002) Amisulpride, an unusual “atypical” antipsychotic: a meta-analysis of randomized controlled trials. Am J Psychiatry 159:180–190
Leucht S, Shamsi SA, Busch R, Kissling W, Kane JM (2008) Predicting antipsychotic drug response—replication and extension to six weeks in an international olanzapine study. Schizophr Res 101:312–319
Morosini PL, Magliano L, Brambilla L, Ugolini S, Pioli R (2000) Development, reliability and acceptability of a new version of the DSM-IV social and occupational functioning assessment scale (SOFAS) to assess routine social functioning. Acta Psychiatr Scand 101:323–329
Mortimer A, Martin S, Loo H, Peuskens J (2004) A double-blind, randomized comparative trial of amisulpride versus olanzapine for 6 months in the treatment of schizophrenia. Int Clin Psychopharmacol 19:63–69
Naber D, Karow A (2001) Good tolerability equals good results: the patient’s perspective. Eur Neuropsychopharmacol 11(Suppl 4):S391–S396
Naber D, Moritz S, Lambert M, Pajonk FG, Holzbach R, Mass R, Andresen B, Rajonk F (2001) Improvement of schizophrenic patients’ subjective well-being under atypical antipsychotic drugs. Schizophr Res 50:79–88
Perrault G, Depoortere R, Morel E, Sanger DJ, Scatton B (1997) Psychopharmacological profile of amisulpride: an antipsychotic drug with presynaptic d2/d3 dopamine receptor antagonist activity and limbic selectivity. J Pharmacol Exp Ther 280:73–82
Puech A, Fleurot O, Rein W (1998) Amisulpride, an atypical antipsychotic, in the treatment of acute episodes of schizophrenia: a dose-ranging study vs. Haloperidol. Acta Psychiatr Scand 98:65–72
Samara MT, Leucht C, Leeflang MM, Anghelescu IG, Chung YC, Crespo-Facorro B, Elkis H, Hatta K, Giegling I, Kane JM, Kayo M, Lambert M, Lin CH, Möller HJ, Pelayo-Terán JM, Riedel M, Rujescu D, Schimmelmann BG, Serretti A, Correll CU, Leucht S (2015) Early improvement as a predictor of later response to antipsychotics in schizophrenia: a diagnostic test review. Am J Psychiatry 172:617–629
San L, Ciudad A, Alvarez E, Bobes J, Gilaberte I (2007) Symptomatic remission and social/vocational functioning in outpatients with schizophrenia: prevalence and associations in a cross-sectional study. Eur Psychiatry 22:490–498
Shalev A, Hermesh H, Rothberg J, Munitz H (1993) Poor neuroleptic response in acutely exacerbated schizophrenic patients. Acta Psychiatr Scand 87:86–91
Simpson M, Angus JW (1970) A rating scale for extrapyramidal side effects. Acta Psychiatr Scand 212:11–19
van Buuren S, Groothuis-Oudshoorn K (2011) Mice: multivariate imputation by chained equations in R. J Stat Softw 45:1–67
Stroup TS, Lieberman JA, McEvoy JP, Swartz MS, Davis SM, Capuano GA, Rosenheck RA, Keefe RS, Miller AL, Belz I, Hsiao JK, Investigators C (2007) Effectiveness of olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia after discontinuing perphenazine: a CATIE study. Am J Psychiatry 164:415–427
Suzuki T, Uchida H, Watanabe K, Nomura K, Takeuchi H, Tomita M, Tsunoda K, Nio S, Den R, Manki H, Tanabe A, Yagi G, Kashima H (2007) How effective is it to sequentially switch among olanzapine, quetiapine and risperidone?—a randomized, open-label study of algorithm-based antipsychotic treatment to patients with symptomatic schizophrenia in the real-world clinical setting. Psychopharmacology 195:285–295
van Os J, Drukker M, a Campo J, Meijer J, Bak M, Delespaul P (2006) Validation of remission criteria for schizophrenia. Am J Psychiatry 163:2000–2002
Vanelle JM, Douki S (2006) A double-blind randomised comparative trial of amisulpride versus olanzapine for 2 months in the treatment of subjects with schizophrenia and comorbid depression. Eur Psychiatry 21:523–530
Acknowledgement
The authors gratefully acknowledge the support from the German Ministerium fuer Bildung und Forschung (BMBF) and the project management by the Deutsche Luft- und Raumfahrt Organisation (DLR).
Funding
The study conduct is supported by a grant from the “Bundesministerium fuer Bildung und Forschung” (BMBF), a German governmental ministry (Grant code 01KG0910). As sponsor functions the Technische Universitaet Muenchen, represented by the Klinikum rechts der Isar Muenchen. Eli Lilly provides the olanzapine medication for the trial, but has no influence on the protocol, data analysis, publication, or other aspects of the trial.
Study progress
Study recruitment has started in January 2010, and first results can be expected at the end of 2015.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Heres has received lecture honoraria from Janssen-Cilag, Sanofi-Aventis, Bristol-Myers-Squibb, Eli Lilly, and Johnson & Johnson. Dr. Heres acts as consultant and/or participates in board meetings of Janssen-Cilag, Eli Lilly, Roche, Lundbeck, and Johnson & Johnson. Dr. Heres has accepted travel or hospitality payment from Janssen-Cilag, Sanofi-Aventis, Johnson & Johnson, Pfizer, Bristol-Myers Squibb, AstraZeneca, Lundbeck, Novartis, and Eli Lilly. Dr. Heres participated in clinical trials sponsored or supported by Eli Lilly, Janssen-Cilag, Johnson & Johnson, Bristol-Myers Squibb, AstraZeneca, Lundbeck, Novartis, Servier, Pierre Fabre, Pfizer, Roche, Shire, and Merck. Prof. Stefan Leucht has received lecture honoraria and functioned as advisory board member or consultant from/for Janssen-Cilag, Sanofi-Aventis, Bristol-Myers Squibb, Eli Lilly and company, GlaxoSmithKline, H. Lundbeck A/S, Pfizer Inc., Sanofi-Aventis, and Johnson & Johnson. He received lecture honoraria from AstraZeneca and EssexPharma and research grants from Eli Lilly and Sanofi-Aventis.
Rights and permissions
About this article
Cite this article
Heres, S., Cirjaliu, D.M., Dehelean, L. et al. The SWITCH study: rationale and design of the trial. Eur Arch Psychiatry Clin Neurosci 266, 513–521 (2016). https://doi.org/10.1007/s00406-015-0624-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-015-0624-y