Abstract
Background
Early non-response is a well-established prognostic marker but evidence-based and consistent recommendations to manage it are limited. The aim of this systematic review and meta-analysis was to generate evidence-based strategies for the management of schizophrenia patients with early non-response to 2 weeks of antipsychotic treatment.
Methods
We conducted a systematic review and meta-analysis of randomized trials comparing antipsychotic dose escalation, switch, augmentation and continuation in individuals with study-defined early antipsychotic treatment non-response. Eligibility criteria were (1) clinical trials of primary psychosis treating for at least 2 weeks with antipsychotic monotherapy with study-defined operationalized criteria for early non-response; and (2) randomization to at least two of the following treatment strategies: dose escalation, switch, augmentation, or treatment continuation. Information sources were Pubmed, PsycINFO, and EMBASE, and risk of bias was assessed using Jadad scores. Results were synthesized using random-effects meta-analysis, comparing each intervention with treatment continuation for total symptom change as the primary outcome, generating standardized mean differences (SMDs) and 95% confidence intervals (CIs). Studies meeting the selection criteria but providing insufficient data for a meta-analysis were presented separately.
Results
We screened 454 records by 1 August 2022, of which 12 individual datasets met the inclusion criteria, representing 947 research participants. Of those studies, five provided data to include in the meta-analysis (four with early non-response at 2 weeks, one at 3 weeks). Early non-response was defined within a timeline of 2 weeks in eight datasets, with the remaining datasets ranging between 3 and 4 weeks. The rates of early non-response ranged between 72.0 and 24.1%, and the endpoint ranged within 4–24 weeks post randomization. Quality was good (i.e., Jadad score of ≥3) in 8 of the 12 datasets. Overall, three studies compared antipsychotic switch versus continuation and two compared antipsychotic switch versus augmentation, in both cases without significant pooled between-group differences for total symptom severity (n = 149, SMD 0.18, 95% CI −0.14 to 0.5). Individually, two relatively large studies for antipsychotic switch versus continuation found small advantages for switching antipsychotics for total symptom severity (n = 149, SMD −0.49, 95% CI −1.05 to −0.06). One relatively large study found an advantage for dose escalation, although this finding has not been replicated and was not included in the meta-analysis. None of the alternatives included antipsychotic switch to clozapine.
Conclusions
Despite robust accuracy of early antipsychotic non-response predicting ultimate response, the evidence for treatment strategies that should be used for early non-response after 2–3 weeks is limited. While meta-analytic findings were non-significant, some individual studies suggest advantages of antipsychotic switch or dose escalation. Therefore, any conclusions should be interpreted carefully, given the insufficient high-quality evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Early antipsychotic treatment non-response at 2–3 weeks is a marker of ultimate non-response that has been validated in previous studies. |
Preliminary meta-analytic findings suggest that neither dose escalation, switching, nor augmentation were superior to continuation, although switches to clozapine were not studied and the number of studies and participants was small. |
More randomized controlled studies are needed before clinical recommendations can be made as to which is the best strategy when encountering early antipsychotic treatment non-response. |
1 Introduction
Psychotic disorders affect up to 3% of the population worldwide and are associated with great personal and societal burden [1]. While antipsychotic drugs are the cornerstone of the treatment of psychoses [2], clinical response to these drugs is variable [3, 4]. Given this heterogeneity in treatment response, it is important to develop prognostic tools and/or biomarkers to predict the efficacy of antipsychotic drugs to shorten the duration of ineffective treatments and plan appropriate treatment strategies accordingly.
The development of such predictive tools is currently underway using both neurobiological and clinical research. While significant progress has been made for the use of neuroimaging prognostic biomarkers of treatment response in psychoses [5, 6], clinical information may show predictive abilities with acceptable sensitivity and specificity. In particular, failure to at least minimally respond to antipsychotic treatment during the initial weeks of treatment has been validated as a prognostic marker of treatment response. In a meta-analysis of 43 studies, Samara et al. [7] measured and meta-analyzed the predictive metrics of early non-response on ultimate treatment response. The authors found that improvements in psychotic symptom severity <20% (which is consistent with less than minimally improved) on the Clinical Global Impression (CGI) scale [8] after 2 weeks of antipsychotic treatment had a specificity of 86% and a negative predictive value of 90% in predicting ultimate antipsychotic treatment failure at the end of the respective study period. In this meta-analysis, the predictive ability of early non-response was very consistent across study populations and characteristics [7]. Such low likelihood of antipsychotic treatment response in patients who do not even minimally improve during the initial 2 weeks of treatment has resulted in recommendations to shorten the treatment duration for these individuals in recently updated guidelines [9, 10]. However, despite the consistent data supporting this clinical recommendation, what the next treatment step is in this clinical scenario has been studied less. New evidence-based recommendations are necessary to orient patients, clinicians, and other stakeholders in the management of early antipsychotic treatment non-response.
For the management of psychosis in individuals with poor response to a full trial of antipsychotics, clinical practice guidelines advise against dose escalation, given the limited efficacy of this strategy and the possible greater risk of dose-dependent adverse effects [9,10,11]. Switching to a different antipsychotic has been studied in multiple occasions with controversial results [12]. Most recently, the Optimization of Treatment and Management of Schizophrenia in Europe (OPTiMiSE) trial found that switching had limited efficacy for the treatment of patients who had failed an antipsychotic trial [13]. Similarly, a large overview of meta-analyses recommended against the use of polypharmacy in patients with schizophrenia in those with poor initial treatment response [14]. Furthermore, there is a lack of evidence for antipsychotic polypharmacy in insufficient treatment response [15]. While these management strategies have been studied in patients who fail an antipsychotic trial for a reasonable time and duration, these recommendations may not apply to individuals with early antipsychotic treatment non-response, for whom the change in strategy would occur much earlier.
In order to inform the clinical management of early antipsychotic non-response with evidence-based interventions, we conducted a systematic review and meta-analysis of the efficacy of antipsychotic dose escalation, augmentation, and switch compared with treatment continuation for the treatment of individuals with schizophrenia whose psychotic symptoms did not improve at least minimally during the initial 2 weeks of an acute trial with an antipsychotic. We hypothesized that continuing the initially ineffective antipsychotic treatment would be inferior to one or more of the alternative treatment strategies.
2 Methods
We conducted a systematic literature review to identify articles that met our eligibility criteria (see below) following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for systematic reviews [16]. Once the datasets meeting the eligibility criteria were identified, we proceeded to extract data separately for each trial. If data necessary to conduct a meta-analysis were not available, the articles were commented on separately from the meta-analysis in a descriptive review. To meta-analyze data, it is necessary to have two or more studies comparing the same strategy for which data on effect size and variance are reported.
2.1 Eligibility Criteria
We included studies in which patients with schizophrenia or related disorders (schizoaffective, schizophreniform disorder, psychosis not otherwise specified) were treated for at least 2 weeks with antipsychotic drugs in monotherapy and had defined criteria for early non-response. Furthermore, eligible studies had to randomize, in a double-blind fashion, the subjects who met the criteria for early antipsychotic non-response to at least two of the following: (1) dose escalation; (2) augmentation with another psychotropic medication; (3) switching to another antipsychotic; or (4) treatment continuation.
2.2 Study Selection and Data Extraction
A systematic data search was conducted independently and in duplicate, with a last update on 1 August 2022 by two authors (JR and DG) using the following search terms: “(schizophrenia OR psychosis OR schizophreniform OR schizoaffective) AND (‘early response’ OR ‘early nonresponse’ OR ‘early non-response’ OR ‘early improvement’)” separately in Pubmed, PsycINFO and EMBASE. The authors conducting the study screening were masked from each other’s results and worked independently. Any discrepancy regarding ultimately determined study eligibility was resolved by consensus.
Data for the type of strategy, sample size, mean change and standard deviation in the psychopathology scale between baseline and outcome standard deviation were extracted to meta-analyze the data for each arm separately. In addition, data about the study characteristics were extracted. Risk of bias of each individual study was measured using the Jadad score, a validated rating scale for the measurement of risk of bias in clinical trials [17]. The mean Jadad score was calculated for each of the strategies for which data were meta-analyzed based on the score of the article from which they were derived.
2.3 Statistical Analyses
First, we calculated standardized mean differences (SMDs) for each comparison. For this, we used the Cohen’s d formula of the difference between the two means divided by the pooled standard deviation. The data points for this calculation were the mean difference in change in symptoms between baseline and endpoint. With these estimates of SMDs and the reported variance data for each study group and each psychopathology symptom domain, we proceeded to pool the data for each strategy using a random-effects meta-analysis based on a linear (mixed-effects) model framework. 95% confidence intervals (CI) were obtained in the meta-analytic model, and the cut-off for statistical significance was set at α < 0.05. Analyses were performed using the ‘metafor’ package in R [18].
3 Results
3.1 Study Characteristics
A systematic search of the literature yielded a total of 215 unique references, of which 10 publications corresponding to 12 individual datasets met our eligibility criteria, of which five datasets provided sufficient meta-analyzable data—three for the comparison of antipsychotic switch versus continuation and two for the comparison of antipsychotic switch versus augmentation, each involving a second antipsychotic (Fig. 1). All the studies set the symptom threshold as being less than minimally improved and the time threshold at 2 weeks, except for one study that did so at 3 weeks. In these studies, early non-response rates ranged between 24.1% and 72.4%, with sample sizes ranging from n = 14 to n = 378, with only two studies with n > 100. The antipsychotic used prior to determination of early non-response was risperidone in five studies, olanzapine in three studies, and amisulpride, lurasidone, quetiapine or a first-generation antipsychotic in one study each. The strategies to which individuals were randomized were most often antipsychotic continuation versus switch (six datasets), followed by antipsychotic augmentation versus switch (three datasets), antipsychotic dose increase versus augmentation (one dataset), and antipsychotic continuation versus dose increase (one dataset). The endpoint was within 6–24 weeks after trial onset in all trials. Between 33.6% and 83.4% of the early non-response samples were female, participant’s age at baseline ranged from 29.4 to 49.0 years. The Positive and Negative Syndrome Scale (PANSS) was used in all trials and the baseline total PANSS severity score ranged between 91.2 and 121.2. None of the strategies involved clozapine, and none of the studies involved first-episode psychosis or early-onset psychosis in patients younger than 18 years of age (Table 1).
The quality of the studies ranged between the maximum Jadad score of 5 and 1 point. While all the included studies randomized patients determined to have early antipsychotic non-response, few studies provided details about the randomization or masking process. Studies that were included in the meta-analysis had an average Jadad score of 3.5, while the remaining studies had an average Jadad score of 2.6.
3.2 Meta-Analyzed Comparisons between Strategies
3.2.1 Antipsychotic Switch versus Continuation
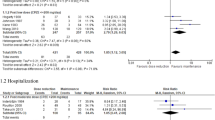
Pooling across the three datasets (n = 149) that randomized early antipsychotic non-responders to either antipsychotic switching or continuation on the same treatment after 2 weeks of non-response, the results were non-significant in all analyses. This included an SMD of 0.18 (95% CI −0.14 to 0.5) for the PANSS total, SMD −0.01 (95% CI −0.33 to 0.31) for PANSS positive, SMD 0.29 (95% CI −0.04 to 0.61) for PANSS negative, and SMD 0.26 (95% CI −0.06 to 0.59) for PANSS general, where positive values favor antipsychotic switching over continuation of treatment (Fig. 2).
3.2.2 Antipsychotic Switch versus Augmentation
There were two datasets (n = 51) that randomized early antipsychotic non-responders to either antipsychotic switching or augmentation. The pooled results were non-significant in all analyses. This included an SMD of −0.49 (95% CI −1.05 to −0.06) for PANSS total, SMD −0.42 (95% CI −0.98 to −0.13) for PANSS positive, SMD −0.11 (95% CI −0.66 to 0.44) for PANSS negative, and SMD −0.44 (95% CI −0.99 to 0.12) for PANSS general, where negative values favor antipsychotic augmentation and positive values favor switching (Fig. 3).
3.3 Narrative Review
The comparison for which there was a greater number of datasets was antipsychotic continuation versus switch, with a total of seven datasets. Of these studies, four were not included in the meta-analysis as they did not provide data on baseline and/or endpoint symptom severity scores. None of the studies not included in the meta-analyses individually found significant differences between continuing antipsychotic treatment after early non-response during the initial weeks and switching to another antipsychotic. In an open-label clinical trial of similar design, Suzuki and colleagues [19] compared switching between olanzapine, quetiapine or risperidone for non-responders at 4 weeks with either of these drugs. The results indicated that switching to risperidone or olanzapine for early antipsychotic non-response was significantly better than switching to quetiapine. In another study, Kinon et al. [20] studied 156 patients with early non-response to 4 weeks of fluphenazine 20 mg/day randomization to dose escalation to 80 mg/day or switching to haloperidol 20 mg/day. No significant difference in response to treatment was detected for either antipsychotic switching or dose escalation compared with either each other or with treatment continuation. In another study conducted by Shalev and colleagues [21], patients were assigned to either haloperidol, levomepromazine or perphenazine, and those who did not improve at 4 weeks were randomly switched to another of these drugs. The differences in improvement rates across switches for patients with early non-response were not statistically significant. However, two relatively large studies by Kinon et al. [22] and Heres et al. [23], respectively, which also had the highest Jadad scores compared with the three small studies, showed small but significant advantages for the antipsychotic switching condition over continuation. In the first of these studies, switching from risperidone to olanzapine resulted in small relative gains at week 12 (PANSS total −3.49; p = 0.020), although those switching to olanzapine also showed significant increments in triglycerides and weight gain. In the second of these studies, where the switch was in both directions between olanzapine and amisulpride, there was a greater difference for antipsychotic switch in either direction compared with staying on the same antipsychotic (odds ratio for symptom remission 3.01, 95% CI 1.35–6.72), with significant differences in some secondary psychopathology outcomes (PANSS negative −1.91, 95% CI −3.7 to −0.12; CGI −0.34, 95% CI −0.64 to −0.05), but not in other important secondary outcomes (i.e., PANSS total or positive scores).
The other comparison that has been studied in a relatively large study (n = 98) is antipsychotic dose escalation versus continuation in a study conducted by Loebel et al. [24], although these findings have not yet been replicated in other datasets. In this study, individuals who failed to improve their total PANSS by ≥20% on lurasidone 80 mg/day were re-randomized to either staying at 80 mg/day or doubling the dose to 160 mg/day. Those individuals who were re-randomized to the high dose showed a moderate effect size in total symptom change (SMD 0.52, p < 0.05), while the early non-responders staying on the lurasidone 80 mg/day dose had numerically even lower PANSS total change than patients in the included placebo arm. Nevertheless, the change in CGI-Severity (SMD 0.44; p = 0.052) fell short of statistical significance for the antipsychotic dose escalation versus dose continuation arm. In this study, dose escalation within the approved dose range was generally well tolerated.
Other comparisons were performed generally with smaller studies with greater exposure to bias. For instance, dose escalation of risperidone was compared against augmentation of risperidone with olanzapine in 26 patients [25], but without significant differences between these two treatment strategies. Similarly, another study by Hatta et al. [26] reported two datasets for which early non-responders to olanzapine or risperidone were randomized to either switching between these two drugs or combining them in augmentation. In each of the two datasets included in this publication, the primary outcome was time to treatment discontinuation, whereas a secondary outcome was symptom severity. In this study, with 24–27 subjects per treatment arm, no statistically significant differences were observed between the various treatment alternatives for early non-responders after the first 2 weeks of antipsychotic treatment.
4 Discussion
In a systematic review of studies comparing the efficacy of antipsychotic augmentation, dose escalation, switch, or continuation for the management of early antipsychotic non-response in patients with schizophrenia spectrum disorders, we identified 12 studies, of which only five provided sufficient data for a strategy-based meta-analysis. Most of the studies were relatively small, with substantial exposure to potential bias. Switch was the strategy with more available data. Most of the switches were performed between agents that were pharmacologically relatively dissimilar (i.e., olanzapine to sulpiride, or risperidone to olanzapine), although in one small study, switches were between less dissimilar agents (i.e., haloperidol to perphenazine). Interestingly, none of the switches were to clozapine, the only antipsychotic approved and recommended consistently by guidelines for treatment-resistant schizophrenia after two full, at least 6-week antipsychotic trials [27, 28]. This finding is particularly remarkable since most of the data converged in pointing out small, if any, advantages of switching to another drug if there was no response within the initial 2–4 weeks of antipsychotic treatment, which suggests high rates of treatment resistance among this population. Indeed, the meta-analysis of eligible studies did not show any significant difference between antipsychotic switch and continuation or between antipsychotic switch and augmentation.
The studies with the largest sample sizes and lower exposure to potential bias [22,23,24] converged in finding individually statistically significant advantages for either antipsychotic switching or dose escalation versus antipsychotic continuation. However, these differences tended to be relatively small and did not expand to all outcomes of interest, while in some cases involved a greater cost in terms of adverse effects that may not necessarily be justifiable given the small advantage in symptom improvement. However, one needs to bear in mind that the results were based on mean group scores and that patient subgroups may have larger benefits, and that those may not necessarily all be those with adverse effect disadvantages. Thus, more data are needed, including analyses that contrast groups with greater benefits, i.e., treatment responders, and those with greater or specific adverse effect burden.
Limitations of some of the included studies include the relatively short follow-up duration, with some authors arguing for future trials needing to expand beyond 8 weeks of duration [23], which may find greater advantages for the alternatives to continuing antipsychotic treatment. Another relevant challenge that these trials may have faced is the potential of non-adherence with oral medication. None of the lead-in phases or treatment alternatives after early antipsychotic non-response used long-acting injectable antipsychotics that ensure antipsychotic intake [29], or other methods to check for treatment adherence, such as antipsychotic plasma levels [30]. Apparent residual psychosis or insufficient treatment response has been well documented in the context of suboptimal treatment adherence [31]. Thus, it is possible that, at least in part, suboptimal adherence could have been related to early non-response in the first place, as well as for the lack of separation between treatment strategies after randomization. Although most of the included studies were conducted in the inpatient setting, designs that involve the use of long-acting injectable antipsychotics could be reassuring in excluding the confounder of non-adherence [32]. The role of non-adherence in both early non-response and subsequent response after randomization is also particularly relevant since, allegedly, a proportion of those patients with early antipsychotic non-response could ultimately meet the criteria for treatment resistance [28]. Arguably, part of the obstacle in conducting studies that randomize early non-responding patients to clozapine are the common, as well as some rare but potentially serious, adverse effects of clozapine treatment [33], which could render switching premature if there is a possibility of late response to an antipsychotic with a more benign adverse effect profile, or if the lack of response is the result of suboptimal adherence [31]. However, in future studies, the switch to clozapine after early antipsychotic non-response could be justified by the high sensitivity and specificity of early non-response as a predictor of ultimate non-response [7], as well as by antipsychotic plasma levels that could eliminate non-adherence as a cause of suboptimal response. Given the serious consequences of treatment resistance [34] and evidence for the decreased efficacy of clozapine when its use is delayed [35], it would be valuable to study the efficacy of switching to clozapine after early non-response more systematically, especially when none of the alternatives has shown clear advantages in the past.
Moreover, in parallel to this work, data that explore the predictive metrics of early non-response for ultimately meeting treatment-resistance criteria [28] seems very necessary, given the inordinate delays in the initiation of clozapine among those for whom it may be the only indicated treatment [36]. If early antipsychotic non-response turns out to be a clinically useful marker of the risk of treatment resistance, it could facilitate the earlier implementation of clozapine treatment, which is underutilized and whose utilization varies greatly, both worldwide [37] and in the US [38]. Furthermore, the development of early antipsychotic non-response and differential response to subsequent interventions, including clozapine, could also be studied along with neurobiological biomarkers [5, 6] to optimize the accuracy of predictions of treatment response and resistance in schizophrenia [39]. Similarly, combining clinical and neurobiological predictors has optimized the accuracy of predictions of conversion from clinical high-risk to full-blown psychosis [40], which could serve as a model. Furthermore, a better understanding of the accuracy of the prediction of early antipsychotic non-response for meeting full treatment-resistant schizophrenia criteria would be important to reconcile the timeframes for each of these clinical definitions, since individuals with early antipsychotic non-response to two different trials would still technically not meet the Treatment Response and Resistance in Psychosis (TRRIP) criteria for treatment resistance that would require two failed antipsychotic trials of at least 6 weeks at a therapeutical dose [28], leaving these cases currently in diagnostic limbo.
Another consideration that should be taken into account is that despite the excellent accuracy of predicting ultimate antipsychotic non-response by early non-response [7], some studies have challenged the need to change treatment early, highlighting the phenomenon of later-onset response in a minority of individuals. For example, in a first episode treatment trial with either olanzapine or risperidone, Gallego and colleagues [41] found that about 25% of patients responded between weeks 8 and 16 of treatment, not finding sufficient accuracy of early non-response to be clinically meaningful in this particular study or first-episode population per se. These apparently conflicting data suggest heterogeneity in time to response across individuals and, possibly, illness phases [42]. This is an intriguing line of research, given the consistent data showing that effects of antipsychotic drugs can be measured very early on in their use [43, 44]. Thus, future research into the factors that explain the variance in time to treatment response, including potential non-adherence or pharmacokinetics/ultra-rapid metabolizer status leading to suboptimal antipsychotic blood levels [45], seem necessary to ultimately validate early antipsychotic non-response as a clinically useful marker that should prompt specific treatment steps.
The results of this study need to be interpreted within its limitations. First, these include the limited number of mostly small studies testing treatment strategies in individuals with early antipsychotic non-response. Second, data in first-episode and early-onset schizophrenia spectrum samples are currently absent. Third, although early non-response was generally defined homogeneously as a total symptom reduction <20% or less than minimally improved on a global rating scale, the time point defining early non-response ranged from week 2 (all studies included in the meta-analysis] to 3 and 4 weeks after antipsychotic initiation (in studies covered in the narrative review). Fourth, adherence was not assured as no long-acting antipsychotics were included nor antipsychotic blood levels measured, which introduces the potential bias of insufficient antipsychotic response due to insufficient adherence. Fifth, our analyses do not factor in the risk/benefit ratio between efficacy and adverse effects for each of the included treatment strategies. Sixth, follow-up durations after the initiation of a treatment strategy after early antipsychotic non-response may not have been sufficiently long in all cases to be certain that the maximum effect could have been observed. Finally, although at least a subgroup of patients with early antipsychotic non-response could be treatment-resistant, no study investigated the merits of a switch to clozapine, especially in multi-episode patients with a history of insufficient prior antipsychotic response.
Taken together, based on the results of this systematic review and exploratory meta-analysis, the recommendations to clinicians should be cautious, given the limitations of these data. Although the positive predictive value previously found for early antipsychotic non-response is robust enough to recommend to not continue treatment beyond 2 weeks in the event of non-response [9, 10], no strong recommendations can be made as to what the next step should be. Antipsychotic switching or dose escalation may have some advantages, although these are probably small. Other aspects such as the confirmation of adherence and factors affecting pharmacodynamics during the initial treatment trial are also important, as well as considerations about the adverse effects of either antipsychotic switching or dose increase, given the limited expected gains in efficacy based on the current limited evidence base. Finally, clinicians should consider the possibility of treatment-resistant schizophrenia in at least some of these individuals, and clozapine should be considered once treatment-resistance criteria are met [28].
5 Conclusion
The data on how to manage early antipsychotic non-response are still rather limited, and consequently no strong clinical treatment recommendations can be made at this point. Some individual data favor antipsychotic dose increase and switching, although the gains, at least at group levels, seem to be relatively small. Future research is clearly necessary to better understand the relationship between early antipsychotic non-response and best next treatment steps as well as the presence or development of treatment resistance, including the role of clozapine in the management of these individuals.
References
Charlson FJ, Ferrari AJ, Santomauro DF, et al. Global epidemiology and burden of Schizophrenia: findings from the global burden of disease study 2016. Schizophr Bull. 2018;44(6):1195–203. https://doi.org/10.1093/schbul/sby058.
Kahn RS, Sommer IE, Murray RM, et al. Schizophrenia. Nat Rev Dis Primer. 2015;2:15067. https://doi.org/10.1038/nrdp.2015.67.
McCutcheon RA, Pillinger T, Efthimiou O, et al. Reappraising the variability of effects of antipsychotic medication in schizophrenia: a meta-analysis. World Psychiatry. 2022;21(2):287–94. https://doi.org/10.1002/wps.20977.
Winkelbeiner S, Leucht S, Kane JM, Homan P. Evaluation of differences in individual treatment response in schizophrenia spectrum disorders: a meta-analysis. JAMA Psychiat. 2019;76(10):1063–73. https://doi.org/10.1001/jamapsychiatry.2019.1530.
Sarpal DK, Argyelan M, Robinson DG, et al. Baseline striatal functional connectivity as a predictor of response to antipsychotic drug treatment. Am J Psychiatry. 2016;173(1):69–77. https://doi.org/10.1176/appi.ajp.2015.14121571.
Li A, Zalesky A, Yue W, et al. A neuroimaging biomarker for striatal dysfunction in schizophrenia. Nat Med. 2020;26(4):558–65. https://doi.org/10.1038/s41591-020-0793-8.
Samara MT, Leucht C, Leeflang MM, et al. Early improvement as a predictor of later response to antipsychotics in schizophrenia: a diagnostic test review. Am J Psychiatry. 2015;172(7):617–29. https://doi.org/10.1176/appi.ajp.2015.14101329.
Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel RR. What does the PANSS mean? Schizophr Res. 2005;79(2–3):231–8. https://doi.org/10.1016/j.schres.2005.04.008.
Remington G, Addington D, Honer W, Ismail Z, Raedler T, Teehan M. Guidelines for the pharmacotherapy of schizophrenia in adults. Can J Psychiatry. 2017;62(9):604–16. https://doi.org/10.1177/0706743717720448.
Keepers GA, Fochtmann LJ, Anzia JM, et al. The American psychiatric association practice guideline for the treatment of patients with schizophrenia. Am J Psychiatry. 2020;177(9):868–72. https://doi.org/10.1176/appi.ajp.2020.177901.
Hasan A, Falkai P, Wobrock T, et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, part 1: update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J Biol Psychiatry. 2012;13(5):318–78. https://doi.org/10.3109/15622975.2012.696143.
Buckley PF, Correll CU. Strategies for dosing and switching antipsychotics for optimal clinical management. J Clin Psychiatry. 2008;69(Suppl 1):4–17.
Kahn RS, van Winter RI, Leucht S, et al. Amisulpride and olanzapine followed by open-label treatment with clozapine in first-episode schizophrenia and schizophreniform disorder (OPTiMiSE): a three-phase switching study. Lancet Psychiatry. 2018;5(10):797–807. https://doi.org/10.1016/S2215-0366(18)30252-9.
Correll CU, Rubio JM, Inczedy-Farkas G, Birnbaum ML, Kane JM, Leucht S. Efficacy of 42 pharmacologic cotreatment strategies added to antipsychotic monotherapy in schizophrenia: systematic overview and quality appraisal of the meta-analytic evidence. JAMA Psychiat. 2017;74(7):675–84. https://doi.org/10.1001/jamapsychiatry.2017.0624.
Galling B, Roldán A, Hagi K, Rietschel L, Walyzada F, Zheng W, et al. Antipsychotic augmentation vs monotherapy in schizophrenia: systematic review, meta-analysis and meta-regression analysis. World Psychiatry. 2017;16(1):77–89.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7): e1000097. https://doi.org/10.1371/journal.pmed.1000097.
Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. https://doi.org/10.1016/0197-2456(95)00134-4.
R Core Team (2020). R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing. URL https://www.R-project.org/.
Suzuki T, Uchida H, Watanabe K, et al. How effective is it to sequentially switch among Olanzapine, Quetiapine and Risperidone? A randomized, open-label study of algorithm-based antipsychotic treatment to patients with symptomatic schizophrenia in the real-world clinical setting. Psychopharmacology. 2007;195(2):285–95. https://doi.org/10.1007/s00213-007-0872-2.
Kinon BJ, Kane JM, Johns C, et al. Treatment of neuroleptic-resistant schizophrenic relapse. Psychopharmacol Bull. 1993;29(2):309–14.
Shalev A, Hermesh H, Rothberg J, Munitz H. Poor neuroleptic response in acutely exacerbated schizophrenic patients. Acta Psychiatr Scand. 1993;87(2):86–91. https://doi.org/10.1111/j.1600-0447.1993.tb03335.x.
Kinon BJ, Chen L, Ascher-Svanum H, et al. Early response to antipsychotic drug therapy as a clinical marker of subsequent response in the treatment of schizophrenia. Neuropsychopharmacol. 2010;35(2):581–90. https://doi.org/10.1038/npp.2009.164.
Heres S, Cordes J, Feyerabend S, et al. Changing the antipsychotic in early nonimprovers to amisulpride or olanzapine: randomized, double-blind trial in patients with schizophrenia. Schizophr Bull. 2022;48(6):1273–83. https://doi.org/10.1093/schbul/sbac068.
Loebel A, Silva R, Goldman R, et al. Lurasidone dose escalation in early nonresponding patients with schizophrenia: a randomized placebo-controlled study. J Clin Psychiatry. 2016;77(12):1672–80. https://doi.org/10.4088/JCP.16m10698.
Hatta K, Otachi T, Sudo Y, et al. A comparison between augmentation with olanzapine and increased risperidone dose in acute schizophrenia patients showing early non-response to risperidone. Psychiatry Res. 2012;198(2):194–201. https://doi.org/10.1016/j.psychres.2012.01.006.
Hatta K, Otachi T, Fujita K, et al. Antipsychotic switching versus augmentation among early non-responders to risperidone or olanzapine in acute-phase schizophrenia. Schizophr Res. 2014;158(1–3):213–22. https://doi.org/10.1016/j.schres.2014.07.015.
Correll CU, Martin A, Patel C, et al. Systematic literature review of schizophrenia clinical practice guidelines on acute and maintenance management with antipsychotics. NPJ Schizophr. 2022;8(1):5. https://doi.org/10.1038/s41537-021-00192-x.
Howes OD, McCutcheon R, Agid O, et al. Treatment-resistant schizophrenia: treatment response and resistance in psychosis (TRRIP) working group consensus guidelines on diagnosis and terminology. Am J Psychiatry. 2017;174(3):216–29. https://doi.org/10.1176/appi.ajp.2016.16050503.
Correll CU, Citrome L, Haddad PM, et al. The use of long-acting injectable antipsychotics in schizophrenia: evaluating the evidence. J Clin Psychiatry. 2016;77(Suppl 3):1–24. https://doi.org/10.4088/JCP.15032su1.
Lopez LV, Shaikh A, Merson J, Greenberg J, Suckow RF, Kane JM. Accuracy of clinician assessments of medication status in the emergency setting: a comparison of clinician assessment of antipsychotic usage and plasma level determination. J Clin Psychopharmacol. 2017;37(3):310–4. https://doi.org/10.1097/JCP.0000000000000697.
McCutcheon R, Beck K, D’Ambrosio E, et al. Antipsychotic plasma levels in the assessment of poor treatment response in schizophrenia. Acta Psychiatr Scand. 2018;137(1):39–46. https://doi.org/10.1111/acps.12825.
Rubio JM, Schoretsanitis G, John M, et al. Psychosis relapse during treatment with long-acting injectable antipsychotics in individuals with schizophrenia-spectrum disorders: an individual participant data meta-analysis. Lancet Psychiatry. 2020;7(9):749–61. https://doi.org/10.1016/S2215-0366(20)30264-9.
Bak M. Monitoring clozapine adverse effects calls for the integration of protocol and good clinical practice. J Clin Psychiatry. 2012;73(10):1313–4. https://doi.org/10.4088/JCP.12com07964.
Kane JM, Agid O, Baldwin ML, et al. Clinical Guidance on the Identification and Management of Treatment-Resistant Schizophrenia. J Clin Psychiatry. 2019;80(2):18123. https://doi.org/10.4088/JCP.18com12123.
Nielsen J, Nielsen RE, Correll CU. Predictors of clozapine response in patients with treatment-refractory schizophrenia: results from a Danish Register Study. J Clin Psychopharmacol. 2012;32(5):678–83. https://doi.org/10.1097/JCP.0b013e318267b3cd.
Thien K, O’Donoghue B. Delays and barriers to the commencement of clozapine in eligible people with a psychotic disorder: a literature review. Early Interv Psychiatry. 2019;13(1):18–23. https://doi.org/10.1111/eip.12683.
Bachmann CJ, Aagaard L, Bernardo M, et al. International trends in clozapine use: a study in 17 countries. Acta Psychiatr Scand. 2017;136(1):37–51. https://doi.org/10.1111/acps.12742.
Bareis N, Olfson M, Wall M, Stroup TS. Variation in psychotropic medication prescription for adults with schizophrenia in the United States. Psychiatr Serv. 2022;73(5):492–500. https://doi.org/10.1176/appi.ps.202000932.
Potkin SG, Kane JM, Correll CU, et al. The neurobiology of treatment-resistant schizophrenia: paths to antipsychotic resistance and a roadmap for future research. NPJ Schizophr. 2020;6(1):1. https://doi.org/10.1038/s41537-019-0090-z.
Koutsouleris N, Kambeitz-Ilankovic L, Ruhrmann S, et al. Prediction models of functional outcomes for individuals in the clinical high-risk state for psychosis or with recent-onset depression: a multimodal, multisite machine learning analysis. JAMA Psychiat. 2018;75(11):1156. https://doi.org/10.1001/jamapsychiatry.2018.2165.
Gallego JA, Robinson DG, Sevy SM, et al. Time to treatment response in first-episode schizophrenia: should acute treatment trials last several months? J Clin Psychiatry. 2011;72(12):1691–6. https://doi.org/10.4088/JCP.10m06349.
Case M, Stauffer VL, Ascher-Svanum H, et al. The heterogeneity of antipsychotic response in the treatment of schizophrenia. Psychol Med. 2011;41(6):1291–300. https://doi.org/10.1017/S0033291710001893.
Ketter TA, Agid O, Kapur S, Loebel A, Siu CO, Romano SJ. Rapid antipsychotic response with ziprasidone predicts subsequent acute manic/mixed episode remission. J Psychiatr Res. 2010;44(1):8–14. https://doi.org/10.1016/j.jpsychires.2009.07.006.
Agid O, Kapur S, Arenovich T, Zipursky RB. Delayed-onset hypothesis of antipsychotic action: a hypothesis tested and rejected. Arch Gen Psychiatry. 2003;60(12):1228–35. https://doi.org/10.1001/archpsyc.60.12.1228.
Schoretsanitis G, Kane JM, Correll CU, et al. Blood levels to optimize antipsychotic treatment in clinical practice: a joint consensus statement of the american society of clinical psychopharmacology and the therapeutic drug monitoring task force of the arbeitsgemeinschaft für neuropsychopharmakologie und pharmakopsychiatrie. J Clin Psychiatry. 2020;81(3):199. https://doi.org/10.4088/JCP.19cs13169.
Woo YS, Park SY, Yoon BH, Choi WS, Wang SM, Bahk WM. Amisulpride augmentation in schizophrenia patients with poor response to olanzapine: a 4-week, randomized, rater-blind, controlled Pilot Study. Clin Psychopharmacol Neurosci. 2022;20(3):567–72. https://doi.org/10.9758/cpn.2022.20.3.567.
Hatta K, Otachi T, Sudo Y, et al. Difference in early prediction of antipsychotic non-response between risperidone and olanzapine in the treatment of acute-phase schizophrenia. Schizophr Res. 2011;128(1–3):127–35. https://doi.org/10.1016/j.schres.2011.02.011.
Loebel A, Citrome L, Correll CU, Xu J, Cucchiaro J, Kane JM. Treatment of early non-response in patients with schizophrenia: assessing the efficacy of antipsychotic dose escalation. BMC Psychiatry. 2015;15:271. https://doi.org/10.1186/s12888-015-0629-0.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Jose M. Rubio was supported in part by grant number K23MH127300. No funding was specifically received for this article.
Author contributions
CUC conceptualized the study; DG and JMR conducted the record search; and JMR conducted the analyses and wrote the first iteration of the manuscript. All co-authors provided meaningful edits to the final version of the manuscript. All authors agree to be accountable for this work.
Conflicts of interest
Jose M. Rubio has been a consultant for Lundbeck, Teva and Janssen, has received research funding from Alkermes, and receives royalties from UpToDate. Daniel Guinart has been a consultant for and/or has received speaker honoraria from Otsuka America Pharmaceuticals, Janssen Pharmaceuticals, Lundbeck and Teva. Christoph U. Correll has been a consultant and/or advisor to, or has received honoraria from, AbbVie, Acadia, Alkermes, Allergan, Angelini, Aristo, Boehringer-Ingelheim, Cardio Diagnostics, Cerevel, CNX Therapeutics, Compass Pathways, Darnitsa, Gedeon Richter, Hikma, Holmusk, IntraCellular Therapies, Janssen/J&J, Karuna, LB Pharma, Lundbeck, MedAvante-ProPhase, MedInCell, Merck, Mindpax, Mitsubishi Tanabe Pharma, Mylan, Neurocrine, Newron, Noven, Otsuka, Pharmabrain, PPD Biotech, Recordati, Relmada, Reviva, Rovi, Seqirus, SK Life Science, Sunovion, Sun Pharma, Supernus, Takeda, Teva, and Viatris; provided expert testimony for Janssen and Otsuka; served on a Data Safety Monitoring Board for Lundbeck, Relmada, Reviva, Rovi, Supernus, and Teva; received grant support from Janssen and Takeda; received royalties from UpToDate; and is a stock option holder of Cardio Diagnostics, Mindpax, LB Pharma and Quantic. John M. Kane has been a consultant for or received honoraria from Alkermes, Forum, Allergan, Genentech, Lundbeck, Intracellular Therapies, Janssen Pharmaceutica, Johnson & Johnson, Merck, Neurocrine, Otsuka, Pierre Fabre, Reviva, Roche, Sunovion, Takeda and Teva; has received grant support from Otsuka Lundbeck and Janssen; and is a shareholder in Vanguard Research, LB PharmaGroup, and LB Pharmaceuticals, Inc.
Availability of data
Not applicable.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rubio, J.M., Guinart, D., Kane, J.M. et al. Early Non-Response to Antipsychotic Treatment in Schizophrenia: A Systematic Review and Meta-Analysis of Evidence-Based Management Options. CNS Drugs 37, 499–512 (2023). https://doi.org/10.1007/s40263-023-01009-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-023-01009-4