Abstract
Despite the fact that alcoholism is a severe public health problem of worldwide proportions, only a limited number of medications is used as coadjuvant treatment. The objectives of this study were to analyse the use of disulfiram for alcohol-dependent patients and the immediate interruption of treatment following medication prescription. This is a transversal study of 810 patients who attended the Alcohol and Drug Research Unit (UNIAD) during the 2000–2006 period. The study showed that both male and female patients who had remained under treatment during the first year used proportionally more disulfiram than those who remained for lesser time under treatment, and immediate treatment interruption was statistically more significant in this latter group of patients after prescription of this medication. Although disulfiram is an old medication, it seems that this drug can be useful for keeping alcohol-dependent patients under outpatient treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alcoholism is one of the relevant health problems worldwide. It is a complex syndrome involving social, psychological, and individual factors that affect the patient at different phases of his or her life, bringing negative and wide repercussions during the course of the disease.
In developing countries like Brazil the consumption of alcoholic beverages is one of the factors associated with several diseases and mortality rates, corresponding to 8–14.9% of all health problems faced by these nations [1].
In Brazil, prevalence of alcohol dependence was estimated to be 17.1% for men and 5.7% for women [2]. Beer is the most widely consumed alcoholic beverage in Brazil, with 54 l per capita/year, followed by cachaça (sugar cane brandy) and wine with, respectively, 12 and 1.8 l per capita/year. In 2005, the beer production was estimated at approximately 9,884 millions litres, whereas cachaça production achieved 1.3 billions litres in 2002. Of these, 14.8 million litres had been exported, placing cachaça as the fourth leading distilled beverage worldwide [3]. In addition, clandestine production of cachaça should not be ignored as it accounts for a significant part of the national market [4]. Alcohol was responsible for about 90% of all hospitalisations resulting from psychoactive substance dependence [5].
The most recent national study on alcohol drinking patterns among Brazilians has shown that the great majority of alcohol drinkers belong to higher social-economic classes and live in the southern states, although the highest alcohol consumption was observed in the poorer classes and among those living in the North, Centre-West, and Northeast regions of the country. In a sample of adult men, 11% reported drinking every day and 28% consumed alcoholic beverages 1–4 times a week. In the Northeast region, 13% of the subjects reported consuming 12 or more doses of alcohol beverages a day. In the same sample, men had withdrawal rate reduced by 40% compared to women, and they consumed more distilled beverages than women did, although wine was preferentially consumed by the latter group [6].
Studies have reported that approximately half of the patients suffering from alcohol dependence syndrome drop out of the treatment a few months later [7, 8], resulting in negative outcomes in terms of clinical evaluation and prognosis, which impedes optimal benefits from the treatment, affecting the quality of life and increasing the health-care costs [9].
Several therapeutic approaches have been tested in recent decades in an attempt to reduce the number of lapses and relapses, which can be one of the barriers impeding treatment continuity, and the discovery of new pharmacological methods becomes object for speculation worldwide.
Pharmacotherapy for treatment of alcoholism
Although alcoholism is considered one of the most severe health problems worldwide, even today only a limited number of medications is available for its treatment.
Acamprosate, which has been approved by Food and Drug Administration (FDA), acts on the GABA-a system, and studies have suggested that this drug has beneficial effects on the relapse rates by blocking the craving [10].
The use of naltrexone, an opioid antagonist, for treatment of alcoholism was approved by FDA in 1995. Studies reveal that this medication can attenuate the pleasurable effects of alcohol, showing that its use either oral or injectable reduced the number of relapses to heavy drinking among alcohol-dependent patients suffering from withdrawal [11, 12].
A double-blind, randomised study comparing acamprosate and naltrexone have shown that the latter was more effective for those patients reporting more craving [13].
Association of acamprosate with naltrexone seems to be efficient and safe for alcohol-dependent patients whose response to treatment using one of the medications is not enough [14].
Disulfiram was the first pharmacological intervention approved by FDA for treatment of alcohol dependence. Of easy administration, this low-cost drug acts by inhibiting aldehyde dehydrogenase (ALDH), enzymes that degrade alcohol at the acetaldehyde stage, causing accumulation of acetaldehyde in the organism which results in an ethanol–disulfiram reaction [15].
Although disulfiram is mostly used because of its aversive action, this drug also acts on the central nervous system by inhibiting the dopamine beta-hydroxylase and increasing the dopamine concentrations in the mesolimbic system. Some patients reported a decrease in their longing for drinking (craving) [16], while other studies found that disulfiram improved treatment retention [17] and prevented relapses [18].
Some medications have not yet been approved by FDA and they need further evaluation for clinical use, such as topiramato, which seems to increase the withdrawal rates modestly [19], and ondansetron, a 5-HT3 antagonist and antiemetic drug that reduces the alcohol consumption in experimental animals [20], thus being proposed for treatment of early alcohol dependence [21].
In virtue of the relevance of this theme, the objective of the present study was to analyse the use of disulfiram among alcohol-dependent patients and the immediate treatment interruption following prescription of medication.
Methods
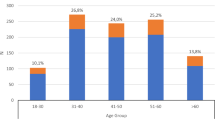
This is a transversal study involving a sample of 810 patients (652 men and 158 women) who were alcohol-dependent according to ICD-10 criteria and had sought treatment in the Alcohol and Drug Research Unit (UNIAD) [22] between 2000 and 2006 for the first time.
The patients were followed up during the first year of treatment and divided into three groups:
-
1.
Group 1: patients remaining under treatment for first month after screening;
-
2.
Group 2: patients remaining under treatment from first month to sixth month;
-
3.
Group 3: patients remaining under treatment from sixth month to 12th month.
The patients were distributed according to the “treatment dropout” criteria, that is, four consecutive non-justified absents. The patients who had abandoned the treatment could return, but only the first participation was recorded.
UNIAD is an outpatient unit linked to the Department of Psychiatry of the Federal University of São Paulo (UNIFESP) whose objectives are related to education, research, prevention, and treatment of abusers of alcohol, tobacco, and other drugs.
Disulfiram was offered to patients presenting with no alcohol withdrawal abstinence syndrome during screening or during the outpatient process of alcohol detoxification in which the patient attended a session every week, with 2–4 sessions on average at the end of the process. For those patients presenting alcohol withdrawal syndrome and who needs specific medication (497 men and 124 women) diazepam was the most used medication (79.6 and 44.5%, respectively), followed by lorazepam (12.2 and 15.3%, respectively).
Prior to the choice of a given medication, each case was evaluated regarding hepatic diseases, pregnancy, cardiac problems, arterial hypertension, diabetes, age, motivation for keeping abstinence, and cognition for understanding the therapeutic goals.
Medical staff was responsible for prescribing the medication (250 mg/day) and the patient was supposed to take it, whereas interdisciplinary personnel were involved in instructing and monitoring the patient every week during group or individual sessions.
Both patient and caregiver, if present, were instructed about the adverse effects resulting from the association between medication and alcohol, including its derivatives, as well as about the 1- to 2-week duration of therapeutic action following interruption of treatment [23]. They have also signed an informed consent form in which they are liable for the consequences if the recommendations are not followed.
This study was previously submitted to the UNIFESP Research Ethics Committee (process # 1627/05).
Chi-square tests were used for statistical analysis at significance level of 0.05.
Results
Table 1 shows that the proportion of patients of Group 1 who took medication is statistically lower than that of other groups, regardless of gender.
Table 2 shows that immediate dropout of treatment following prescription of disulfiram is statistically higher in Group 1 compared to other groups for both men and women.
Discussion
Despite being an “old” medication and largely used for treatment of alcoholism in Brazil, little is known about disulfiram regarding its effectiveness and usage in terms of gender.
Medication is part of the treatment and in association with other types of therapy its efficacy can be increased. One of the few studies associating treatment duration with alcohol abuse among women showed that disulfiram was directly related to a higher outpatient treatment retention (Elbreder et al. 2008) [24].
The present study showed that patients, regardless of gender, remaining under treatment during the first year of study had used proportionally more disulfiram compared to those patients dropping out the treatment.
The majority of patients seeking this health care service present with severe alcohol dependence, most belonging to disfavoured social-economical classes with low levels of education and professional qualification. Because disulfiram is a low-cost and easy-to-use medication, it was the coadjuvant treatment chosen by those patients desiring to achieve alcohol abstinence.
Medical ethics issues should be always raised as disulfiram has a series of adverse effects. On the other hand, any intervention that quickly interrupts alcohol consumption in patients with severe alcohol dependence should not be discarded, and the cost–benefits relationship as well as the side effects should also be, respectively, informed and monitored weekly.
According to the literature, dropout rates can be as high as 50% in the first weeks of treatment [25], and this study shows a high rate of patients attending only the first session, which makes any type of treatment or intervention very difficult regardless the use of medication.
Some aspects that can influence the decision whether or not to take medication should be observed: presence of psychiatric comorbidities [26], patient’s motivation during medication prescription [27], empathy between therapist and patient [28], reliability on the proposed treatment plan, and adequate understating of the therapeutic goals on the part of the patient [29]. Those patients who had dropped out of the treatment immediately after medication prescription possibly had one of these related factors.
Therefore, the multidisciplinary staff should not only take care about these factors as they can act as a barrier against any medication treatment, but also know the characteristics of each population in order to ease the treatment planning and achieve successful results [30].
Conclusion
Disulfiram is an important tool for treating alcoholism, but this medication should be understood as part of the therapy instead of being considered as the main treatment. Indeed, disulfiram can help alcohol-dependent patients remain under outpatient treatment, although some factors should be observed prior to medication prescription.
References
The World Health Report (2002) Reducing risks, promoting health life. World Health Organization, Geneva
Carlini E A, Galduróz JCF, Noto AR, Nappo AS (2001) Use of psychotropic drugs in Brazil: household survey in the 107 biggest Brazilian cities–2001. SENAD (Secretaria Nacional Anti-Drogas-Presidência da República), Brasilia
Galduróz JCF, Caetano R (2004) Epidemiology of alcohol use in Brazil. Rev Bras Psiquiatr 26(2):3–6
Laranjeira R, Dunn J (1998) Death by methanol poisoning in Brazil. Addiction 93(7):1103–1106
Noto AR, Moura YG, Nappo AS, Galduróz JCF, Carlini EA (2002) Internações por transtornos mentais e de comportamento decorrentes de substâncias psicoativas: um estudo epidemiológico nacional do período de 1988 a 1999. J Bras Psiquiatr 51(2):113–121
Laranjeira R, Pinsky I, Zaleski M, Caetano R (2007) I Levantamento nacional sobre os padrões de consumo de álcool na população brasileira. SENAD, Brasilia
Stark MJ (1992) Dropping out of substance abuse treatment: a clinically oriented review. Clin Psychol Rev 12:93–116
McKay JR (2005) Is there a care for extended interventions for alcohol and drug use disorders? Addiction 100:1594–1610
Marinker M, Shaw J (2003) Not to be taken as directed: putting concordance for taking medicines into practice. BMJ 326:348–349
Ritson B (2005) ABC of alcohol: treatment for alcohol related problems. BMJ 330(7483):139–141
Johnson BA (2007) Naltrexone long-acting formulation in the treatment of alcohol dependence. Ther Clin Risk Manag 3(5):741–749
Srisurapanont M, Jarusuraisin N (2001) Opioid antagonist for alcohol dependence. Cochrane Review, Cochrane Library, issue 4, Oxford, England (update software)
Richardson K, Baillie A, Reid S, Morley K, Teesson M, Sannibale C et al (2008) Do acamprosate or naltrexone have an effect on daily drinking by reducing craving for alcohol? Addiction 103(6):953–959
Kiefer F, Wiedemann K (2004) Combined therapy: what does acamprosate and naltrexone combination tell us? Alcohol Alcohol 39(6):542–547
Kline AS, Kingstone E (1977) Disulfiram implants: the right treatment but the wrong drug? Can Med Assoc J 116(12):1382–1383
Edwards G, Marshall JE, Cook, CC (1999) O tratamento do alcoolismo–um guia para profissionais da saúde, 3rd edn. Artmed, Porto Alegre
Chandrasekaran R, Sivaprakash B, Chitraleka V (2001) Five years of alcohol de-addiction services in a tertiary care general hospital. Indian J Psychiatry 43:58–60
Hunt RR (2002) How effective are pharmacologic agents for alcoholism? J Fam Pract 51:577
Johnson BA, Rosenthal N, Capece JA, Wiegand F et al (2007) Topiramate for treating alcohol dependence. A randomized controlled trial. JAMA 298(14):1641–1651
Boyce-Rustay JM, Wiedholz LM, Millstein RA, Carroll J, Murphy DL, Daws LC, Holmes A (2006) Ethanol-related behaviors in serotonin transporter knockout mice. Alcohol Clin Exp Res 30:1957–1965
Johnson BA, Roache JD, Ait-Daoud N, Zanca NA, Velasquez M (2002) Ondansetron reduces the craving of biologically predisposed alcoholics. Psychopharmacology (Berl) 160(4):408–413
UNIAD, Unidade de Pesquisa em Álcool e Drogas. Departamento de Psiquiatria. UNIFESP. Disponível em http://www.uniad.org.br
Gelbman F, Epstein NB (1949) Initial clinical experience with antabuse. Can Med Assoc J 60(6):549–552
Elbreder MF, Siqueira MM, Laranjeira R, Barbosa DA (2008) Profile of female alcohol users in specialized outpatient clinic. J Bras Psiquiatr 57(1):9–15
Meier PS, Donmall MC, McElduff P et al (2006) The role of the early therapeutic alliance in predicting drug treatment dropout. Drug Alcohol Depend 83:57–64
Mann K, Hintz T, Jung M (2004) Does psychiatric comorbidity in alcohol-dependent patients affect treatment outcome? Eur Arch Psychiatry Clin Neurosci 254(3):172–181
Armitage CJ (2009) Is there utility in the transtheoretical model? Br J Health Psychol 14(Pt 2):195–210
De Weert-Van Oene GH, De Jong CAJ, Jörg F, Schrijvers AJP (1999) The helping alliance questionnaire: psychometric properties in patients with substance dependence. Subst Use Misuse 34:1549–1569
Moretti F, Goss C, Del Piccolo L (2004) Communication strategies to motivate patients to follow doctor’s advice. Recenti Prog Med 95(2):61–66
Diehl A, Croissant B, Batra A, Mundle G, Nakovics H, Mann K (2007) Alcoholism in women: is it different in onset and outcome compared to men? Eur Arch Psychiatry Clin Neurosci 257(6):344–351
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Elbreder, M.F., de Humerez, D.C. & Laranjeira, R. The use of disulfiram for alcohol-dependent patients and duration of outpatient treatment. Eur Arch Psychiatry Clin Neurosci 260, 191–195 (2010). https://doi.org/10.1007/s00406-009-0038-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-009-0038-9