Abstract
Background
Alcohol dependence remains a major health problem from both a public health and clinical perspective. Harm reduction strategies have been increasingly recognized as suitable treatment goals. Nalmefene has been recently approved for this precise therapeutic indication after completion of phase III trials. However, more data from routine practice settings are needed in order to obtain evidence with high external validity. The aim of this study was to conduct a single-arm, phase IV study with alcohol-dependent outpatients starting nalmefene for the first time.
Methods
An observational, multisite, single-arm, phase IV study was conducted among adult alcohol-dependent outpatients who received nalmefene for the first time. The study consisted of four visits: baseline, 4 weeks (referred to as 1 month hereafter), 6 and 12 months. At each visit, drinking variables were obtained from the Timeline Followback regarding the previous month. Satisfaction with medication was also assessed for both patients and professionals, with the Medication Satisfaction Questionnaire. A repeated measures mixed model was performed for effectiveness analysis regarding drinking outcomes (reduction in total alcohol consumption and number of heavy drinking days). Regression analyses were performed in order to find predictors of response to nalmefene.
Results
A total of 110 patients were included, with 88 reporting data at the 1-month visit. On average, patients took nalmefene 68% of the days. The number of heavy drinking days decreased from 13.5 to 6.8 days/month, and total alcohol consumption decreased from 169 to 79 units. For both outcomes, significant reductions at 1 month were found, with no other significant variables reaching significance. Thirty-seven patients were considered medication responders, but given the high presence of low-risk drinkers in our sample, no significant predictors could be found. Satisfaction was globally high for both professionals and patients, and overall nalmefene was well tolerated, with no serious adverse events reported.
Conclusion
The data provided by this phase IV study suggest nalmefene is an effective, well-tolerated treatment for alcohol dependence in real-world, clinical settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Nalmefene significantly reduced patients’ drinking in the first month, while being well tolerated. |
A great number of patients in real settings display psychiatric comorbidities. This study suggests they also benefit from nalmefene. |
Despite being marketed as an as-needed medication, a majority of patients take nalmefene on a daily basis. |
1 Introduction
Alcohol dependence remains today as a major public health problem, with almost 15 million people affected in the European Union (EU) [1]. Moreover, it is estimated that less than 10% of this collective receive any treatment [2]. Unfortunately, the natural course of alcohol dependence is one of a relapsing-remitting disease, with most affected individuals suffering a relapse in the first 12 months after abstinence has been achieved [3, 4].
Although abstinence has been the prevailing objective in the treatment of alcohol dependence [5], the possibility and convenience of establishing reduction in heavy drinking as a possible goal is now a solid reality [6], since it could be more appropriate for some patients, it has been shown to reduce the annual and lifetime risk of alcohol-related death, and it could attract patients who are currently not inclined to seek treatment or do not accept abstinence as a treatment goal [7,8,9].
In this unsatisfactory panorama, nalmefene emerged as a new compound for the treatment of alcohol dependence. Although its structural characteristics are similar to those of naltrexone, there are some differences. For instance, nalmefene has a greater bioavailability [10, 11], a more effective union to central opioid receptors [12, 13], an absence of dose-dependent hepatic toxicity, and partial agonistic activity at the kappa receptors, which are involved in the cerebral reward system [14]. That being said, it must also be noted that naltrexone has shown efficacy in reducing heavy drinking in many studies and meta-analysis [15], and this has led some authors to argue that real, significant differences between nalmefene and naltrexone are yet to be demonstrated [16].
While evidence supporting nalmefene efficacy already existed prior to its formal approval [17,18,19,20], the three pivotal, phase III studies leading to nalmefene approval demonstrated that nalmefene is efficacious in reducing alcohol consumption in patients with a high-risk drinking level [21,22,23,24].
Notwithstanding, while experimental designs such as those of phase III studies are essential for internal validity assessment and are the cornerstone of drug efficacy assessment, it has been extensively noted in many areas that external validity remains disproportionally neglected [25,26,27]. This fact might yield relevant consequences, such as the fact that patients from experimental settings might differ significantly from patients in real-world settings [28, 29], ultimately jeopardizing the feasibility, applicability, and even the relevance of experimental findings [30].
In this context, previous studies in several diseases, such as hypertension, social anxiety, rheumatoid arthritis, and others [31], have found that phase III and phase IV patients are not always similar, a fact that could have relevant implications. Therefore, we believe it is also necessary to evaluate, in the field of alcohol use disorders, whether patients in “real life” are comparable to patients of previous experimental studies, and what differences might exist. This is in fact one of the reasons leading to the performance of phase IV studies [32]. The present study is a single-arm, phase IV study of nalmefene designed to evaluate its prescription patterns and effectiveness under routine, clinical conditions, as well as patients’ and professionals’ satisfaction with the treatment.
Another relevant issue concerning nalmefene and phase IV trials is adverse events. While most of them in clinical trials have been mild to moderate, there is a need to better assess their presence and intensity in real-world conditions. In fact, phase III clinical trials showed a high rate of adverse events, with nausea, dizziness, headache, and insomnia being the most frequent.
Finally, recent critiques to both nalmefene efficacy and approval cannot be overlooked [33,34,35,36]. It has been argued that the approval of nalmefene was based on biased data from the phase III trials [33]. Similarly, many criticisms have been raised regarding the lack of meaningful differences with naltrexone [34]. Others have again emphasized the results from subgroup analysis and the high drop-out rates from randomized controlled trials [35, 36]. This fact, indeed, makes the effectiveness data provided by this phase IV trial even more necessary and relevant.
The aim of this paper is therefore to report baseline and 1-month results of the phase IV study of nalmefene, which has been designed as a 12-month study.
2 Methods
2.1 Study Design and Participants
An observational, multisite, single-arm, phase IV study was conducted among alcohol-dependent outpatients taking nalmefene for the first time as a treatment for alcohol dependence. To be included, patients had to be adults (≥ 18 years) diagnosed with alcohol dependence according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV TR) or the International Classification of Diseases (ICD-10) criteria who according to routine clinical criteria had been started on nalmefene for the first time. Patients had to be willing to participate and sign informed written consent. The main exclusion criteria, besides those relative to nalmefene contraindications, were any unstable medical or psychiatric condition that, in the opinion of the investigators, would not allow the patient to fulfill the study procedures.
2.2 Procedure
As this was an observational study, the decision to start nalmefene was completely independent of patients’ inclusion into the study. Once clinicians decided to prescribe nalmefene to a patient, study participation was offered if inclusion criteria were met. The study consists of four visits: baseline, 4 weeks (referred to as 1 month hereafter), 6, and 12 months. Study visits are planned to be conducted by the same treating physicians. Patients continue to receive their usual treatment independent of study visits and procedures. Effectiveness and safety assessments were performed at the 1-month visit. At study entry, patients were offered the possibility of using a mobile app in order to record their alcohol and medication use [37, 38].
2.3 Outcome Variables
The main outcome variables of the study were:
-
1.
Reduction in drinking, measured as change from baseline in heavy drinking days and total alcohol consumption (units in the previous 28 days). These data were derived from the Timeline Followback for the previous month [39]. As the study was conducted in Spain, one drink was considered to contain 10 g of pure ethanol. The main efficacy analysis was planned for month 6, although the same analysis was to be carried out at months 1 and 12.
-
2.
Patient and clinician satisfaction, as measured by the Medication Satisfaction Questionnaire (MSQ) [40, 41].
As a secondary outcome, drinking risk level response was measured (defined as a change from very high drinking risk level at baseline to medium drinking risk level or below, or from high or medium drinking risk level at baseline to low drinking risk level or below). For risk categories, World Health Organization (WHO) definitions were used (very high risk: more than 100 g of alcohol per day in men and more than 60 g/day in women; high risk: 60–100 g/day in men and 40–60 g/day in women; medium risk: 40–60 g/day in men and 20–40 g/day in women; low risk: 1–40 g/day in men and 1–20 g/day in women). Changes in liver enzymes were also considered secondary outcomes.
Other collected variables at baseline included previous history of drug use, psychiatric history, family history of drug and alcohol use, and concomitant or changes in psychiatric medication during the study period. All these variables were collected by directly inquiring patients, with no structured questionnaires being used. At the study visit, the number of days that patients took nalmefene was also recorded.
We also defined a profile for responders to medication. To be considered as such, patients had to fulfill any of the two following criteria: (1) reduction in daily alcohol consumption of at least 70% or (2) downshift of two categories in the drinking risk level according to the WHO or shift to low-risk category.
2.4 Sample Size Calculation
The sample size calculation was based on a standard deviation (SD) for the change from baseline in number of heavy drinking days of 7 days and the change from baseline in total alcohol consumption of 45 g/day. With a significance level of 5%, 160 patients would provide a power of 90% for detecting differences between baseline and month 6, accounting for an expected drop-out rate of 10%.
2.5 Statistical Analysis
Descriptive statistics were performed for baseline variables. For effectiveness analysis, the repeated measures linear mixed procedure with random intercepts was used for both heavy drinking days and total alcohol consumption as main outcomes. Age, sex, time (referred to as the difference between baseline and 1-month visit), and number of days taking nalmefene were entered as fixed effects. We also included the presence of any psychiatric comorbidity and the presence of a positive family history of alcohol as covariates. For each main outcome, regression coefficients (b), t values, and p values were calculated. Statistical significance was set at 0.05. Missing data at 1 month for outcome variables was addressed with the conservative approach of baseline observation carried forward (BOCF).
A descriptive analysis of the MSQ at 1 month was conducted. For a better assessment of patients’ satisfaction and possible predictors, the variable was further dichotomized between the two highest ratings and the rest of the categories followed by logistic regression analysis in order to establish potential predictors. Included variables were sex, age, number of days taking nalmefene, presence of comorbid drug use, mean alcohol consumption, and number of heavy drinking days during the first month of the study.
Once the responders had been identified, univariate comparisons were conducted between responders and non-responders regarding drinking and clinical variables, followed by a logistic regression analysis for the detection of significant predictors of response. Included variables were sex, age, number of days taking nalmefene, presence of comorbid drug use, and presence of psychiatric comorbidity. A descriptive analysis of adverse events was also conducted.
3 Results
3.1 Sample
A total of 110 patients were included from four sites in the Spanish region of Catalonia, between 2015 and 2016. Table 1 displays the main sociodemographic characteristics of the sample.
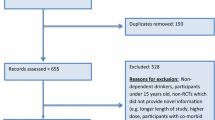
In the month before starting nalmefene, patients had on average 13.5 heavy drinking days and drank on average 60.4 g of alcohol per day. The mean values of liver parameters were within the reference ranges. The vast majority of patients had not previously been treated for either alcohol dependence or alcohol withdrawal symptoms. Two thirds of patients had past or present addictive comorbidities and more than a third a psychiatric comorbidity. A family history of alcohol problems was present in almost half of the sample. A total of 88 patients provided data on the first-month visit. Figure 1 shows a graphic representation of the number of days patients took nalmefene. On average, they took it 19.2 days (SD = 10). Importantly, almost half of the patients took the medication on a daily basis. No overdoses were reported. Fifteen patients reported discontinuation of the treatment (six due to adverse events, four due to change of treatment goal, and five for other reasons).
3.2 Efficacy
The mean number of heavy drinking days decreased from 13.5 to 6.8 days/month. The repeated measures linear mixed model revealed a significant effect of time (b = 8.5, t = 8.14, p < 0.001). The rest of the variables were not statistically significant. For total alcohol consumption, the number of units consumed in the previous 28 days decreased from 169 to 79. Again, time was the only significant effect (b = 102.8, t = 5.14, p < 0.001).
Regarding the analysis of drinking risk level, a total of 44 patients (40%) downshifted their risk level. A total of 22 patients had a one-category downshift, 15 patients a two-category downshift, and seven patients a three-category downshift. Only four patients presented an increase in their risk category. The rest (62 patients) stayed on the same level of risk. Non-significant changes were observed for liver enzymes.
Differential characteristics between responders and non-responders are shown in Table 2. None of the variables investigated yielded significant results in the logistic regression analysis.
3.3 Satisfaction
Figure 2 displays professionals’ and patients’ satisfaction with nalmefene, as recorded by the MSQ. A great majority of professionals stated that a drinking reduction goal highly or simply facilitates the therapeutic alliance with patients (91%). When compared to previous pharmacological treatments, three out of 31 patients (9.7%) reported low satisfaction with nalmefene, 11 out of 31 (35.5%) reported no changes in satisfaction, and 17 patients (54.8%) reported a higher satisfaction.
In the logistic regression analysis, sex (being man), number of days taking study medication, and a lesser mean alcohol consumption during the first month of the study were associated with increased satisfaction.
3.4 Safety
During the first month, 29 patients had medication-related adverse events, which are described in Table 3. Most were mild, and no serious adverse events were recorded. Also, no overdose was observed or notified.
4 Discussion
The early results of this phase IV trial confirm the effectiveness of nalmefene in alcohol-use disorder patients in routine clinical settings. Both the number of heavy drinking days and the total alcohol consumption were significantly reduced during the first month of treatment. Overall, nalmefene was well tolerated and no significant severe or life-threatening reactions were observed.
Of note, the rates of both addictive and psychiatric comorbidities were high, a fact that is in sharp contrast with the samples of randomized, controlled studies, which are usually more restrictive in their inclusion criteria. In fact, the high rate of psychiatric comorbidities in alcohol patients is a well-documented phenomenon [42, 43]. This finding supports the criticisms targeted at the external validity of experimental studies [30] and at the same time suggests that studies like the SENSE trial [24], where patients with psychiatric comorbidities were included, should be the norm rather than the exception.
In trying to find differential characteristics between responders and non-responders to treatment, as measured by reductions in alcohol consumption parameters and changes in drinking risk categories, we were unable to find statistically significant variables. This could be, in part, due to lack of statistical power. Further studies with greater statistical power should try to find predictors of response. Given the lack of significance, it remains to be elucidated whether, just as it is the case with naltrexone [44, 45], a positive family history of alcohol problems predicts a greater response to nalmefene.
Also in line with the lack of significant differences between responders and non-responders, it should be noted that a great number of patients were already labeled as low-risk drinkers at baseline, thus reducing the statistical power needed to detect differences. In fact, almost half of the patients were considered low-risk drinkers at study entry, a fact that at first sight could seem contradictory to nalmefene therapeutic indications. It should be noted, however, that risk assessment for study purposes was based on the previous 28 days. It is probable that clinicians, when deciding the risk category of patients, take into account a longer timeframe. Also, similar to what has been observed in phase III trials, it is possible that the mere fact of patients deciding to enter into treatment leads to significant reductions in drinking. It would also seem reasonable to believe that, in specialized treatment settings, reduction aims are offered to those with the lowest drinking risk. Interestingly, the percentage of low-risk drinkers in this trial is very similar to that of phase III trials if we add up the baseline low-risk drinkers and the ones who became low-risk drinkers prior to nalmefene initiation. Importantly, even taking into account this situation, reductions in drinking parameters were significant, even with the conservative approach of BOCF.
Satisfaction data show a high degree of satisfaction regarding nalmefene for a majority of patients and clinicians. Moreover, a majority of clinicians were highly concordant with the fact that being able to set up a drinking reduction goal with patients is of help when establishing a therapeutic alliance with them. Despite not being a frequent treatment goal in alcohol studies, the importance of the therapeutic alliance should never be underestimated, since many studies highlight its importance in the therapeutic process of patients [46, 47]. In trying to find reasons supporting the high satisfaction rate found in this study, one could hypothesize that nalmefene, being the first drug approved for alcohol reduction, could somehow empower both patients and professionals in the sense that it somehow makes official, from the pharmacological point of view, a paradigm that has been increasingly recognized as valid, necessary and adequate in some instances, namely, alcohol reduction as opposed to total abstinence. As expected, satisfaction was to some extent influenced by outcomes, as shown by the regression analysis.
Finally, it is important to consider the differences that exist between this study and the phase III trials. Age at onset of drinking problems is clearly different. While real differences could be expected between real practice and experimental studies, it could also be due to different methods of data recollection. As already mentioned, low-risk drinkers were also overrepresented in this study, and worth mentioning, too, this trial had a higher rate of previously treated alcohol-dependent patients, including a higher percentage of patients having been treated for alcohol withdrawal, when compared to phase III trials. While that could suggest a greater severity, baseline alcohol parameters were, conversely, milder in our study sample, with fewer heavy drinking days and lower mean alcohol consumption. It also looks like patients had a superior rate of medication intake. Interestingly, it should also be mentioned that a high proportion of patients in this study took nalmefene on a daily basis, suggesting that, despite being labeled as an “as-needed” medication, patients and clinicians in real-world practice will frequently use it on a scheduled, daily basis. All in all we believe this study suggests that, as previously shown in other diseases, samples from experimental studies might differ in some relevant aspects from patients in routine clinical practice. While efforts targeted at increasing phase III trials’ external validity should be encouraged, this study also confirms that phase IV studies are indeed a crucial part of the research process.
Several limitations apply to this study. First, inherent to post-marketing studies, this is an observational study with no comparison group. Also, though primary effectiveness analysis reached statistical significance, the final sample size remained smaller than expected (only being able to include 110 patients out of 160 expected); therefore, caution should be taken when interpreting effectiveness results. Also, it is important to mention that we only included patients from four different sites, all belonging to the same city. In this sense, phase III trials had a much wider representation, with patients from different countries being included. Finally, it is important to remember that these are short-term results, and that 6-month data will be necessary to confirm these early outcomes.
5 Conclusions
This study backs up previous demonstrations of nalmefene efficacy in alcohol-dependent patients. It also highlights that patients in routine settings might differ significantly from patients included in experimental studies. Importantly, this study confirms previous observations of a high psychiatric comorbidity in alcohol-dependent subjects. It also suggests that, if we want to expand and increase the validity of all the research regarding pharmacological treatments in the field of alcohol dependence, phase IV trials are essential.
References
Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(9):655–79.
Kohn R, Saxena S, Levav I, Saraceno B. The treatment gap in mental health care. Bull World Health Organ. 2004;82(11):858–66.
Merkx MJM, Schippers GM, Koeter MWJ, Vuijk PJ, Oudejans SCC, Stam RK, et al. Guidelines for allocating outpatient alcohol abusers to levels of care: predictive validity. Addict Behav. 2011;36(6):570–5.
Miller WR, Walters ST, Bennett ME. How effective is alcoholism treatment in the United States? J Stud Alcohol. 2001;62(2):211–20.
Agency EM. Guideline on the development of medicinal products for the treatment of alcohol dependence. European Medicines Agency 2010. http://www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2010/03/WC500074898.pdf. Accessed 1 Sept 2017.
Gastfriend DR, Garbutt JC, Pettinati HM, Forman RF. Reduction in heavy drinking as a treatment outcome in alcohol dependence. J Subst Abuse Treat. 2007;33(1):71–80.
Heilig M, Goldman D, Berrettini W, O’Brien CP. Pharmacogenetic approaches to the treatment of alcohol addiction. Nat Rev Neurosci. 2011;12(11):670–84.
Luquiens A, Reynaud M, Aubin HJ. Is controlled drinking an acceptable goal in the treatment of alcohol dependence? A survey of French alcohol specialists. Alcohol Alcohol. 2011;46(5):586–91.
Rehm J. The risks associated with alcohol use and alcoholism. Alcohol Res Health. 2011;34(2):135–43.
Dixon R, Gentile J, Hsu HB, Hsiao J, Howes J, Garg D, et al. Nalmefene: safety and kinetics after single and multiple oral doses of a new opioid antagonist. J Clin Pharmacol. 1987;27(3):233–9.
Gal TJ, DiFazio CA, Dixon R. Prolonged blockade of opioid effect with oral nalmefene. Clin Pharmacol Ther. 1986;40(5):537–42.
Emmerson PJ, Liu MR, Woods JH, Medzihradsky F. Binding affinity and selectivity of opioids at mu, delta and kappa receptors in monkey brain membranes. J Pharmacol Exp Ther. 1994;271(3):1630–7.
Ingman K, Hagelberg N, Aalto S, Någren K, Juhakoski A, Karhuvaara S, et al. Prolonged central mu-opioid receptor occupancy after single and repeated nalmefene dosing. Neuropsychopharmacology. 2005;30(12):2245–53.
Bruijnzeel AW. kappa-Opioid receptor signaling and brain reward function. Brain Res Rev. 2009;62(1):127–46.
Garbutt JC. Efficacy and tolerability of naltrexone in the management of alcohol dependence. Curr Pharm Des. 2010;16(19):2091–7.
Swift RM. Naltrexone and nalmefene: any meaningful difference? Biol Psychiatry. 2013;73(8):700–1.
Mason BJ, Salvato FR, Williams LD, Ritvo EC, Cutler RB. A double-blind, placebo-controlled study of oral nalmefene for alcohol dependence. Arch Gen Psychiatry. 1999;56(8):719–24.
Mason BJ, Ritvo EC, Morgan RO, Salvato FR, Goldberg G, Welch B, et al. A double-blind, placebo-controlled pilot study to evaluate the efficacy and safety of oral nalmefene HCl for alcohol dependence. Alcohol Clin Exp Res. 1994;18(5):1162–7.
Anton RF, Pettinati H, Zweben A, Kranzler HR, Johnson B, Bohn MJ, et al. A multi-site dose ranging study of nalmefene in the treatment of alcohol dependence. J Clin Psychopharmacol. 2004;24(4):421–8.
Karhuvaara S, Simojoki K, Virta A, Rosberg M, Loyttyniemi E, Nurminen T, et al. Targeted nalmefene with simple medical management in the treatment of heavy drinkers: a randomized double-blind placebo-controlled multicenter study. Alcohol Clin Exp Res. 2007;31(7):1179–87.
Gual A, He Y, Torup L, van den Brink W, Mann K. A randomised, double-blind, placebo-controlled, efficacy study of nalmefene, as-needed use, in patients with alcohol dependence. Eur Neuropsychopharmacol. 2013;23(11):1432–42.
Mann K, Bladström A, Torup L, Gual A, van den Brink W. Extending the treatment options in alcohol dependence: a randomized controlled study of as-needed nalmefene. Biol Psychiatry. 2013;73(8):706–13.
van den Brink W, Aubin HJ, Bladstrom A, Torup L, Gual A, Mann K. Efficacy of as-needed nalmefene in alcohol-dependent patients with at least a high drinking risk level: results from a subgroup analysis of two randomized controlled 6-month studies. Alcohol Alcohol. 2013;48(5):570–8.
van den Brink W, Sørensen P, Torup L, Mann K, Gual A, SENSE Study Group. Long-term efficacy, tolerability and safety of nalmefene as-needed in patients with alcohol dependence: a 1-year, randomised controlled study. J Psychopharmacol. 2014;28(8):733–44.
Pearson M, Coomber R. The challenge of external validity in policy-relevant systematic reviews: a case study from the field of substance misuse. Addiction. 2010;105(1):136–45.
Dekkers OM, von Elm E, Algra A, Romijn JA, Vandenbroucke JP. How to assess the external validity of therapeutic trials: a conceptual approach. Int J Epidemiol. 2010;39(1):89–94.
Rothwell PM. External validity of randomised controlled trials: “to whom do the results of this trial apply?”. Lancet. 2005;365(9453):82–93.
Hoertel N, de Maricourt P, Katz J, Doukhan R, Lavaud P, Peyre H, et al. Are participants in pharmacological and psychotherapy treatment trials for social anxiety disorder representative of patients in real-life settings? J Clin Psychopharmacol. 2014;34(6):697–703.
Uijen AA, Bakx JC, Mokkink HGA, van Weel C. Hypertension patients participating in trials differ in many aspects from patients treated in general practices. J Clin Epidemiol. 2007;60(4):330–5.
Persaud N, Mamdani MM. External validity: the neglected dimension in evidence ranking. J Eval Clin Pract. 2006;12(4):450–3.
Farahani P, Levine M, Gaebel K, Thabane L. Clinical data gap between phase III clinical trials [pre-marketing] and phase IV [post-marketing] studies: evaluation of etanercept in rheumatoid arthritis. Can J Clin Pharmacol. 2005;12(3):e254–63.
Linden M. Phase-IV research: specifics, objectives and methodology. Pharmacopsychiatry. 1984;17(5):140–2.
Naudet F, Granger B, Braillon A. Cost-effectiveness of nalmefene: exaggerated expectations or fallacy? Alcohol Alcohol. 2016;51(5):623–4.
Soyka M, Friede M, Schnitker J. Comparing nalmefene and naltrexone in alcohol dependence: are there any differences? Results from an indirect meta-analysis—comment to Naudet. Pharmacopsychiatry. 2016;49(6):261–2.
Naudet F, Fitzgerald N, Braillon A. Nalmefene for alcohol dependence: a NICE decision? Lancet Psychiatry. 2016;3(12):1104–5.
Fitzgerald N, Angus K, Elders A, de Andrade M, Raistrick D, Heather N, et al. Weak evidence on nalmefene creates dilemmas for clinicians and poses questions for regulators and researchers. Addiction. 2016;111(8):1477–87.
Barrio P, Ortega L, Bona X, Gual A. Development, validation, and implementation of an innovative mobile app for alcohol dependence management: protocol for the SIDEAL trial. JMIR Res Protoc. 2016;5(1):e27.
Barrio P, Ortega L, López H, Gual A. Self-management and shared decision-making in alcohol dependence via a mobile app: a pilot study. Int J Behav Med. 2017;24(5):722–727.
Sobell LC, Sobell MB. Timeline follow-back: a technique for assessing self-reported ethanol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: psychosocial and biological methods. Totowa: Humana Press; 1992. p. 41–72.
Kalali A. Patient satisfaction with, and acceptability of, atypical antipsychotics. Curr Med Res Opin. 1999;15(2):135–7.
Vernon MK, Revicki DA, Awad AG, Dirani R, Panish J, Canuso CM, et al. Psychometric evaluation of the Medication Satisfaction Questionnaire [MSQ] to assess satisfaction with antipsychotic medication among schizophrenia patients. Schizophr Res. 2010;118(1–3):271–8.
Flensborg-Madsen T, Mortensen EL, Knop J, Becker U, Sher L, Grønbæk M. Comorbidity and temporal ordering of alcohol use disorders and other psychiatric disorders: results from a Danish register-based study. Compr Psychiatry. 2009;50(4):307–14.
Fein G. Psychiatric comorbidity in alcohol dependence. Neuropsychol Rev. 2015;25(4):456–75.
Monterosso JR, Flannery BA, Pettinati HM, Oslin DW, Rukstalis M, O’Brien CP, et al. Predicting treatment response to naltrexone: the influence of craving and family history. Am J Addict. 2001;10(3):258–68.
Garbutt JC, Greenblatt AM, West SL, Morgan LC, Kampov-Polevoy A, Jordan HS, et al. Clinical and biological moderators of response to naltrexone in alcohol dependence: a systematic review of the evidence. Addiction. 2014;109(8):1274–84.
Dundon WD, Pettinati HM, Lynch KG, Xie H, Varillo KM, Makadon C, et al. The therapeutic alliance in medical-based interventions impacts outcome in treating alcohol dependence. Drug Alcohol Depend. 2008;95(3):230–6.
Öjehagen A, Berglund M, Hansson L. The relationship between helping alliance and outcome in outpatient treatment of alcoholics: a comparative study of psychiatric treatment and multimodal behavioural therapy. Alcohol Alcohol. 1997;32(3):241–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Lundbeck. The sponsor was involved in the study design, but not in data collection, analysis, manuscript writing, or the decision to submit the article for publication.
Conflict of interest
Dr. Barrio, Dr. Roncero, Dr. Guardia and Dr. Gual have received honoraria from Lundbeck. Dr. Barrio has also received honoraria from Pfizer. Dr. Roncero has also received honoraria from Janssen-Cilag, Otsuka, Server, GSK, Rovi, Astra, MSD and Sanofi. Dr. Yuguero and Dr. Ortega have no conflict of interest to declare.
Ethics approval
The study protocol, final approved informed consent document, and all supporting information were submitted to and approved by the institutional review boards of all participating centers.
Consent to participate
All participants provided written informed consent before taking part in study procedures. The study was conducted in accordance with the International Conference on Harmonisation and Good Clinical Practice and the principles of the Declaration of Helsinki.
Rights and permissions
About this article
Cite this article
Barrio, P., Ortega, L., Guardia, J. et al. Who Receives Nalmefene and How Does It Work in the Real World? A Single-Arm, Phase IV Study of Nalmefene in Alcohol Dependent Outpatients: Baseline and 1-Month Results. Clin Drug Investig 38, 147–155 (2018). https://doi.org/10.1007/s40261-017-0590-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-017-0590-4