Abstract
Sleep disorders are common in adults with attention deficit/hyperactivity disorder (ADHD). Two sleep questionnaires; the Brown ADD Scale, the Symptom-Checklist-90-R, and a self-developed symptom questionnaire were administered in this study. In a sample of 61 patients without comorbidity, current substance abuse and medication intake, sleep problems were reported more often than in healthy controls. A lack of being refreshed in the morning was very closely associated with ADHD symptomatology whereas insomnia was related to the presence of comorbidity and depressive symptoms. In the total sample (N = 120), medication intake (mainly stimulants) was not related to any of the sleep parameters. It seems important to screen adult patients with ADHD for the presence of sleep disorders, especially insomnia, restless legs syndrome, and sleep-related breathing disorders (the last in conjunction with the body mass index). Since primary sleep disorders are associated with cognitive impairment, one might expect that ADHD symptomatology may improve if comorbid sleep disorders are adequately treated in addition to the specific ADHD treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep disorders are common in children with attention deficit/hyperactivity disorder (ADHD) (overviews: [1, 2]). In addition to complaints of insomnia, increased prevalence rates for restless legs syndrome, periodic limb movements during sleep and sleep apnea have been reported, although the findings are not yet conclusive [3]. Since ADHD persists in up to 50% of the children into adulthood [4, 5] and the prevalence rate of ADHD in adults is estimated to be about 4% [6–8], it is interesting to learn if sleep complaints are also a common feature in adult ADHD.
In two clinical samples of adult ADHD patients (N = 219, Dodson and Zhang 1999, cited in [9]; N = 141, [9]) sleep problems were reported by more than 70% of the patients. Even in a non-clinical sample of 148 high-school students [10] symptoms of inattention and hyperactivity measured by the Adult Behavior Checklist correlated significantly with insomnia complaints (r = 0.47) and daytime sleepiness (r = 0.61). In a small sample (N = 8), Kooij et al. [9] found increased motor activity during sleep measured by actigraphy and reduced sleep quality (both measures improved after 3 weeks of stimulant therapy). The first polysomnographic study [11] showed no differences in sleep parameters such as sleep efficiency, arousal index, slow wave sleep, and REM sleep among 20 adult ADHD patients without current comorbidity, or drug intake and age- and sex-matched controls. Three patients, however, suffered from restless legs symptoms and the index of periodic limb movements during sleep was elevated in the total patient sample [11]. Despite the lack of differences in the objective sleep parameters, subjective sleep quality rated after the laboratory nights was considerable lower in the patients in comparison to the controls [11] indicating a sleep misperception.
A heightened rate of ADHD symptoms in restless legs patients in comparison to insomnia patients and controls might indicate a genetic link (dopaminergic system) between the two disorders [12]. Naseem et al. [13] and Surman et al. [14] reported several cases of adult ADHD patients with sleep complaints who were diagnosed with sleep apnea after polysomnographic evaluation. Since CPAP treatment reduced daytime symptoms in these patients [13], Surman et al. [14] recommend that taking a sleep history should be part of ADHD diagnostic procedures. Overall, these studies have shown that sleep disorders—as other psychiatric comorbidities (cf. [15])—are common in adult ADHD patients.
The present study was designed to investigate two topics. First, the subjective sleep quality and other symptoms, e.g., movement disorders, were measured psychometrically in order to compare these data with those of healthy controls and to correlate sleep quality with disorder-related variables such as severity of daytime symptomatology, comorbidity, and medication intake. Second, the effect of depressive mood on the group differences and correlation was studied, hypothesizing that the link between sleep disorders and ADHD is not solely explained by depressive mood.
Method
Patients and healthy controls
Overall, 120 patients (64 women, 56 men) whose mean age was 34.8 ± 10.0 years (range: 18–62 years) were included in this investigation. All patients met DSM IV criteria for ADHD. The subtypes distributed as follows: 31 inattentive, 87 combined, 2 hyperactive-impulsive. Mean Brown Attention Deficit Disorder Scales (BADDS) score was 74.9 ± 25.6 (N = 114). In 22 patients other disorders were diagnosed: 16 depression/dysthymia, 4 anxiety disorder, 1 tic disorder, and 1 obsessive-compulsive disorder. In 8 patients current substance abuse (4 THC abuse, 2 alcohol abuse, 1 multiple substance abuse, 1 stimulant abuse) was present. Forty-two patients took medication: methylphenidate (20), reboxitine (8), serotonin reuptake inhibitors (6), venlafaxine (4), tricyclic antidepressants (3), and fenetyllin (1). Forty patients reported that they smoke. Another first-grade family member with ADHD was present in 78 cases.
Sixty-one patients (34 women, 27 men) were free of medication and without comorbidity. Their mean age was 35.3 ± 10.8 years. The distribution of the subtypes was as follows: (14 inattentive, 46 combined, 1 hyperactive-impulsive). Mean BADDS score was 76.5 ± 24.5 (N = 58).
The control sample comprised 444 persons (376 women, 68 men) whose mean age was 23.5 ± 5.7 years [16]. None of the controls suffered from sleep disorders or psychiatric illness at the time of the investigation.
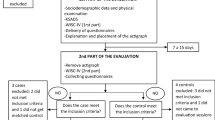
Materials and procedure
During the course of diagnostic and therapeutic procedures within the ADHD outpatient Department of the Central Institute of Mental Health, Mannheim, the patients received several questionnaires, which they completed at home.
The first questionnaire was developed by the authors and —beside socio-demographic items—consisting of questions regarding current symptomatology (medication, family history, and smoking). For the regression analysis, the two hyperactive-impulsive patients were added to the combined group (coded as 1), whereas the inattentive group was coded as 0. In a similar way, THC abuse, smoking, family history of ADHD, and medication intake were given a binary code for the regression analyses.
Attention deficit/hyperactivity disorder symptomatology was measured by the BADDS ([17], German translation: U. Ruhl). The BADDS comprises 40 four-point self-rating scales (0 = never, 1 = once a week or less, 2 = twice a week, 3 = almost daily) aiming at five clusters: organizing and activating to work (9 items), sustained attention and concentration (9 items), sustaining energy and effort (9 items), managing affective interference (7 items), and utilizing “working memory”, and accessing recall (6 Items). The sum score was included in the present analysis. A cut-off of 50 has a high sensitivity (96%) and high specifity (94%) [17]. The retest reliability (r = 0.87, two-week period, N = 75) and the internal consistency (Cronbach’s alpha > 0.86 for the total score) are high [17]. For further details on the German version see Sobanski et al. [18].
In addition, two sleep questionnaires (Schlaffragebogen B; SF-B; [19] and Landecker Inventar zur Erfassung von Schlafstörungen; LISST; Weeß et al. [20] were administered. The SF-B sleep questionnaire comprises 28 items measuring composite scores such as sleep quality (11 items) and feeling of being refreshed in the morning (7 items). The estimates refer to the previous 2 weeks. The composite scores (averages) ranged from 1 to 5, since most scales of the sleep questionnaire are constructed as five-point Likert scales. Sleep latency was measured by a six-point scale (1 = less than 5 min, 2 = 5–10 min, 3 = 10–20 min, 4 = 20–30 min, 5 = 30 min to 1 h, 6 = more than 1 h). The inter-item consistency for the composite scores range from r = 0.77 to r = 0.87 and the retest reliability (4 weeks) was about r = 0.70 [19]. Construct validity was shown in several factor analyses, and comparisons with expert ratings were satisfying, for example, r = −0.67 between sleep quality and the degree of insomnia [19].
The LISST sleep questionnaire is composed of 75 items and was constructed as a screening instrument to detect different sleep disorders. Sum scores were computed for movement disorders (5 items), sleep/wake rhythm disorder (7 items), insomnia (6 items), sleep quality (8 items), nocturnal breathing disorders (4 items), restless legs syndrome (5 items), parasomnias (6 items), and tiredness during the day (5 items). The single scales followed a six-point Likert scale format (1 = never, 2 = rarely, 3 = sometimes, 4 = often, 5 = very often, 6 = always). Sufficient internal consistencies as well as accurate discrimination of patients with sleep disorders (diagnosed in a sleep medicine center including two polysomnographic nights) have been demonstrated [20].
The Symptom Checklist (SCL-90-R; [21]) with a retrospective interval of 7 days was the third instrument of the present study. The general severity index (mean for all 90 four-point items) and the depression scale were included in the analyses. Sufficient reliability and validity for these measures have been demonstrated by the test author [21].
Statistical analyses were carried out with the SAS for Windows (Vers. 8.02) software package. Since the patient group and the healthy controls differed in respect to age means and gender distribution, analyses of covariance (ANCOVA) were computed to control for age and gender effects; gender was introduced as a second factor and age as covariate. Pearson correlations and partial correlations were computed for the relationships between questionnaire measures. Regression analyses for different sleep variables as dependent variables and age, gender, comorbidity, substance abuse, subtype, smoking, medication intake, ADHD in the family, BADDS, and depression scale as predictors have been carried out. The significance levels were given as exact values. Bonferroni corrections have not been carried out since the study is exploratory and, second, the reduction of statistical power would have been a problem.
Results
Sleep variables in ADHD patients versus controls
In Table 1, the comparisons for the SF-B sleep questionnaire are depicted. Patients (without comorbidity, current substance abuse, and medication) rated their sleep quality and the feeling of being refreshed in the morning much lower than healthy controls, whereas the effects regarding sleep latency and frequency of nocturnal awakenings were only marginally significant. Although the F-values were reduced by introducing the depression score of the SCL-90-R as a second covariate, the differences between patients and controls regarding sleep quality and feeling of being refreshed in the morning remained significant.
The results of the LISST sleep questionnaire are comparable (see Table 2); patients reported movement disorder symptoms, insomnia symptoms, problems with sleep quality, problems with sleep/wake pattern, sleep-disordered breathing symptoms, tiredness during the day and parasomnias more often. After adding the depression score to the ANCOVA as the second covariate, the differences remained significant except for sleep-disordered breathing.
The patients differed also in regard to the depression scale (patients: 1.15 ± 0.88 vs. controls: 0.80 ± 0.65, F = 14.7, P < 0.0001) and the general symptom index (patient: 0.91 ± 0.59 vs. controls: 0.59 ± 0.44, F = 23.1, P < 0.0001). Both analyses are ANCOVAS with the factors diagnosis (reported) and gender and the covariate age.
Sleep variables and BADDS scores
As expected, the BADDS score correlated significantly with low sleep quality, not feeling refreshed in the morning, movement disorder symptoms, insomnia, problems with sleep/wake pattern and tiredness during the day in the subsample of patients without comorbidity, current substance abuse, and medication intake (see Tables 1 and 2). Sleep latency, frequency of nocturnal awakenings, problems with sleep quality (LISST), sleep-disordered breathing symptoms, and parasomnias were not associated with the BADDS score. If the depression score is partialled out, significant correlation coefficients were found for sleep quality, feeling of being refreshed in the morning, sleep latency, problems with sleep/wake pattern, and tiredness during the day, i.e., the severity of daytime ADHD symptomatology is associated with the amount of sleep problems.
Sleep variables and clinical variables
In Table 3, regression analyses for the total patient sample are depicted. The BADDS index was significantly related to sleep quality, feeling of being refreshed in the morning, sleep latency, problems with sleep/wake pattern, and tiredness during the day. The depression scale, on the other hand, was related to movement disorders, insomnia, problems with sleep quality, problems with sleep/wake pattern, parasomnias and tiredness during the day. The presence of comorbidity (mainly depression) was associated with poor sleep quality, not feeling refreshed in the morning, insomnia, and problems with sleep quality. Smoking was associated with higher tiredness during the day. Men more often reported symptoms of sleep-disordered breathing like snoring or apneas but if the body mass index (BMI) was additionally introduced in this regression analysis, only this variable (t = 3.0, P = 0.0017) and smoking (t = 2.2, P = 0.0108) showed significant associations to sleep-disordered breathing symptoms. Substance abuse, medication intake, subtype, and ADHD in another family member were not related to any of the sleep variables.
Discussion
The findings of the present study confirmed that adult patients with ADHD report sleep complaints more often than healthy controls. The feeling of being refreshed in the morning was very closely associated with ADHD symptomatology whereas insomnia, on the other hand, was related to the presence of comorbidity and depressive symptoms.
As reported by Dodson and Zhang (1999; cited in [9] and Kooij et al. [9], it was also found that patients without comorbidity, current substance abuse and medication intake report sleep problems more often than healthy controls. Even after controlling for depressive mood, most differences remained significant. The basic idea behind controlling for depressive mood—even within sub-clinical ranges and not limiting it to exclusion of manifest depressive syndromes—was the possible bias because the patients are seeking help for their ADHD symptoms and might differ especially in this aspect from non-help seeking patients. However, the results indicate that ADHD is genuinely associated with sleep disorders. Taking into account the findings of Philipsen et al. [11], it seems that patients seem to suffer from a sleep misperception, i.e., reduced sleep quality and relatively normal objective physiological sleep parameters. This might be interpreted as cognitive arousal and the strong effect on the feeling of being refreshed in the morning demonstrating that this is of clinical relevance.
Movement disorders, e.g., restless legs symptoms were also reported more often in this patient sample confirming the findings of Wagner et al. [12] and the idea of a genetic link via the dopaminergic system between the two disorders, e.g., striatal dysfunction of the dopaminergic system (cf. [22, 23]). Despite the case reports of Naseem et al. [13] and Surman et al. [14], sleep-disordered breathing symptoms were not found to be elevated in this sample. The regression analysis clearly showed that these symptoms were associated with the well-known body-mass index and smoking risk factors but not ADHD symptomatology. One might assume that some cases of sleep apnea patients are misdiagnosed (as reported for a child by Schredl et al. [24]) and in the other cases the co-occurrence of the two disorders is explained by chance. In order to verify the questionnaire findings of the present study, further polysomnographic studies in adult ADHD patients are necessary.
The correlation and regression analyses revealed that the severity of ADHD symptoms was closely related to the feeling of being refreshed in the morning, problems with the sleep/wake pattern, sleep quality, and sleep latency whereas the depressive symptomatology (depression scale and depression as comorbidity) was related to insomnia, parasomnias, movement disorders, and tiredness during the day. Since Kooij et al. [9] measured an increased number of movements during the night by actigraphy and Philipsen et al. [11] reported increased indices of periodic limb movements, one might speculate if the feeling of not been refreshed after sleep is related to movements during sleep. Studies with larger samples of ADHD who undergo polysomnographic recording in addition to filling in the sleep questionnaires will be necessary to answer this question. Interestingly, medication intake in this cross-sectional study was not related to any of the sleep variables, although Kooij et al. [9] reported a positive effect of stimulant therapy on sleep (last intake of medication at 4 p.m.) in a very small sample (N = 8). Therefore, larger studies are necessary to answer the question as to whether therapy with stimulants and/or specific psychotherapy for adult ADHD patients (cf. [25]) affect the sleep of adult ADHD patients—measured by polysomnography and sleep questionnaires—in a positive way.
Conclusion
It seems important to screen adult patients with ADHD for the presence of sleep disorders, especially insomnia, restless legs syndrome, and sleep-related breathing disorders (the last in conjunction with the BMI). Since primary sleep disorders are associated with cognitive impairment [26], one might expect that ADHD symptomatology will improve if comorbid sleep disorders will be adequately treated, e.g., cognitive-behavioral therapy for insomnia and sleep misperception, dopamine agonists for restless legs syndrome, and periodic limb movements during sleep, or CPAP for sleep-related breathing disorders. This will be especially important to consider for patients whose sleep problems do not improve during stimulant therapy.
References
Cohen-Zion M, Ancoli-Israel S (2004) Sleep in children with attention-deficit hyperactivity disorder (ADHD): a review of naturalistic and stimulant intervention studies. Sleep Med Rev 8:379–402
Owens J (2005) The ADHD and sleep conundrum: a review. J Dev Behav Pediatr 26:312–322
Frölich J, Lehmkuhl G, Wiater A (2003) Schlafstörungen bei hyperkinetischen Kindern—Zusammenhänge zu Arousalstörungen, differentialdiagnostische Abgrenzungen und Komorbiditäten. Z Kinder Jugendpsychiatrie 31:113–143
Rasmussen P, Gillberg C (2000) Natural outcome of ADHD with developmental coordination disorder at age 22 years: a controlled, longitudinal, community-based study. J Am Acad Child Adolesc Psychiatry 39:1424–1431
Barkley RA, Fischer M, Smallish L, Fletcher K (2002) The persistence of attention-deficit/hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. J Abnorm Psychol 111:279–289
Murphy K, Barkley RA (1996) Prevalence of DSM-IV symptoms of ADHD in adult licensed drivers: implication of clinical diagnosis. J Atten Disord 1:147–161
Heiligenstein E, Conyers LM, Berns AR, Smith MA (1998) Preliminary normative data on DSM-IV attention deficit hyperactivity disorder in college students. J Am Coll Health 46:185–188
Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, Faraone SV, Greenhill LL, Howes MJ, Secnik K, Spencer T, Ustun TB, Walters EE, Zaslavsky AM (2006) The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. Am J Psychiatr 163:716–723
Kooij JJS, Middelkoop HAM, van Gils K, Buitelaar JK (2001) The effect of stimulants on nocturnal motor activity and sleep quality in adults with ADHD: an open-label case–control study. J Clin Psychiatry 62:952–956
Kass SJ, Wallace JC, Vodanovich SJ (2003) Boredom proneness and sleep disorders as predictors of adult attention deficit scores. J Atten Disord 7:83–91
Philipsen A, Feige B, Hesslinger B, Ebert D, Carl C, Hornyak M, Lieb K, Voderholzer U, Riemann D (2005) Sleep in adults with attention-deficit/hyperactivity disorder: a controlled polysomnographic study including spectral analysis of the sleep EEG. Sleep 28:738–745
Wagner ML, Walters AS, Fisher BC (2004) Symptoms of attention-deficit/hyperactivity disorder in adults with restless legs syndrome. Sleep 27:1499–1504
Naseem S, Chaudhary B, Collop N (2001) Attention deficit hyperactivity disorder in adults and obstructive sleep apnea. Chest 119:294–296
Surman BH, Thomas RJ, Aleardi M, Pagano C, Biederman J (2006) Adults with ADHD and sleep complaints: a pilot study identifying sleep-disordered breathing using polysomnography and sleep quality assessment. J Atten Disord 9:550–555
Sobanski E (2006) Psychiatric comorbidity in adults with attention-deficit/hyperactivity disorder (ADHD). Eur Arch Psychiatry Clin Neurosci 254(Suppl 1):I/26–I/31
Schredl M (2003) Effects of state and trait factors on nightmare frequency. Eur Arch Psychiatry Clin Neurosci 253:241–247
Brown TE (1996) Brown Attention-Deficit Disorder Scales. San Antonio: Psychological Corporation
Sobanski E, Alm B, Krumm B (2006) Methylphenidatbehandlung bei Erwachsenen mit Aufmerksamkeitsdefizit-/Hyperaktivitätsstörung: Bedeutung von Störungssubtyp und aktueller psychiatrischer Komorbidität. Nervenarzt (online March 17, 2006)
Görtelmeyer R (1986) Schlaf-Fragebogen A und B (Sf-A, Sf-B). In: Collegium Internationale Psychiatriae Scalarum (ed) International Skalen für Psychiatrie. Weinheim, Beltz
Weeß HC, Schürmann T, Steinberg R (1998) Das Landecker Inventar zur Erfassung von Schlafstörungen. Klingenmünster, Unpublished Questionnaire
Derogatis LR (1986) Symptom-Check-Liste (SCL 90-R). In: Collegium Internationale Psychiatriae Scalarum (ed) International Skalen für Psychiatrie. Weinheim, Beltz
Michaud M, Soucy JP, Chabli A, Lavigne G, Montplaisir J (2002) SPECT imaging of striatal pre- and postsy-naptic dopaminenergic status in restless legs syndrome with periodic leg movements in sleep. J Neurol 249:164–170
Krause J, la Fougere C, Krause KH, Ackenheil M, Dresel SH (2005) Influence of the striatal dopamine transporter availability on the response to methylphenidate in adult patients with ADHD. Eur Arch Psychiatry Clin Neurosci 255:428–431
Schredl M, Weiland G, Hentschel F (2003) Hyperaktiv durch Schlafstörungen? Obstruktives Schlafapnoe-Syndrom und Aufmerksamkeitsdefizit bzw. Hyperaktivität bei Kindern im Vorschulalter. Kinderärztliche Praxis 74:192–197
Hesslinger B, Tebartz van Elst L, Nyberg E, Dykierek P, Richter H, Berner M, Ebert D (2002) Psychotherapy of attention deficit hyperactivity disorder in adults: a pilot study using a structured skills training program. Eur Arch Psychiatr Clin Neurosci 252:177–184
Fulda S, Schulz H (2001) Cognitive dysfunction in sleep disorders. Sleep Med Rev 5:423–445
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schredl, M., Alm, B. & Sobanski, E. Sleep quality in adult patients with attention deficit hyperactivity disorder (ADHD). Eur Arch Psychiatry Clin Neurosci 257, 164–168 (2007). https://doi.org/10.1007/s00406-006-0703-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-006-0703-1