Abstract
Introduction
Oral squamous cell carcinoma (SCC) is characterized by a high risk of cervical lymph node metastasis with a high incidence of occult metastasis. A strong debate is still present regarding the best treatment for early oral cavity cancer with N0 neck.
Objective
The aim of the present study was to compare between the results of elective neck dissection (END) and watchful waiting (observation or therapeutic neck dissection) in patients with early-stage (T1/T2) oral squamous cell carcinoma with N0 neck.
Data sources
Medline database (https://www.pubmed.com), Google Scholar and Scopus.
Patients and methods
A systematic review and meta-analysis for the evaluation of regional recurrence rate and 5-year survival rate after elective neck dissection (END) or watchful waiting in early oral cancers were conducted. This study included published English medical articles (which met our predetermined inclusion criteria) in the last 30 years, concerning early oral SCC with N0 neck. 24 articles were included (4 randomized studies and 20 observational “retrospective” studies) with a total number of 2190 of patients who underwent END and 1619 who underwent watchful waiting. Regarding the 5-year survival rate, (10) studies were included with a total number of 1211 patients who underwent END and 948 who underwent watchful waiting.
Results
Regarding the regional recurrence rate, (END) was associated with significantly lower risk of recurrence when compared with observation. Regarding the 5-year survival rate, END was associated with a better survival rate than the observational group.
Conclusions
Elective neck dissection is better than watchful waiting in early (T1/T2) stage oral cavity squamous cell carcinoma with N0 neck, regarding regional recurrence and 5-year survival rate.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The oral cavity includes the buccal mucosa, anterior two-thirds of the oral tongue, retromolar trigone, lips, floor of the mouth, hard palate and alveolar ridge. Squamous cell carcinoma (SCC) is responsible for more than 90% of the head and neck tumors arising from the oral cavity and oropharynx [1]. Lymph node metastases is the most significant prognostic factor for recurrence and survival rate, reducing the survival rate by 50% [2].
Elective (prophylactic) neck treatment of the cervical nodes is performed to avoid the spread of an occult metastasis when the risk of occult metastases exceeds 15–20% [3]. Apart from carcinoma of the lips and hard palate, which have a lower incidence of cervical nodal metastasis at diagnosis, oral squamous cell carcinoma (OSCC) is characterized by a high incidence of early metastases to cervical lymph nodes (with levels 1–3 being the first-echelon lymph nodes), particularly tumors arising from oral tongue and floor of mouth [4, 5].
More than 30% of the patients with oral cavity cancer and clinically N0 neck have occult cervical nodal metastases at diagnosis. The incidence depends on the primary tumor site, depth of the tumor and its histopathologic type [6].
A strong debate about neck treatment for early-stage squamous cell carcinoma of the oral cavity (stages I and II) with clinically negative necks exist. Both elective neck dissection and “watchful-waiting” policy have their proponents. The debate arises from the fact that routine prophylactic neck treatment will add unnecessary cost and morbidity, while there is no preoperative investigation (up till now) to be 100% sure that nodal micro-metastasis does not exist, which if neglected will lead to poor regional control and decrease survival rate [7].
Aim of the study
The aim of this systematic review and meta-analysis study was to assess the need for elective neck dissection (END) in early-stage (T1/T2) OSCC with N0 neck by comparing the results of regional recurrence and 5-year survival rate in patients who underwent END versus watchful-waiting policy (therapeutic neck dissection) through analysis of prospective “randomized controlled trials” and retrospective “observational” studies.
Materials and methods
This study was done in the following steps.
-
Determination of the target subject.
Patients diagnosed with early (T1/T2) oral SCC with N0 neck.
-
Identification and location of articles.
This study was limited to published medical articles in English language in the last 30 years (1989–2018) with stage I (T1N0M0) or stage II (T2N0M0) oral squamous cell carcinoma (OSCC) in six areas (oral tongue, buccal mucosa, hard palate, alveolar margins, floor of the mouth and retromolar trigone), excluding cancer of the lips. This study was conducted through searching the Medline database (https://www.pubmed.com), Google Scholar and Scopus, using a combination of the following keywords: early oral SCC; squamous cell carcinoma; cervical neck dissection; T1/T2 oral cancers; N0 neck and oral tongue.
Included articles
-
Published in English language.
-
Published in the last 30 years.
-
Patients with oral SCC in six areas of the oral cavity (oral tongue, buccal mucosa, hard palate, alveolar margins, floor of mouth and retromolar trigone), excluding cancer of the lips.
-
Patients with pathologically proven SCC of the oral cavity.
-
Patients with N0 neck clinically and radiologically.
-
Patients with oral squamous cell carcinoma who received surgical treatment only.
-
Patients did not receive previous neck radiotherapy
Study design Randomized control trials (prospective) and observational “retrospective” studies.
Type of intervention Elective neck dissection (END) versus watchful waiting (observation or therapeutic neck dissection).
Articles which miss one or more of the above-mentioned inclusion criteria, such as articles not in English, non-SCC oral cavity tumours, clinically positive neck nodes at diagnosis, neck treatment with radiotherapy and late stage oral cavity cancer were excluded.
Medline search was done with blinding of the author’s name and journal’s name. Over 1200 articles were identified. After removal of duplicates (460), the identified articles decreased to 740 articles. After exclusion of non-relevant articles (695), 45 articles were found to be relevant. Applying the inclusion criteria, 24 articles were found to match them and selected for further steps of data analysis.
-
Data extraction.
Information was gathered from each individual study (Table 1), extracting data about:
-
The site of the tumor.
-
Total number of patients in each study and number of cases who underwent elective neck dissection (END group) or watchful waiting.
-
Type of END.
-
The results of regional control and 5-year survival rate in both groups (END group versus observational group).
Table 1 Included articles -
Data were independently extracted by two reviewers and cross-checked.
Statistical methods
Statistical analysis was done using an Openmeta software (https://openmeta.metamorphsoftware.com/).
Testing for heterogeneity
Studies included in the meta-analysis were tested for heterogeneity of the estimates using the following tests:
-
Cochran Q Chi square test: a statistically significant test (p value < 0.1) denoted heterogeneity among the studies.
-
I square (I2) index which reflects the inconsistency in the effect size measured in the meta-analysis. It may be interpreted—although not universally accepted—as follows.
I2 = 0–25%: unimportant heterogeneity.
I2 = 25–50%: moderate heterogeneity.
I2 = 50–75%: substantial heterogeneity.
I2 = 75–100%: considerable heterogeneity.
Examination of publication bias
Publication bias was assessed by examination of the funnel plots of the effect size measures and the Begg–Mazumdar rank correlation and Egger regression tests. The funnel plot is a plot of the estimated effect size on the horizontal axis versus a measure of study size (standard error for the effect size) on the vertical axis. Publication bias results in asymmetry of the funnel plot. If publication bias is present, smaller studies will show larger effects. The funnel plot may not always be a reliable tool, especially when the number of studies included in the analysis is small.
Pooling of estimates
Comparison of binary outcomes was done by estimation of the risk ratios (RR) with their 95% confidence interval (CI) and risk difference or risk reduction with their 95% CI. The incidence of the bad outcome was measured in both intervention and control groups, where incidence = number of events (regional recurrence) in a group divided by the total number of patients in this study.
Estimates from included studies were pooled using the DerSimonian and Laird random effects method (REM) and the Mantel–Haenszel fixed effects method (FEM). In the presence of significant heterogeneity, the REM was considered. Otherwise, the FEM was considered. p values < 0.05 are considered statistically significant.
Results
Regional recurrence rate
Randomized “prospective” clinical studies (N = 4)
Four studies were included, with a total number of 343 in the END group and 361 in the control group.
-
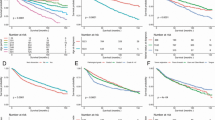
Risk ratio (Table 2, Fig. 1) There was a significant heterogeneity among the included studies (Cochran Q = 9.7521, df = 3, p = 0.0208, I2 = 69.24%). Under the random effects model (REM), END was associated with a risk of regional recurrence = 36.1% of that in the control group (RR = 0.361, 95% CI 0.197–0.660, p = 0.001). There was no evidence of publication bias by examining the Funnel plot, Egger: bias = 0.591587, p = 0.8522.
Table 2 Meta-analysis for the randomized control articles (risk ratio and risk difference of regional recurrence) -
Risk difference (Table 2) There was no significant heterogeneity among the included studies (Cochran Q = 1.6567, df = 3, p = 0.6466, I2 = 0.0%). Under the fixed-effect model (FEM), END was associated with a risk of regional recurrence that was 30.2% less than the same risk in the control group (RD = 0.302, 95% CI 0.240–0.364, p < 0.001). There was no evidence of publication bias on examining the funnel plot, Egger: bias = 1.100238, p = 0.1773.
Observational “retrospective” studies (N = 20)
Twenty studies were included in the analysis with a total number of 1847 of cases in the END group and 1258 cases in the watchful-waiting group.
-
Risk ratio (Table 3, Fig. 2) There was a significant heterogeneity among the included studies (Cochran Q = 61.1626, df = 19, p < 0.001, I2 = 68.94%). Under the random effects model (REM), END was associated with a risk of recurrence = 63.1% of the watchful-waiting group (RR = 0.631, 95% CI 0.472–0.842, p = 0.002). There was no evidence of publication bias by examining the funnel plot, Egger: bias = − 0.544464, p = 0.5968.
Table 3 Meta-analysis for the retrospective articles (risk ratio and risk difference of regional recurrence) -
Risk difference (Table 3) There was a significant heterogeneity among the included studies (Cochran Q = 51.385, df = 19, p = 0.001, I2 = 63.02%). Under the random-effect model (REM), END was associated with a risk of recurrence that was 9.87% less than the same risk in the watchful-waiting group (RD = 0.0987, 95% CI 0.0439–0.154, p < 0.001). There was no evidence of publication bias on examining the funnel plot, Egger: bias = 0.731823, p = 0.5301.
The pooled estimates of the risk reduction as well as the risk difference showed variations between the clinical trials and observational studies, hence we have not gathered them together. The 95% confidence intervals of the risk reduction of the two study types overlapped, while those of the risk difference did not.
Five-year survival rate
Ten studies were included in the analysis with a total number of 1211 in the END group and 948 in the watchful-waiting group.
-
Risk ratio (Table 4, Fig. 3) There was a significant heterogeneity among the included studies (Cochran Q = 18.50, df = 9, p = 0.0298, I2 = 51.4%). Under the random-effects model (REM), END was associated with a 67.3% improvement in the 5-year survival rate than those observed in the watchful-waiting group (RR = 0.673, 95% CI 0.508–0.893, p = 0.006). There was no evidence of publication bias on examining the funnel plot, Egger: bias = − 1.063209, p = 0.3159.
Table 4 Meta-analysis for the “Five-years survival rate” -
Risk difference (Table 4) There was a significant heterogeneity among the included studies (Cochran Q = 17.31, df = 9, p = 0.044, I2 = 48.01%). Under the random-effects model (REM), watchful-waiting group was associated with a 5-year survival rate that was 8.6% less than that of the END group (RD = 0.0861, 95% CI 0.0314–0.141, p = 0.002). There was no evidence of publication bias on examining the funnel plot, Egger: bias = 0.13042, p = 0.9303.
Discussion
The oral cavity is the most common site in the head and neck for primary malignant tumors and more than 90% of these cases are oral squamous cell carcinomas (OSCC) [1, 8]. Cervical nodal metastases is the most important prognostic factor for recurrence and survival rate, reducing the survival rate by 50%, especially with cancer of the oral tongue and floor of mouth as they have a high propensity of metastases [2, 9]. Neck staging is done clinically (bimanual palpation), radiologically and pathologically, with the latter being the most accurate way. Computed tomography (CT) and magnetic resonance imaging (MRI) are used to assess cervical lymph node metastasis; in addition, a preoperative positron emission tomography (PET) CT scan is useful as a baseline, if adjuvant treatment is anticipated. However, these imaging modalities cannot detect accurately cervical nodal micro-metastasis and hence the further need for elective neck treatment [10,11,12,13]. Recently, intraoperative sentinel lymph node biopsy (SLNB) with detection of micro-RNA molecules (marker for nodal metastasis) superseded ultrasound-guided fine needle aspiration cytology (FNAC) in detecting occult nodal micro-metastasis with more accurate results [14,15,16].
Weiss et al. showed that observation is the ideal option when the chance of occult metastasis is less than 20% in clinically N0 (cN0) and END is preferred if the probability of occult metastasis is greater than 20% [17]. The oral tongue and floor of mouth are the two most common subsites in oral cavity to be involved with SCC; moreover, they can metastasize to the contralateral side of the neck through their midline communications [18, 19]. Therefore, those patients should be offered END even in early stage (if they are thicker than 4 mm) because they carry the highest incidence of nodal metastases and contralateral spread. Moreover, surgical resection provides pathological staging, facilitating accurate assessment [20]. Yuen et al.’s retrospective study concluded that END decreased mortality due to regional recurrence and increased the survival rate in early-stage oral tongue carcinoma [21]. However, the optimal treatment of clinically N0 neck in patients with early-stage (I and II) oral cavity SCC is still debated. Both elective neck dissection and “watchful-waiting” policy have their proponents.
Some surgeons prefer END due to a high incidence of occult nodal metastases, which if neglected will lead to poor regional control and decreased survival rate with no preoperative investigation (up till now) to be 100% sure that nodal micro-metastasis does not exist. Other surgeons mentioned that routine prophylactic neck treatment will add unnecessary cost and morbidity [7, 9]. Kligerman et al. showed that patients with early-stage carcinoma of the oral cavity (stages I and II), who have been treated with primary resection plus supraomohyoid neck dissection, developed fewer neck recurrences than those who had had resection of the primary only [22].
Shah and Andersen showed that 77% of patients with oral squamous carcinoma and clinically N0 necks at initial surveillance had pathologically adverse outcomes at the time of neck dissection. Hence, they argued for END in patients with N0 necks [23]. A meta-analysis study by Fasunla et al. [7] (including four randomized controlled articles) concluded that END reduced the risk of disease-specific death in oral cavity cancers with clinically node-negative neck. But in their study, T3 patients were included, two subsites only were assessed and follow-up duration for disease-specific death was up to 3 years only (Table 5) [7]. A recent Cochrane database update of surgical interventions for the treatment of oral and oropharyngeal cancers showed insufficient evidence to draw conclusions about END for clinically negative neck nodes at the time of removal of the primary tumor compared to therapeutic (delayed) ND [24].
Our study was conducted to evaluate the need for END versus watchful waiting in early-stage OSCC (T1N0M0/T2N0M0) with proven N0 neck. It included 24 articles (4 prospective clinical trials and 20 retrospective studies) that have been published in the last three decades. In ten articles only, we were able to extract data about the 5-year survival rate. Many studies were excluded because they did not meet the inclusion criteria. For example, Okura et al.’s study was excluded because we could not extract the number of cases that suffered from regional recurrence in each group [25]. Also, Dillon et al.’s study in 2017 was excluded because we could not extract the number of cases of early-stage oral SCC, since the authors pooled the data of early- and late-stage OSCC together [26].
Regional control
Regarding the evaluation of regional recurrence in early-stage OSCC, our meta-analysis included 24 articles (f4 randomized clinical trials and 20 retrospective studies) with a total of 219) patients who underwent END and 1619 cases who underwent watchful waiting (therapeutic neck dissection). Meta-analysis for the four randomized “prospective” clinical trials (with a total of 343 cases in the END group and 361 cases in the watchful-waiting group) showed that END was associated with a risk of regional recurrence = 36.1% of that in the watchful-waiting group. Meta-analysis for the 20 “retrospective” studies (with a total of 1847 cases in the END group and 1258 cases in the watchful-waiting group) showed that END was associated with a risk of regional recurrence = 63.1% of the watchful-waiting group. These results confirmed the importance of END in reducing regional recurrence in early-stage OSCC with N0 neck.
5-year survival rate
Although many studies found improved survival rates in patients with early-stage OSCC and N0 neck who underwent END at the time of primary tumour resection [5, 22, 27, 28], Vandenbroucke et al. failed to show a statistically significant difference in survival rate between the group who received radical neck dissection and the group who was observed and received therapeutic neck dissection [29].
Kligerman et al. mentioned improved 3-year survival rate in early-stage OSCC who underwent END versus watchful waiting [22]. Dias et al. showed improved 3- and 5-year survival rates in patients with T1N0M0 SCC of the oral tongue and floor of the mouth who received END versus observation [30]. Goto et al. showed improved 5-year survival rate when END was done versus observation in early-stage oral tongue SCC [31]. Huang et al. mentioned similar results regarding disease-free survival (absence of loco-regional recurrence or second primary cancer) and overall survival [32]. Also, Peng et al. concluded that END led to improved disease-free survival in T1 oral tongue SCC [4].
Although Keski-Säntti et al. showed that early-stage oral tongue SCC patients who received END suffered from significantly fewer regional recurrences than the watchful-waiting group, there were no statistical differences in the overall survival and disease-specific survival between the two groups [33]. Also, Liu et al. and Zhang et al. concluded that END had not increased the disease-free survival or overall survival in clinical stage I oral tongue SCC [34, 35].
From the above, we can see that the 24 included articles in our study depended on different rates to assess survival after END and watchful waiting (3- and 5-year survival rate, overall survival, disease-specific survival and disease-free survival). Therefore, we chose the 5-year survival rate to pool its results in this meta-analysis. We gathered the results of 5-year survival rate from (10) articles with a total of 1211 of patients who underwent END versus 948 cases who underwent watchful waiting. There was a significant heterogeneity among the included articles. END was associated with a 67.3% improvement in the 5-year survival rate than those observed in the watchful-waiting group. These findings confirmed that elective neck dissection in early-stage OSCC with N0 neck can significantly improve the 5-year survival rate, hence the importance of END in early OSCC with N0 neck in reducing regional recurrence and improving the 5-year survival rate.
Limitations of the current study
-
Radiologic neck staging as N0 for cervical nodal metastasis differed between the various included studies. For example, some studies depended on high-definition neck ultrasound, while others depended on CT or MRI.
-
In our study, patients with stage I (T1N0M0) and stage II (T2N0M0) OSCC were pooled together, while in the meta-analysis study published by Massey et al. (2018), they were segregated. Massey et al. concluded that the incidence of occult cervical nodal metastasis in stage I and stage II OSCC were 11.5% and 24.5%, respectively. For that, they recommended END in T2N0M0 and watchful waiting in T1N0M0 OSCC [36]. However, we should be cautious while interpreting these results, since most of these studies did not use the recent TNM staging for OSCC, which incorporated the depth of invasion (DOI), being a very important prognostic factor. The 8th edition of the American Joint Committee on Cancer (AJCC) staging manual defined T1 OSCC as a tumor size ≤ 2 cm and DOI ≤ 5 mm [37].
Conclusions
Elective neck dissection is better than watchful waiting in early (T1/T2)-stage oral cavity squamous cell carcinoma with N0 neck, regarding regional recurrence and 5-year survival rate.
References
Landis SH, Murray T, Bolden S, Wingo PA (1999) Cancer statistics, 1999. CA Cancer J Clin 49(1):8–31. https://doi.org/10.3322/canjclin.49.1.8 (PMID: 10200775)
Fakih AR, Rao RS, Borges AM, Patel AR (1989) Elective versus therapeutic neck dissection in early carcinoma of the oral tongue. Am J Surg 158(4):309–313. https://doi.org/10.1016/0002-9610(89)90122-0 (PMID: 2802032)
Paleri V, Urbano TG, Mehanna H, Repanos C, Lancaster J, Roques T et al (2016) Management of neck metastases in head and neck cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 130(S2):S161–S169. https://doi.org/10.1017/S002221511600058X (PMID: 27841133)
Peng KA, Chu AC, Lai C, Grogan T, Elashoff D, Abemayor E et al (2014) Is there a role for neck dissection in T1 oral tongue squamous cell carcinoma? The UCLA experience. Am J Otolaryngol 35(6):741–746. https://doi.org/10.1016/j.amjoto.2014.06.019 (PMID: 25091179)
Haddadin KJ, Soutar DS, Webster MH, Robertson AG, Oliver RJ, MacDonald DG (2000) Natural history and patterns of recurrence of tongue tumours. Br J Plast Surg 53(4):279–285. https://doi.org/10.1054/bjps.1999.1111 (PMID: 10876250)
Yuen APW, Lam KY, Lam LK, Ho CM, Wong A, Chow TL et al (2002) Prognostic factors of clinically stage I and II oral tongue carcinoma—a comparative study of stage, thickness, shape, growth pattern, invasive front malignancy grading, Martinez–Gimeno score, and pathologic features. Head Neck 24(6):513–520. https://doi.org/10.1002/hed.10094 (PMID: 12112547)
Fasunla AJ, Greene BH, Timmesfeld N, Wiegand S, Werner JA, Sesterhenn AM (2011) A meta-analysis of the randomized controlled trials on elective neck dissection versus therapeutic neck dissection in oral cavity cancers with clinically node-negative neck. Oral Oncol 47(5):320–324. https://doi.org/10.1016/j.oraloncology.2011.03.009 (PMID: 21459661)
Davidson J, Biem J, Detsky A (1995) The clinically negative neck in patients with early oral cavity carcinoma: a decision-analysis approach to management. J Otolaryngol 24(6):323–329 (PMID: 8699596)
Byers RM, Weber RS, Andrews T, McGill D, Kare R, Wolf P (1997) Frequency and therapeutic implications of “skip metastases” in the neck from squamous carcinoma of the oral tongue. Head Neck 19(1):14–19. https://doi.org/10.1002/(SICI)1097-0347(199701)19:1%3c14:AID-HED3%3e3.0.CO;2-Y (PMID: 9030939)
Merritt RM, Williams MF, James TH, Porubsky ES (1997) Detection of cervical metastasis. A meta-analysis comparing computed tomography with physical examination. Arch Otolaryngol Head Neck Surg 123(2):149–152. https://doi.org/10.1001/archotol.1997.01900020027004 (PMID: 9046281)
Sun J, Li B, Li CJ, Li Y, Su F, Gao QH, Wu FL, Yu T, Wu L, Li LJ (2015) Computed tomography versus magnetic resonance imaging for diagnosing cervical lymph node metastasis of head and neck cancer: a systematic review and meta-analysis. Onco Targets Ther 8:1291–1313. https://doi.org/10.2147/OTT.S73924 (eCollection 2015. Review. PubMed PMID: 26089682; PubMed Central PMCID: PMC4467645)
Kubicek GJ, Champ C, Fogh S, Wang F, Reddy E, Intenzo C et al (2010) FDG-PET staging and importance of lymph node SUV in head and neck cancer. Head Neck Oncol 2(1):19. https://doi.org/10.1186/1758-3284-2-19 (PMID: 20637102)
Yoon DY, Hwang HS, Chang SK, Rho YS, Ahn HY, Kim JH et al (2009) CT, MR, US,18F-FDG PET/CT, and their combined use for the assessment of cervical lymph node metastases in squamous cell carcinoma of the head and neck. Eur Radiol 19(3):634–642. https://doi.org/10.1007/s00330-008-1192-6 (PMID: 18843493)
Nieuwenhuis EJC, Castelijns JA, Pijpers R, van den Brekel MWM, Brakenhoff RuudH, van der Waal I, Snow GB, Leemans CR (2002) Wait-and-see policy for the N0 neck in early-stage oral and oropharyngeal squamous cell carcinoma using ultrasonography-guided cytology: is there a role for identification of the sentinel node? Head Neck 24(3):282–289. https://doi.org/10.1002/hed.10018 (PMID: 11891961)
Thompson CF, St John MA, Lawson G, Grogan T, Elashoff D, Mendelsohn AH (2013) Diagnostic value of sentinel lymph node biopsy in head and neck cancer: a meta-analysis. Eur Arch Otorhinolaryngol 270(7):2115–2122. https://doi.org/10.1007/s00405-012-2320-0 (PMID: 23263205)
de Carvalho AC, Scapulatempo-Neto C, Maia DC, Evangelista AF, Morini MA, Carvalho AL et al (2015) Erratum: accuracy of microRNAs as markers for the detection of neck lymph node metastases in patients with head and neck squamous cell carcinoma. BMC Med 13(1):155. https://doi.org/10.1186/s12916-015-0406-4 (PMID: 26129943)
Weiss MH, Harrison LB, Isaacs RS (1994) Use of decision analysis in planning a management strategy for the stage N0 neck. Arch Otolaryngol Head Neck Surg 120(7):699–702. https://doi.org/10.1001/archotol.1994.01880310005001 (PMID: 8018319)
Mashberg A, Meyers H (1976) Anatomical site and size of 222 early asymptomatic oral squamous cell carcinomas: a continuing prospective study of oral cancer. II Cancer 37(5):2149–2157. https://doi.org/10.1002/1097-0142(197605)37:5%3c2149:AID-CNCR2820370502%3e3.0.CO;2-G (PMID: 1260707)
Kowalski LP (2002) Results of salvage treatment of the neck in patients with oral cancer. Arch Otolaryngol Head Neck Surg 128(1):58–62. https://doi.org/10.1001/archotol.128.1.58 (PMID: 11784256)
Ferlito A, Rinaldo A, Robbins KT, Silver CE (2006) Neck dissection: past, present and future? J Laryngol Otol 120(2):87–92. https://doi.org/10.1017/S0022215105004512 (PMID: 16359146)
Yuen AP, Wei WI, Wong YM, Tang KC (1997) Elective neck dissection versus observation in the treatment of early oral tongue carcinoma. Head Neck 19(7):583–588. https://doi.org/10.1002/(SICI)1097-0347(199710)19:7%3c583:AID-HED4%3e3.0.CO;2-3 (PMID: 9323146)
Kligerman J, Lima RA, Soares JR, Prado L, Dias FL, Freitas EQ et al (1994) Supraomohyoid neck dissection in the treatment of T1/T2 squamous cell carcinoma of oral cavity. Am J Surg 168(5):391–394. https://doi.org/10.1016/S0002-9610(05)80082-0 (PMID: 7977957)
Shah JP, Andersen PE (1995) Evolving role of modifications in neck dissection for oral squamous carcinoma. Br J Oral Maxillofac Surg 33(1):3–8. https://doi.org/10.1016/0266-4356(95)90077-2 (PMID: 7718525)
Bulsara VM, Worthington HV, Glenny AM, Clarkson JE, Conway DI, Macluskey M (2018) Interventions for the treatment of oral and oropharyngeal cancers: surgical treatment. Cochrane Database Syst Rev 12:CD006205. https://doi.org/10.1002/14651858.CD006205.pub4 (PMID: 30582609)
Okura M, Aikawa T, Sawai NY, Iida S, Kogo M (2009) Decision analysis and treatment threshold in a management for the N0 neck of the oral cavity carcinoma. Oral Oncol. https://doi.org/10.1016/j.oraloncology.2009.03.013 (PMID: 19457712)
Dillon JK, Villing AS, Jones RS, Futran ND, Brockhoff HC 2nd, Carlson ER et al (2019) What is the role of elective neck dissection in the management of patients with buccal squamous cell carcinoma and clinically negative neck? J Oral Maxillofac Surg 77(3):641–647. https://doi.org/10.1016/j.joms.2018.10.021 (PMID:30503978)
Capote A, Escorial V, Muñoz-Guerra MF, Rodríguez-Campo FJ, Gamallo C, Naval L (2007) Elective neck dissection in early-stage oral squamous cell carcinoma—does it influence recurrence and survival? Head Neck 29(1):3–11. https://doi.org/10.1002/hed.20482 (PMID:17103411)
D’Cruz AK, Vaish R, Kapre N, Dandekar M, Gupta S, Hawaldar R et al (2015) Head and Neck Disease Management Group. Elective versus therapeutic neck dissection in node-negative oral cancer. N Engl J Med 373(6):521–529. https://doi.org/10.1056/NEJMoa1506007 (PMID: 26027881)
Vandenbrouck C, Sancho-Garnier H, Chassagne D, Saravane D, Cachin Y, Micheau C (1980) Elective versus therapeutic radical neck dissection in epidermoid carcinoma of the oral cavity: results of a randomized clinical trial. Cancer 46(2):386–390. https://doi.org/10.1002/1097-0142(19800715)46:2%3c386:AID-CNCR2820460229%3e3.0.CO;2-9 (PMID: 6992980)
Dias FL, Kligerman J, Matos de Sá G, Arcuri RA, Freitas EQ, Farias T et al (2001) Elective neck dissection versus observation in stage I squamous cell carcinomas of the tongue and floor of the mouth. Otolaryngol Head Neck Surg 125(1):23–29. https://doi.org/10.1067/mhn.2001.116188 (PMID: 11458209)
Goto M, Hasegawa Y, Terada A, Hyodo I, Hanai N, Ijichi K et al (2005) Prognostic significance of late cervical metastasis and distant failure in patients with stage I and II oral tongue cancers. Oral Oncol 41(1):62–69. https://doi.org/10.1016/j.oraloncology.2004.06.007 (PMID: 15598587)
Huang SF, Kang CJ, Lin CY, Fan KH, Yen TC, Wang HM et al (2008) Neck treatment of patients with early stage oral tongue cancer: comparison between observation, supraomohyoid dissection, and extended dissection. Cancer 112(5):1066–1075. https://doi.org/10.1002/cncr.23278 (PMID: 18246535)
Keski-Säntti H, Atula T, Törnwall J, Koivunen P, Mäkitie A (2006) Elective neck treatment versus observation in patients with T1/T2 N0 squamous cell carcinoma of oral tongue. Oral Oncol 42(1):96–101. https://doi.org/10.1016/j.oraloncology.2005.06.018 (PMID: 16256414)
Liu TR, Chen FJ, Yang AK, Zhang GP, Song M, Liu WW et al (2011) Elective neck dissection in clinical stage I squamous cell carcinoma of the tongue: does it improve regional control or survival time? Oral Oncol 47(2):136–141. https://doi.org/10.1016/j.oraloncology.2010.11.018 (PMID: 21216182)
Zhang T, Lubek JE, Salama A, Dyalram D, Liu X, Ord RA (2014) Treatment of cT1N0M0 tongue cancer: outcome and prognostic parameters. J Oral Maxillofac Surg 72(2):406–414. https://doi.org/10.1016/j.joms.2013.05.028 (PMID: 24045188)
Massey C, Dharmarajan A, Bannuru RR, Rebeiz E (2019) Management of N0 neck in early oral squamous cell carcinoma: a systematic review and meta-analysis. Laryngoscope 129(8):E284–E298. https://doi.org/10.1002/lary.27627 (PMID: 30570760)
Amin MB, Edge SB, Greene FL et al (eds) (2017) AJCC cancer staging manual, 8th edn. Springer, New York. https://doi.org/10.1007/978-3-319-40618-3
Franceschi D, Gupta R, Spiro RH, Shah JP (1993) Improved survival in the treatment of squamous carcinoma of the oral tongue. Am J Surg 166(4):360–365. https://doi.org/10.1016/S0002-9610(05)80333-2 (PMID: 8214293)
Beenken SW, Krontiras H, Maddox WA, Peters GE, Soong S, Urist MM (1999) T1 and T2 squamous cell carcinoma of the oral tongue: prognostic factors and the role of elective lymph node dissection. Head Neck 21(2):124–130. https://doi.org/10.1002/(SICI)1097-0347(199903)21:2%3c124:AID-HED5%3e3.0.CO;2-A (PMID: 10091980)
Yii NW, Patel SG, Rhys-Evans PH, Breach NM (1999) Management of the N0 neck in early cancer of the oral tongue. Clin Otolaryngol Allied Sci 24(1):75–79. https://doi.org/10.1046/j.1365-2273.1999.00224.x (PMID: 10196656)
D’Cruz AK, Siddachari RC, Walvekar RR, Pantvaidya GH, Chaukar DA, Deshpande MS et al (2009) Elective neck dissection for the management of the N0 neck in early cancer of the oral tongue: need for a randomized controlled trial. Head Neck 31(5):618–624. https://doi.org/10.1002/hed.20988 (PMID: 19132717)
Yuen AP, Ho CM, Chow TL, Tang LC, Cheung WY, Ng RW et al (2009) Prospective randomized study of selective neck dissection versus observation for N0 neck of early tongue carcinoma. Head Neck 31(6):765–772. https://doi.org/10.1002/hed.21033 (PMID: 19408291)
Lin MJ, Guiney A, Iseli CE, Buchanan M, Iseli TA (2011) Prophylactic neck dissection in early oral tongue squamous cell carcinoma 2.1–4.0 mm depth. Otolaryngol Head Neck Surg 144(4):542–548. https://doi.org/10.1177/0194599810394988 (PMID: 21493232)
Pugazhendi SK, Thambiah L, Venkatasetty A, Thangaswamy V (2012) Elective neck dissection versus “wait and watch” policy in tongue carcinoma. J Pharm Bioallied Sci 4(6 Suppl 2):S226–S229. https://doi.org/10.4103/0975-7406.100212 (PMID: 23066257)
Tai SK, Li WY, Yang MH, Chang SY, Chu PY, Tsai TL et al (2012) Treatment for T1–2 oral squamous cell carcinoma with or without perineural invasion: neck dissection and postoperative adjuvant therapy. Ann Surg Oncol 19(6):1995–2002. https://doi.org/10.1245/s10434-011-2182-5 (PMID: 22203180)
Beltramini GA, Massarelli O, Demarchi M, Copelli C, Cassoni A, Valentini V et al (2012) Is neck dissection needed in squamous-cell carcinoma of the maxillary gingiva, alveolus, and hard palate? A multicentre Italian study of 65 cases and literature review. Oral Oncol 48(2):97–101. https://doi.org/10.1016/j.oraloncology.2011.08.012 (PMID: 21993155)
Feng Z, Li JN, Li CZ, Guo CB (2014) Elective neck dissection versus observation in the management of early tongue carcinoma with clinically node-negative neck: a retrospective study of 229 cases. J Craniomaxillofac Surg 42(6):806–810. https://doi.org/10.1016/j.jcms.2013.11.016 (PMID: 24529348)
Kelner N, Vartanian JG, Pinto CA, Coutinho-Camillo CM, Kowalski LP (2014) Does elective neck dissection in T1/T2 carcinoma of the oral tongue and floor of the mouth influence recurrence and survival rates? Br J Oral Maxillofac Surg 52(7):590–597. https://doi.org/10.1016/j.bjoms.2014.03.020 (PMID: 24840539)
Huang SF, Chang JT, Liao CT, Kang CJ, Lin CY, Fan KH et al (2015) The role of elective neck dissection in early stage buccal cancer. Laryngoscope 125(1):128–133. https://doi.org/10.1002/lary.24840 (PMID: 25043680)
Liu X, Lao X, Liang L, Zhang S, Li K, Liao G et al (2017) Neck observation versus elective neck dissection in management of clinical T1/2N0 oral squamous cell carcinoma: a retrospective study of 232 patients. Chin J Cancer Res 29(3):179–188. https://doi.org/10.21147/j.issn.1000-9604.2017.03.03 (PMID: 28729768)
Acknowledgements
We are grateful to Dr. Moustafa El Houssini (Professor of Public Health, Faculty of Medicine, Ain Shams University) for his kind support and help during statistical analysis of the data in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Ethical considerations
All procedures performed in the included articles were in accordance with the ethical standards of the institutional and the national research committee and with the 1964 Helsinki Declaration and its later amendments.
Consent
We made sure that all included articles in this study have an informed consent from all patients preoperatively.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ibrahim, S.A., Ahmed, A.N.A., Elsersy, H.A. et al. Elective neck dissection in T1/T2 oral squamous cell carcinoma with N0 neck: essential or not? A systematic review and meta-analysis. Eur Arch Otorhinolaryngol 277, 1741–1752 (2020). https://doi.org/10.1007/s00405-020-05866-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-020-05866-3