Abstract
Objective
To define a new surgical option, with lower morbidity, for the treatment of intralabyrinthine schwannomas.
Study design
Retrospective case review.
Setting
Tertiary referral centers.
Patients
Eight patients affected by an intralabyrinthine schwannoma, with or without extension to the internal auditory canal, that underwent surgery with a transcanal transpromontorial approach, were included in the study. The average age at presentation was 47 years. Patients’ characteristics, symptoms, tumor features, and surgical results were analyzed.
Interventions
All patients were diagnosed and evaluated pre-operatively with high-resolution, gadolinium-enhanced MRI and CT scan of the temporal bone, and underwent surgery via either transcanal transpromontorial endoscopic approach (TTEA) or enlarged transcanal transpromontorial endoscopic approach (ETTA).
Main outcome measures
Hearing function was evaluated with the Hearing Classification System according to the Committee on Hearing and Equilibrium Guidelines. Facial nerve function was evaluated using the House–Brackmann grading system (HB).
Results
In six patients out of eight, a TTEA was performed, whereas, due to the extension of the pathology to the cerebellopontine angle, two patients underwent an ETTA. The mean follow-up period was 15.5 months (range 1–69). No intra-operative and post-operative major complications were observed. Post-operative facial nerve function was normal in seven out of eight patients (grade I HB). One patient presented a grade II HB.
Conclusion
The endoscopic approach to cochlear schwannoma represents a good treatment option for patients and should be preferred to other more invasive surgical techniques when indicated, to reduce complications, hospitalization, and offer to patients the chance to eradicate the disease, thus avoiding the stress of a long-life radiological follow-up.
Level of evidence
4.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schwannomas of the vestibular and cochlear nerves are tumors that arise from the perineural Schwann cells. They develop in the region of ‘‘Redlich–Obersteiner’s’’ transitional zone between central and peripheral myelin until the distal end of the cochleo-vestibular nerve [1].
Intralabyrinthine schwannomas originate in the labyrinth and are a separate entity from the more common vestibular schwannomas of the internal auditory canal (IAC) that extend laterally to involve the labyrinth. Intralabyrinthine schwannomas arise from the distal branches of the cochlear, superior vestibular, or inferior vestibular nerves [2].
In 91% of cases, the most common presenting symptom is hearing loss, that can be progressive, sudden, or fluctuating. Tinnitus, facial palsy, vertigo, dizziness, and symptoms similar to Meniere’s disease are less common and, when present, they are usually preceded by hearing loss. When the lesion is exclusively intralabyrinthine, dizziness may be intractable and more intense than that characterizing a retrolabyrinthine lesion. Diagnosis and the main radiological assessments are done with a high-resolution, gadolinium-enhanced magnetic resonance imaging (MRI).
Other lesions can mimic intralabyrinthine schwannomas on contrast-enhanced MR imaging, including labyrinthitis, labyrinthitis ossificans, hemorrhage, or lipoma [3].
Several algorithms for the management of intralabirynthine schwannoma have been proposed in the literature, depending on the location, symptoms, and growth of the tumor through time: “wait-and-scan” policy, surgical excision, and radiotherapy.
The objective of our study is to define a new surgical option, with lower morbidity, for the treatment of intralabyrinthine schwannomas. In this article, we analyze our experience in the management of intralabyrinthine schwannomas using the transcanal transpromontorial endoscopic approach (TTEA), focusing on clinical presentation, surgical aspects, and results. This technique allows a complete removal of the lesion directly through the external auditory canal, using the promontorial region as surgical corridor to reach the pathology.
Materials and methods
Patients affected by an intralabyrinthine schwannoma, with or without extension to the internal auditory canal, that underwent surgery with a transcanal transpromontorial endoscopic approach (TTEA) at Referral Centers of Otolaryngology-Head and Neck Surgery Department of University Hospital of Verona and Modena, between 2012 and 2017, were included in the study.
Patients affected by intravestibular schwannomas who underwent “wait-and-scan”, radiotherapy, and tumor excision with other surgical approaches (translabyrinthine, transotic, transcochlear, and middle cranial fossa approaches) were excluded from the study.
A retrospective chart review of clinical data and videos of operations was performed in November 2017, analyzing patients’ characteristics, symptoms, tumor features, and surgical results.
Pre-operative assessment
All patients were diagnosed and evaluated pre-operatively with high-resolution, gadolinium-enhanced MRI and CT scan of the temporal bone.
Kennedy classification was used to assess schwannoma’s extension [4] (Table 1).
All the symptoms were reported. Hearing function was evaluated with the Hearing Classification System according to the Committee on Hearing and Equilibrium Guidelines [5].
Facial function was evaluated using the House–Brackmann grading system (HB) [6].
Surgical procedure (Fig. 1)
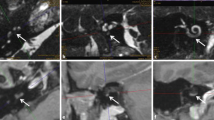
Surgical steps of TTEA. a Right ear, a view over the medial wall of the tympanic cavity after removal of the ossicular chain. b opening of the cochlea and the vestibule. The ILS can be seen inside the middle and upper turn. c Opening of the internal auditory canal with the ILS inside it. d View of the internal auditory canal after tumor removal. CT chorda tympani, FN facial nerve, OW oval window, M malleus, RWN round window niche, P promontory, V vestibule, ILS intralabyrinthine schwannoma, UT upper turn, MT middle turn, BT basal turn, IAC internal auditory canal, VN vestibular nerve, CN cochlear nerve
Intra-operative facial nerve monitoring (NIM) was used in all the cases. Surgical skin preparation was performed using 7.5% povidone iodine prepared solution. After skin injection of mepivacaine and adrenalin (20 mg/ml + 5 mcg/ml), a posterior tympanomeatal flap was elevated using a 0°, 4 mm outer diameter, 180 mm length endoscope. Ossicular chain was removed to expose the medial wall of the tympanic cavity. Using this approach, the medial wall of the tympanic cavity was used as surgical corridor to reach the inner ear. The stapes was also removed, exposing the vestibule and the spherical recess. After opening the vestibule, the promontory was drilled using the Piezosurgery® device or diamond burr, exposing the basal turn of the cochlea. A further drilling was performed uncovering the medial and the upper turns of the cochlea, exposing the tumor. In case of internal auditory canal (IAC) involvement, the fundus of the IAC was exposed and the IAC skeletonized until the porus, and then, the schwannoma was carefully removed from the IAC, preserving the facial nerve. In case of extension in the posterior vestibule, a drilling of the lateral semicircular canal was also easily possible endoscopically, through the external auditory canal (Fig. 2). In this case, the removal of the bone was performed around the tympanic portion of the facial nerve, with a subsequent surgical control of the whole vestibule and the cochlea.
Intravestibulocochlear schwannoma (case 3): a right ear, picture showing the ILS inside the vestibule after removal of the ossicular chain and opening of the cochlea. b Picture showing the involvement of the LSC after its drilling. c Tumor removal. d Surgical field after tumor removal. LSC lateral semicircular canal, FN facial nerve, ILS intralabyrinthine schwannoma, CP cochleariform process, GG geniculate ganglion, ET Eustachian tube, V vestibule
In case of cerebellopontine angle (CPA) involvement, an enlarged transcanal transpromontorial approach (ETTA) was used. In this case, a retroauricular incision with a wide circumferential EAC drilling was required, to obtain an adequate exposure of the portion of the tumor located into the CPA [7].
At the end of the tumor removal, the promontorial defect was obliterated with an abdominal fat pad harvested from the abdomen and fibrin glue, together with absorbable haemostatic material. The Eustachian tube was obliterated with temporal muscle fragments, and the tympanomeatal flap was replaced. Some absorbable gelatin compressed sponge was positioned in the external auditory canal at the end of the procedure. In case of extensive drilling of the EAC and of the medial wall of the tympanic cavity to better expose the IAC when involved by the tumor, a blind sac closure was considered.
Post-operative care
All the patients underwent an antibiotic prophylaxis using third-generation cephalosporins. The patients maintained supine position for the subsequent 48 h post-operatively.
In all cases, the post-operative pain was well tolerated using intravenous paracetamol.
After the discharge, antibiotic eardrops in the operated ear for 15–20 days were finally prescribed.
Follow-up
The patients were evaluated with otoendoscopic examination after 1 month after surgery to check the tympanic membrane healing. An MRI was always planned after 1 year from surgery.
Results
From 2012 to November 2017, eight patients affected by intravestibular schwannomas underwent tumor removal through a transcanal transpromontorial approach (Table 2). Six out of eight patients were males and two were females. The average age at presentation was 47 years. All the patients referred a history of sensorineural hearing loss; all the patients presented a pre-operative class D hearing and six out of eight patients experienced a history of tinnitus prior to treatment. Three patients out of eight also presented occasional imbalance and two patients intractable vertigo, refractory to medical treatment. No pre-operative facial palsy was noted.
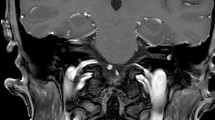
According to Kennedy classification, five out of eight subjects showed an IC schwannoma at the pre-operative MRI, one presented with an IVC schwannoma, while two showed evidence of a TMO schwannoma with the initial CPA involvement (Fig. 3).
In six patients out of eight, a transcanal transpromontorial exclusive endoscopic approach (TTEA) was performed, whereas, due to the extension of the pathology to the CPA, two patients underwent an enlarged transcanal transpromontorial endoscopic approach (ETTA) [7].
The mean follow-up period was 15.5 months (range 1–69) (Table 3). No intra-operative and post-operative (early and late) major complications were observed. Post-operative anacusis on the operated side was expected in every patient. Tinnitus disappeared in four out of six patients, while in two cases, a persistent tinnitus was referred also after surgery. Post-operative facial nerve function was normal in seven out of eight patients (87.5% grade I HB). On the other hand, due to the location of the schwannoma, one patient presented a post-operative facial nerve palsy grade II (12.5%).
Discussion
In general, acoustic neuromas are considered to be slow growing tumors (around 2 mm per year), although it has been observed that their growth rate is very random; and rather than following a geometric line, they seem to spurt unpredictably [8,9,10].
The treatment of ILS can vary depending on the location, severity of symptoms, and the behavior of the tumor with time (i.e., tumor growth and diffusion).
There are three currently accepted therapeutic options: observation (“wait-and-scan” policy), radiosurgery (RS), and surgery.
Neff et al. [2] propose, in patients with serviceable hearing and vertigo, treatment with medications or vestibular rehabilitation. In rare cases of patients with intractable vertigo, a chemical labyrinthectomy may be considered in an effort to selectively destroy vestibular function and maintain hearing for as long as possible. These authors suggest proceeding to surgical removal of the lesion when patients do not respond to conservative treatment of vertigo, despite the presence of serviceable hearing, because the natural course of these lesions generally leads to severe hearing impairment. In their opinion, even severe tinnitus associated with non-serviceable hearing can be an indication for surgery, making the patient aware of the possible persistence of tinnitus [2].
Wait-and-scan policy
As hearing preservation is not a surgical goal in these cases, the main strategy proposed to patients with serviceable hearing without intractable vertigo in the past years has been observation with serial MR imaging [2]. In particular, the protocol proposed for the “wait-and-scan” approach requires, after the diagnosis, the repetition after 12 months of a MRI of the middle ear and CPA with contrast, then every 2 years if no growth is showing.
Radiosurgery
In the literature, there is lack of consensus on radiotherapy for the treatment of these lesions and, usually, it is offered but not recommended, except in the elderly or those unfit for surgery [1].
According to Karpinos et al. [11], the classic indications for RS therapy are a tumor measuring less than 3 cm and at least one of the following concurrent criteria: progressive symptoms in patients over 40, associated comorbidity, tumor in the only ear with useful hearing, bilateral AN, post-surgical recurrence, or rejection of surgery.
RS can thus be considered a viable option for ILSs treatment in patients with poor health conditions exhibiting tumor growth, but that are not eligible for surgical treatment.
Unlike surgery, the objective of RS is to halt the growth of the tumor by causing avascular necrosis with subsequent deposition of collagen [12].
The first RS treatment for AN was applied by Leksell [13, 14] in 1971, but complications such as hearing loss (most frequently), weakness and loss of facial sensitivity, tinnitus, loss of balance, headache, dysarthria, dysphagia, cystic necrosis, and hydrocephaly were showed [11].
Surgical approaches
Surgery may be indicated when intralabyrinthine schwannomas begin to show evidence of extension into the IAC [2, 15]. For some authors, surgery becomes the treatment of choice when the schwannoma develops toward the CPA or the middle ear [5].
Other indications for surgery include non-serviceable hearing, intractable vertigo or uncertainty regarding the diagnosis. Serviceable hearing is defined as a PTA > 50 dB or an SDS > 50% [2]. As intravestibular schwannoma surgery implicates an opening of the otic capsule with a subsequent loss of perilymph, a post-operative loss of any residual hearing is expected. Exceptionally, Lee et al. described a rare case of schwannoma involving lateral and superior semicircular canals with an improvement of hearing function after surgical resection [16].
The surgical options traditionally meant to treat intralabirinthine schwannomas are: translabirinthine (TL), transotic (TO), and middle cranial fossa approach (MCF), depending on the localization and extension of the tumor.
The TL approach is traditionally the most direct route to reach the internal auditory canal (IAC) and cerebellopontine angle (CPA), and can be performed in cases of posterior intralabyrinthine schwannomas (vestibule or semicircular canals). It is reserved for patients with no serviceable hearing left, as it involves sacrifice of residual hearing. The TO approach represents an anterior extension of the translabyrinthine approach via drilling of the anterior and posterior labyrinth, without the need for facial nerve rerouting, and can be reserved for treating intralabirintine or intracochlear schwannomas.
Recently, some authors have proposed a cochlear schwannoma removal with facial bridge cochleostomy associated with the translabyrinthine approach [17]. This approach requires skeletonization of the first and second portions of the fallopian canal on their labyrinthine aspect. Then, the basal turn is exposed using the floor of the IAC and the vestibule as landmarks.
These approaches require a wide retroauricolar incision, as well as an extendend mastoidectomy meant to expose the MCF e PCF dura.
In cases of small intracochlear lesions, a cochleostomy by posterior tympanotomy is possible [4]. Some authors described a transcanal microscopic approach [17] to remove very small intracochlear lesions without extension to the vestibule or internal auditory canal.
The traditional microsurgery is reported to have a high complication rate (59.5%), surgical (28.2%), neurological (26.2%), and medical (5.1%), the main factors for increased complications incidence being sex and race (i.e., non-Caucasian females), presence of comorbidities, and the practice of surgery in hospitals with low volume of patients [18].
The mortality rate of the procedure is 0.2% and complete resection of the tumor is not achieved in 11.7% of the cases undergoing microsurgery [18, 19], especially due to difficulty to check hidden areas under the straight view provided by the microscope.
Endoscopic approaches to middle ear represent the new tendency for otologic surgery as they grant removal of middle ear diseases through a minimally invasive approach, reducing the time of hospitalization and complications. Nowadays, endoscopic approaches to the internal auditory canal for vestibular schwannomas are new and innovative approaches to lateral skull base [20, 21].
There have already been published case series of endoscopic approaches to the lateral skull base and preliminary results, confirming (even if initially) radicality and effectiveness of surgery [22].
In our opinion, the indications for surgical treatment of intravestibular schwannoma are symptomatic patients (intractable vertigo, non-serviceable hearing, and intolerable tinnitus), radiologically demonstrated growing lesions, large schwannomas with CPA extension (KOOS stage II).
There is evidence of several advantages of the endoscopic transpromontorial approach to cochlear schwannoma, such as reduced time of surgery as opposed to the traditional microscopic technique. Using the natural orifice over the middle ear provided by the EAC, it is possible to reach the promontory (and thus, the cochlea) directly, without the need for wide incisions or extensive drilling of the mastoid. Moreover, the transpromontorial approach does not require exposure or manipulation of the MCF or PCF dura, reducing hospitalization and morbidity.
Transcanal transpromontorial approach allows controlling the entire cochlea and the entire internal auditory canal to the porus, and therefore, with the optimization of the surgical technique, this approach may become the treatment of choice, especially for this type of schwannomas.
The endoscopic view provides the opportunity to constantly monitor the facial nerve during surgery, lowering the chance of unintentional damage.
In our series, patients who were treated with the transcanal transpromontorial approach for cochlear schwannoma presented no major short- or long-term complications, and showed a good outcome for facial nerve function after surgery (seven out of eight patients showed grade I HB function and one patient grade II HB). Since the technique has been only recently introduced, the number of cases treated is still small and a longer follow-up is needed to assess the long-term results of this kind of surgery.
The main disadvantage caused by the endoscopic transcanal transpromontorial route to the IAC is represented by the impossibility to preserve the cochlea during the procedure. This does anyway appear a minor problem: in fact, as previously stated, in most cases, cochlear schwannomas present with impaired or unserviceable hearing at time of diagnosis, and tend to have a progression towards anacusis with time. Moreover, in the surgical treatment of cochlear schwannoma, it is mandatory to open the cochlea to remove the tumor occupying the cochlea itself.
Conclusions
The transcanal transpromontorial approach can be considered a good option in the management of cochlear schwannoma, as it represents a minimally invasive procedure. In particular, it can be considered a viable option for young patients with long-life expectancy that tend to reckon wait-and-scan option as excessively stressful or frustrating, as well as for patients that show growth of the lesion during follow-up.
In conclusion, the endoscopic approach to cochlear schwannoma represents a good treatment option for patients and should be preferred to other more invasive surgical techniques when indicated, to reduce complications, hospitalization and offer to patients the chance to eradicate the disease, thus avoiding the stress of a long-life radiological follow-up.
References
Bouchetemble P et al (2013) Intralabyrinthine schwannomas: a case series with discussion of the diagnosis and management. Otol Neurotol 34(5):944–951
Brian A, Neff TOW Jr, Sataloff RT (2003) Intralabyrinthine schwannomas. Otol Neurotol 24:299–307
Salzman KL et al (2012) Intralabyrinthine schwannomas: imaging diagnosis and classification. AJNR Am J Neuroradiol 33(1):104–109
Kennedy RJ et al (2004) Intralabyrinthine schwannomas: diagnosis, management, and a new classification system. Otol Neurotol 25(2):160–167
Anonymous (1995) Committee on Hearing and Equilibrium Guidelines for the evaluation of hearing preservation in acoustic neuroma (vestibular schwannoma). American Academy of Otolaryngology-Head and Neck Surgery Foundation. INC. Otolaryngol Head Neck Surg 113(3):179–180
House JW, Brackmann DE (1985) Facial nerve grading system. Otolaryngol Head Neck Surg 93(2):146–147
Presutti L et al (2017) Expanded transcanal transpromontorial approach to the internal auditory canal: pilot clinical experience. Laryngoscope 127(11):2608–2614
Hoistad DL et al (2001) Update on conservative management of acoustic neuroma. Otol Neurotol 22(5):682–685
Mirz F et al (1999) Investigations into the natural history of vestibular schwannomas. Clin Otolaryngol Allied Sci 24(1):13–18
Stangerup SE et al (2004) Increasing annual incidence of vestibular schwannoma and age at diagnosis. J Laryngol Otol 118(8):622–627
Karpinos M et al (2002) Treatment of acoustic neuroma: stereotactic radiosurgery vs. microsurgery. Int J Radiat Oncol Biol Phys 54(5):1410–1421
Shaw EG, Coffey RJ, Dinapoli RP (1995) Neurotoxicity of radiosurgery. Semin Radiat Oncol 5(3):235–245
Leksell L (1983) Stereotactic radiosurgery. J Neurol Neurosurg Psychiatry 46(9):797–803
Leksell DG (1987) Stereotactic radiosurgery. Present status and future trends. Neurol Res 9(2):60–68
Doyle KJ, Brackmann DE (1994) Intralabyrinthine schwannomas. Otolaryngol Head Neck Surg 110(6):517–523
Lee JJ et al (2015) Recovery of hearing after surgical removal of intralabyrinthine schwannoma. Laryngoscope 125(8):1968–1971
Mazzoni A et al (2017) Acoustic schwannoma with intracochlear extension and primary intracochlear schwannoma: removal through translabyrinthine approach with facial bridge cochleostomy and transcanal approach. Eur Arch Otorhinolaryngol 274(5):2149–2154
Mahboubi H et al (2014) Complications of surgery for sporadic vestibular schwannoma. Otolaryngol Head Neck Surg 150(2):275–281
Coca A, Gómez JR, Llorente JL, Rodrigo JP, Núñez F, Sevilla MA et al (2007) Complicaciones y secuelas en la cirugía de los neurinomas del acústico. Acta Otorrinolaringol Esp 58:470–475
Marchioni D et al (2015) Endoscopic transcanal corridors to the lateral skull base: initial experiences. Laryngoscope 125(Suppl 5):S1–S13
Wick CC, Arnaoutakis D, Barnett SL, Rivas A, Isaacson B (2017) Endoscopic transcanal transpromontorial approach for vestibular schwannoma resection: a case series. Otol Neurotol 38(10):490–495
Presutti L et al (2017) Expanded transcanal transpromontorial approach to the internal auditory canal and cerebellopontine angle: a cadaveric study. Acta Otorhinolaryngol Ital 37(3):224–230
Funding
The present authors have no financial relationship to disclose.
Author information
Authors and Affiliations
Contributions
All of the authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Marchioni, D., De Rossi, S., Soloperto, D. et al. Intralabyrinthine schwannomas: a new surgical treatment. Eur Arch Otorhinolaryngol 275, 1095–1102 (2018). https://doi.org/10.1007/s00405-018-4937-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-018-4937-0