Abstract
Background
Incidences of pharyngocutaneous fistulization (PCF) after total laryngectomy (TL) reported in the literature vary widely, ranging from 2.6 to 65.5%. Comparison between different centers might identify risk factors, but also might enable improvements in quality of care. To enable this on a national level, an audit in the 8 principle Dutch Head and Neck Centers (DHNC) was initiated.
Methods
A retrospective chart review of all 324 patients undergoing laryngectomy in a 2-year (2012 and 2013) period was performed. Overall PCF%, PCF% per center and factors predictive for PCF were identified. Furthermore, a prognostic model predicting the PCF% per center was developed. To provide additional data, a survey among the head and neck surgeons of the participating centers was carried out.
Results
Overall PCF% was 25.9. The multivariable prediction model revealed that previous treatment with (chemo)radiotherapy in combination with a long interval between primary treatment and TL, previous tracheotomy, near total pharyngectomy, neck dissection, and BMI < 18 were the best predictors for PCF. Early oral intake did not influence PCF rate. PCF% varied quite widely between centers, but for a large extend this could be explained with the prediction model. PCF performance rate (difference between the PCF% and the predicted PCF%) per DHNC, though, shows that not all differences are explained by factors established in the prediction model. However, these factors explain enough of the differences that, compensating for these factors, hospital is no longer independently predictive for PCF.
Conclusions
This nationwide audit has provided valid comparative PCF data confirming the known risk factors from the literature which are important for counseling on PCF risks. Data show that variations in PCF% in the DHNCs (in part) are explainable by the variations in these predictive factors. Since elective neck dissection is a major risk factor for PCF, it only should be performed on well funded indication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pharyngocutaneous fistulization (PCF) is a frequent and serious complication after total laryngectomy (TL). It increases morbidity, prolongs hospitalization, potentially necessitates additional surgery, delays or interrupts oral feeding and voice rehabilitation, and raises costs [1,2,3]. Reported incidences of PCF in the literature vary widely from 2.6 to 65.5% [4].
Many prognostic factors for PCF have been described in the literature. The main are prior (chemo)radiotherapy [(C)RT], hypopharyngeal cancer, (extensive) pharyngeal resection and reconstruction, neck dissection, and comorbidities [1, 2, 4,5,6,7]. It is still disputed which factors are most relevant and which could be influenced to decrease the incidence of PCF. These are important issues for pretreatment counseling and health economic decisions [7]. Furthermore, data usually come from single-institution series, which makes a valid interinstitutional comparison impossible. Such a comparison of complications would be relevant to gain better insight in the quality of care for patients undergoing TL on a national level, but can also lead to changes in treatment protocols in individual institutes. Grau et al., using the national Danish Head and Neck Study Group dataset, did identify prognostic factors for PCF in TL patients with prior radiotherapy (RT). However, no comparisons between the different centers in their analysis were conducted [8]. There is evidence though, that multicenter comparison with proper documentation and feedback on complications in surgery can lead to improved quality and reduced costs [9].
To enable such comparison on a national level, interinstitutional nationwide audits are indispensable. Recently the Dutch Head and Neck Society (DHNS) have started a prospective national audit that eventually will lead to benchmarking and hopefully further improved patient care. In the present study we performed a retrospective chart study, supported by all 8 principle Dutch Head and Neck Centers (DHNC) affiliated to the Dutch Head and Neck Society (DHNS) in a 2-year (2012 and 2013) cohort of TL patients. In this study we not only aimed to identify the incidence of PCF per center, but also to establish the factors predictive for PCF, and to develop a prognostic model predicting the PCF% per center. To provide possibly informative data not covered by the chart study, a survey among the head and neck surgeons of the participating centers was carried out as well.
Methods
Retrospective chart study
Patient selection
All patients (n = 324), who underwent a total laryngectomy in the participating centers between January 2012 and December 2013 were included in the study. The total number of TL procedures per DHNC ranged from 17 to 70 (17, 22, 32, 39, 40, 50, 54, and 70, respectively). Four patients were excluded from the analysis, because they died (without PCF) on day 1, 3, 4, and 6, respectively, leaving 320 patients for further analysis.
Data collection
Patient characteristics agreed to collect in the chart review were age, gender, ASA (American Society of Anesthesiologists) score, diabetes, BMI (body mass index), smoking and alchohol history, albumin, hemoglobin, site of primary tumor, T and N classification, prior treatment [e.g., prior C(RT)] and interval between TL and prior treatment. Surgical data collected concerned the indication for TL, previous tracheotomy, extent of pharyngectomy, type of reconstruction, extent of neck dissection [no, selective; unilateral or bilateral and (modified) radical; unilateral or bilateral] use of antibiotics and tracheoesophageal puncture (TEP). Postoperative data were timing of oral intake, timing of speech rehabilitation, hospitalization time, and occurrence, timing and management of PCF. Medical records were retrospectively reviewed by the first author with supervision in each center. This study does not fall under de scope of the Medical Research Involving Human Subjects Act, which was confirmed by the institutional review board (MREC 17.0439).
Survey
Thirty-five head and neck surgeons (members of the DHNS) were invited to participate in a survey about pre-, peri-, and postoperative management concerning TL. 27 (77%) of these surgeons, representing all 8 participating centers, returned their completed questionnaires. Answers in this questionnaire were used to complete data lacking in the chart review. This concerned data on the pharyngeal closure method, because this information was not always well-documented in the surgical reports. And data on the institution’s oral intake protocol, which was used in the analysis of the possible influence of early oral intake on PCF formation [3, 10,11,12].
End points
Primary endpoints for this study were incidence of PCF (occurring within 30 days after discharge), predictive factors for PCF and predicted PCF% per DHNC [13]. As routine swallow X-ray was not performed in all centers, a PCF was recorded when clinically and/or fluoroscopically evidenced. PCF within 14 days after TL was the primary endpoint in a separate analysis pertaining to the role of the (early/late) oral intake protocol.
Statistical analyses
Identification of predictive factors for PCF
IBM SPSS Statistics 22.0 was used to conduct the analyses. Descriptive statistics were computed and additionally univariable and multivariable analyses (using binary logistic regression analysis) were carried out to assess predictive factors for PCF. Factors that were univariably predictive for PCF at a significance level of 10% (2-sided) were initially included in the multivariable logistic regression analysis, which was then further refined using backward elimination. Odds ratios (ORs) and 95% confidence intervals (CIs) of the final model were calculated. Because of multicollinearity between origin of index tumor, pharyngectomy reconstruction, and TEP, only pharyngectomy was kept in the multivariable analysis. It was decided a priori to keep BMI in the final multivariable model regardless it’s predictive value in the current cohort, because its (potential) importance has been described in the literature [2, 14]. Albumin level was excluded from the multivariable analysis because of missing data in 145 (45%) of the patients. As comorbidity was not routinely scored in most of the participating centers in 2012 and 2013, we used the ASA score as a surrogate [15, 16]. In assessing the effect of the interval between (C)RT and TL on PCF formation, we deemed a cut-off point of 30 months clinically relevant. This resulted in one final newly created variable with five levels: no prior (C)RT, RT 0–30 months (mo) before TL, RT 31–444 mo, CRT 0–30 mo, CRT 31–444 mo [1].
Predicted PCF percentages per center
Predicted probabilities on PCF per patient were calculated from the final multivariable logistic regression model. Overall PCF% for all centers and predicted PCF% per center were compared with the observed PCF% per center. When striking differences were observed, we searched both patient data and answers to the survey question about management of pharynx closure for possible explanations.
Role of time from TL to oral intake
The possible effect of timing of oral intake on PCF was analysed univariably and multivariably using PCF within 14 days after TL as outcome variable and initiation of oral intake according to the Institutional protocol as predictor, treating the previously identified predictive factors on PCF as covariates. PCF within 14 days after TL was used as the endpoint for this analysis, because we assume that oral intake mainly can influence the development of PCF in an early postoperative stage.
Two groups were created: an early group (oral intake within 3 days after TL) consisting of all patients in hospitals D and E and late group (oral intake > 3 days after TL) consisting of the patients in the remaining hospitals. The analysis was also conducted with the cut-off point set on 6 days used in hospital H, resulting in an early group with an oral intake ≤ 6 days, and a late group with oral intake after > 6 days.
Results
Retrospective chart study
Patient and tumor characteristics
The cohort consisted of 255 (80%) men and 65 (20%) women. The mean age at time of TL was 63.3 years (SD 9.8 years). Smoking data were available for 299 and missing for 21 patients. 21 patients never consumed tobacco and 278 did. Of this latter group, 143 continued until date of TL and 135 had stopped already. Alcohol abuse was reported by 125 patients, social alcohol consumption by 138, no alcohol consumption ever by 4, and for 53 patients these data were missing. In 217 patients (68%) the tumor was located in the larynx, in 73 (23%) in the hypopharynx, in 29 (9%) the primary tumor was outside these two locations (the ‘miscellaneous’ group), and in 1 (0.3%) the indication for TL was non-malignant disease (recurrent pneumonia). The ‘miscellaneous’ group consisted patients with oropharynx cancer (n = 11), larynx sarcoma (n = 6), thyroid cancer (n = 6), oral cavity cancer (n = 2), esophageal cancer (n = 1), neuroendocrine larynx tumor (n = 1), adenoid cystic carcinoma of the trachea (n = 1), and a clivus meningioma (n = 1). Primary TL was conducted in 117 patients (37%), salvage TL in 138 patients (43%), TL for a second primary in 42 patients (13%) and TL for a dysfunctional larynx in 23 patients (7%). Of the 203 ‘non-primary’ TL patients, 140 patients had prior RT, 50 prior CRT, 12 other cancer treatments, and 1 non-malignant indication for TL. A detailed overview of patient and tumor characteristics can be found in Table 1.
Surgical aspects
Standard TL was performed in 212 patients (66%). 69 patients (22%) underwent near total pharyngectomy and 39 (12%) circumferential pharyngectomy in conjunction with TL. Reconstruction was performed in 127 patients. This concerned reinforcement of the pharynx with a pectoralis major (PM) flap without skin island in 19 patients (6%). Reconstruction of the near total pharyngeal defect with a PM-flap with skin island in 59 patients, and a free flap in 10 [radial forearm flap (RFF) 9, anterolateral thigh (ALT) 1]. The 39 circumferential pharyngeal defects were reconstructed with a tubed PM-flap with skin island (n = 1), a free flap (n = 10; RFF 4, ALT 5, internal mammary artery perforator n = 1), gastric pull-up (n = 18), or free jejunum transfer (n = 9). In 1 patient a planned oropharyngeal-cutaneous fistula was made, whereas this patient also had a PM-flap without skin island.
Selective neck dissection was performed in 110 patients (34%) and (modified) radical neck dissection in 67 patients (21%), 50 at the time of TL and 17 at an earlier date. Of the 141 patients (44%) without neck dissection, node sampling for frozen section was conducted in 36, and these patients were also categorized as ‘no neck dissection’. In two patients neck dissection data were missing.
Primary TEP with insertion of an indwelling voice prosthesis was performed in 261 patients (82%), secondary TEP in 37 (12%), and in 22 (7%) no TEP was performed.
Pharyngocutaneous fistulization
The overall incidence of PCF within 30 days after discharge from the hospital was 25.9% (83/320). After these 30 days, 4 more patients developed PCF, in 3 at day 51, 58, 131, respectively, and in 1 PCF occurred in the “postoperative radiotherapy period”, which we also deemed to be more than 30 days after patient’s discharge at day 12 postoperatively. The incidence of PCF in patients treated with primary TL was 24.8% (29/117), with salvage TL 22.5% (31/138), with TL for a second primary 35.7% (15/42) and with TL for a dysfunctional larynx 34.8% (8/23) (P = 0.264). The median day of PCF manifestation was day 12 (range 1–48 after surgery). 66 of the 83 PCF patients were treated conservatively (79.5%) and 17 required additional surgery (20.5%). In 15 of these 17 patients, flap reconstruction was used (PM 14; ALT 1), resuturing of the pharyngeal defect (1), or surgical exploration only (1). Median time between PCF and additional surgery was 14.0 days (range 0-172). Sixty-five patients (78.3%) were discharged with a cured PCF, and 18 with a persisting PCF (21.7%). Median hospitalization time for patients without PCF was 13 days (range 7–45) and for patients with PCF 20 days (range 8–80) (P < 0.001). Median hospitalization time for conservatively treated PCF patients was 17 days (range 8–68) and for patients with surgically treated PCF this was 35.5 days (range 7–80) (P = 0.012).
Univariable analyses: prognostic factors for PCF
Univariable logistic regression analyses, to identify prognostic factors for PCF, were conducted for gender, age, site of index tumor, diabetes, BMI (n = 316), ASA score, preoperative albumin level (n = 176), preoperative hemoglobin level (n = 284), prior (C)RT, time between prior (C)RT and TL, pharyngectomy, reconstruction, neck dissection, TEP and previous tracheotomy. Factors predictive for PCF were: index tumor, i.e., hypopharynx vs larynx (OR 3.25; 95% CI 1.83–5.76; P < 0.001), BMI < 18 (OR 2.64; 95% CI 1.16-6.00; P = 0.02), albumin level ≤ 40 g/L (OR 1.79; 95% CI 0.92–3.48; P = 0.087), prior CRT (OR 2.51; 95% CI 1.26-5.00; P = 0.009), increased time between prior (C)RT and TL [OR 1.10 (per 1 year increase); 95% CI 1.02–1.17; P = 0.003], near total pharyngectomy (OR 3.86; 95% CI 2.13–6.98; P < 0.001), circumferential pharyngectomy (OR 2.96; 95% CI 1.42–6.17; P = 0.004), reconstruction (all types of reconstruction vs no reconstruction OR 3.62; 95% CI 2.15–6.11; P < 0.001), neck dissection, i.e., selective (OR 2.30; 95% CI 1.26–4.19; P = 0.007) and radical (OR 3.05; 95% CI 1.57–5.95; P = 0.001), secondary TEP and no TEP vs primary TEP (OR 3.83; 95% CI 1.58–9.31; P = 0.003, and OR 3.63; 95% CI 1.78–7.39 P < 0.001, respectively), and tracheotomy (OR 1.83; 95% CI 1.04–3.21; P = 0.036). Prior RT as single-modality treatment is not a significant prognostic factor for PCF compared to no (C)RT (OR 0.87; 95% CI 0.49–1.54, P = 0.635). Smoking (OR 2.25; 95% CI 0.63–8.06; P = 0.213) and discontinuing smoking (OR 1.86; 95% CI 0.52–6.74; P = 0.342) are not predictive for PCF compared to no smoking. A history of alcohol abuse compared to no/social drinking (OR 1.19; 95% CI 0.68–2.06; P = 0.542) also is not predictive for PCF. Details are summarized in Table 2. Table 3 provides an overview of the variations in the DHNC cohorts regarding these significant prognostic factors for PCF.
Multivariable analysis: final prognostic factors for PCF
The multivariable prediction model revealed that prior (C)RT combined with the time interval between TL and prior (C)RT, pharyngectomy, neck dissection and previous tracheotomy were the best predictors for development of PCF. Patients with BMI < 18 had a significantly increased risk on PCF (OR 2.70; 95% CI 1.06–6.90; P = 0.038). Patients with RT and CRT ≥ 31 months before TL and patients with CRT ≤ 30 months before TL were more likely to develop PCF (OR 2.34; 95% CI 1.01–5.43; P = 0.048/OR 5.14, 95% CI 1.13–23.42; P = 0.034 and OR 2.32; 95% CI 1.00–5.38; P = 0.049, respectively) compared to patients with no (C)RT. The other factors associated with PCF were: near total pharyngectomy (OR 2.61; 95% CI 1.33–5.15; P = 0.006), selective and radical neck dissection (OR 2.51; 95% CI 1.23–5.12; P = 0.011, and OR 2.70; 95% CI 1.18–6.15; P = 0.018, respectively) and previous tracheotomy (OR 2.02; 95% CI 1.07–3.79; P = 0.029) (Table 4).
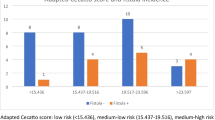
PCF performance rate
For a meaningful comparison of the differences in the PCF percentages, the clinical and surgical differences in the patient cohorts of the 8 DHNC were taken into account. Table 5 shows per DHNC the actual PCF%, the difference between this PCF% and the overall PCF%, the PCF% corrected for predictive (risk) factors found in the multivariable analysis, and the difference between the predicted PCF% and the observed PCF%, called the PCF performance rate. The mean PCF% was higher than the overall mean in centers C and G, close to the overall mean in centers E, F and H, and lower in centers A, B and D.
The predicted PCF% (correction based on the multivariable logistic regression model) was higher than the overall mean PCF% in centers C, E, G and H, indicating that these centers serve a patient population with a higher risk of developing PCF or use surgical techniques implicating a higher risk (such as elective neck dissection). In these DHNCs, patients with BMI < 18, prior CRT (and increased time between prior CRT and TL), previous tracheotomy, extensive pharyngectomy and selective or radical neck dissection occur more than average, as also can be seen in Table 3.
The last column in Table 5 shows the PCF performance rate per DHNC, which is the difference between the actual PCF% and the predicted PCF%. This shows that not all differences are explained by factors established in the prediction model. However, it is also clear that the differences corrected for the predictive (risk) factors are considerably smaller than the differences seen in the third column. Indeed, the predictive factors identified here explain enough of the differences that, compensating for these factors, hospital is no longer independently predictive for PCF (P = 0.380). The PCF performance rates are visualized in Fig. 1.
Data used from the national survey
Pharyngeal closure
Techniques for primary pharyngeal closure differ widely between centers and head and neck surgeons. Nine of 27 who filled in the survey close the pharynx vertically, 14 in a Y/T fashion, and 4 horizontally.
Oral intake
Two centers (D and E) were using an early oral intake protocol, which means initiation of oral intake within 3 days postoperatively. The remaining hospitals were using a late(r) oral intake protocol, varying from starting oral intake at day 6–12. Combining this information with data from the retrospective chart study revealed that patients who started early with oral intake according to the protocol did not have an increased risk on PCF within 14 days after TL compared to patients who started late with oral intake according to the protocol (OR 1.11; 95% CI 0.57–2.17; P = 0.752). This result was comparable in a model together with the final predictive factors (OR 1.14; 95% CI 0.54–2.41; P = 0.736). One center (H) started oral intake according to protocol on day 6 after TL. Adding this center to the ‘early oral intake group according to the protocol’ did not affect this result.
Discussion
This nationwide 2-year audit on postoperative complications of TL showed that PCF still is a significant problem. The overall incidence of 25.9% is comparable to figures reported in the literature [1, 7, 17]. At first sight, there is a considerable variation in PCF% between the participating centers. The analysis based on the multivariable prediction model shows that in part these differences in PCF% are explainable by variations regarding the significant risk factors for PCF. Factors predicting PCF are prior (C)RT in combination with prolonged lead time to TL, near total pharyngectomy, selective neck dissection, radical neck dissection, previous tracheotomy, and BMI < 18. These factors are also in line with earlier studies on the risk for PCF manifestation [1, 2, 4, 5, 18].
The most interesting aspect of this study is that it allows for a detailed comparison between the participating centers. When observing the actual PCF% in the third column in Table 5, the variation is much wider than the variation in the PCF performance shown in the last column of this table. This means that in the center with the lowest incidence of PCF, this incidence is (in part) so low because the identified risk factors are more favorable. Vice versa, centers with a higher PCF% have less favorable risk factors in their population. There are some exceptions, though, with centers showing better PCF performance than predicted (e.g., center A), and centers still less favorable than predicted (e.g., center C). This means that not all differences are explainable with the multivariable prediction model. Center C, for example, besides having a less favorable patient population more patients requiring TL for a dysfunctional larynx (11.4% vs 6.7% in the other centers) and more jejunum reconstructions (10.0% vs 0.8% in the other centers), is also the only one where the majority of the pharynx closures were done horizontally. This might be an explanation of the difference in predicted and observed fistula rate in that center. In this respect, it is somewhat disappointing that information about the closure technique was often not available in sufficient detail. Therefore we only can speculate about the relevance of pharynx closure based on the survey data. However, there are other reports showing that T-shaped closure reduces the incidence of PCF [19].
The prognostic factors found in this study are comparable with those reported in the literature. Dedivitis et al. described a 6% increase in PCF risk in patients who underwent neck dissection [5]. The underlying rationale for this increased risk is that a neck dissection further diminished the vascularity in the operation field, making the remaining tissues more susceptible for infection or poor healing just because of a lack of sufficient perfusion. We also found that both types of neck dissection, selective and radical, are associated with an increased risk on PCF. Management of the N0 neck in patients with advanced stage larynx cancer and management of the N0 neck in salvage patients (with prior N0/N + neck) is still a matter of controversy and the final choice of treatment (no neck dissection/node sampling, or selective neck dissection) is ‘surgeon and center dependent’ [20, 21]. According to the Dutch National Guideline on Laryngeal Carcinoma node a node sampling procedure (instead of a selective neck dissection) can be performed during a primary TL for advanced disease without clinical or radiological evidence of positive lymph nodes in case postoperative radiotherapy is planned or in case of salvage surgery with no evidence of regional metastases and no history of lymph node metastases [22]. This means that the choice for selective neck dissection should be weighed against the higher PCF risk and the option of node sampling for frozen section should be discussed [23]. Obviously, in case of suspicion or evidence of metastatic lymph node involvement there is no choice and neck dissection is indicated.
The finding that previous tracheotomy is predictive for PCF is not very surprising, since this condition forms an additional infection risk and for complicated wound healing. This means that if tracheotomy is avoidable, e.g., by performing a TL ‘a chaud’, that is worthwhile considering. Patients with BMI < 18 were more likely to develop PCF compared to patients with healthy BMI, which is supported by earlier studies describing poor nutritional status as a predictive factor [14, 24]. Certainly in patients in whom there is time to improve nutritional status and condition, such as in case of a TL for a dysfunctional larynx, this should be employed. Interestingly, ASA score at the time of TL had no significant correlation with PCF%. Although ASA score has been reported to be a reasonable surrogate parameter for comorbidity [15, 16], it is not as representative for comorbidity as for example, the ACE-27 score, that is nowadays used in all DHNC centers [25]. However, these data were not yet available in most of the centers in 2012–2013, and hence, ASA was included in the study protocol, with the advantage that the ASA data in this study were available (from anesthesia reports) for the vast majority of the patients.
Lastly, prior (C)RT is frequently described in the literature as prognostic factor for PCF [4, 5, 7, 8, 26]. In the present study, prior CRT was a significant predictior for the development of PCF in univariable analysis [27]. RT as single-modality treatment was not significantly associated with a higher risk of PCF. Interestingly, however, when taking time since prior treatment into account (≤ 30 vs > 30 months), the multivariable analysis showed that also RT was a significant predictor for the development of PCF, as can be seen in Table 4.
The possible influence of oral intake was also examined in this study and, in accordance with other studies, we did not find an association between early oral intake and the development of PCF [3, 10, 11, 28]. Therefore, also the present study suggests that an early oral intake protocol after TL is a safe policy enabling earlier discharge and potentially positively influences the patients’ feeling of normalcy [3].
A strong aspect of this audit is that there was no selection bias as all TLs performed in the 8 centers were used in this analysis. A limitation of this study is that collection of 2-year oncologic outcome data, such as regional control and survival, was not part of the audit protocol. These data are of course indispensable for the final verdict on the best treatment strategy concerning the neck, i.e., the choice between node sampling for frozen section (associated with a decreased the risk on PCF) or selective neck dissection in the cN0 cases. It has to be kept in mind that this audit concerns a retrospective analysis and that not all surgical, clinical and comorbidity data were available. Moreover, the definition of a PCF might have caused some differences as in centers where swallow X-rays are only made in case of clinical suspicion, subclinical fistulas might have been missed. However, we did not find a difference in either the time of fistula occurrence nor in the management between centers employing routine swallow X-rays and those performing them in case of suspicion only.
In conclusion, this nationwide audit has provided valid comparative PCF data from the participating DNHCs, confirming the known risk factors from the literature. These data are useful for counseling on PCF risks. Data show that variations in PCF% in the DHNCs (in part) are explainable by the variations in these identified predictive factors. Standardized detailed surgical reporting is important to acquire more relevant data to identify additional PCF risk factors, and future audits will hopefully lead to a reduction in the PCF rate. Based on the current analysis, the optimal approach of the neck with, especially the use of elective neck dissection, which is a major risk factor for PCF, needs further consideration. The prognostic benefit of elective neck dissection when the patient needs postoperative (C)RT has never been proven. Additionally, the need for elective neck dissection in the salvage setting of a clinically negative neck has never been proven, especially when the neck previously was irradiated electively. We therefore advise to refrain from neck dissections when the risk of occult metastases is low.
References
Hasan Z, Dwivedi RC, Gunaratne DA, Virk SA, Palme CE, Riffat F (2016) Systematic review and meta-analysis of the complications of salvage total laryngectomy. Eur J Surg Oncol 43(1):42–51
Timmermans AJ, Lansaat L, Theunissen EA, Hamming-Vrieze O, Hilgers FJ, van den Brekel MW (2014) Predictive factors for pharyngocutaneous fistulization after total laryngectomy. Ann Otol Rhinol Laryngol 123(3):153–161
Timmermans AJ, Lansaat L, Kroon GV, Hamming-Vrieze O, Hilgers FJ, van den Brekel MW (2014) Early oral intake after total laryngectomy does not increase pharyngocutaneous fistulization. Eur Arch Otorhinolaryngol 271(2):353–358
Paydarfar JA, Birkmeyer NJ (2006) Complications in head and neck surgery: a meta-analysis of postlaryngectomy pharyngocutaneous fistula. Arch Otolaryngol Head Neck Surg 132(1):67–72
Dedivitis RA, Aires FT, Cernea CR, Brandao LG (2015) Pharyngocutaneous fistula after total laryngectomy: systematic review of risk factors. Head Neck 37(11):1691–1697
Deniz M, Ciftci Z, Gultekin E (2015) Pharyngoesophageal suturing technique may decrease the incidence of pharyngocutaneous fistula following total laryngectomy. Surg Res Pract 2015:363640
Busoni M, Deganello A, Gallo O. (2015) Pharyngocutaneous fistula following total laryngectomy: analysis of risk factors, prognosis and treatment modalities. Acta Otorhinolaryngol Ital 35(6):400–405
Grau C, Johansen LV, Hansen HS, Andersen E, Godballe C, Andersen LJ et al (2003) Salvage laryngectomy and pharyngocutaneous fistulae after primary radiotherapy for head and neck cancer: a national survey from DAHANCA. Head Neck 25(9):711–716
Govaert JA, van Dijk WA, Fiocco M, Scheffer AC, Gietelink L, Wouters MW et al (2016) Nationwide Outcomes Measurement in Colorectal Cancer Surgery: Improving Quality and Reducing Costs. J Am Coll Surg 222(1):19–29.e2
Serbanescu-Kele CM, Halmos GB, Wedman J, van der Laan BF, Plaat BE (2015) Early feeding after total laryngectomy results in shorter hospital stay without increased risk of complications: a retrospective case-control study. Clin Otolaryngol 40:587–592
Aires FT, Dedivitis RA, Petrarolha SM, Bernardo WM, Cernea CR, Brandao LG (2015) Early oral feeding after total laryngectomy: a systematic review. Head neck 37(10):1532–1535
Suslu N, Sefik Hosal A (2016) Early oral feeding after total laryngectomy: Outcome of 602 patients in one cancer center. Auris Nasus Larynx 43(5):546–550
Dijs-Elsinga J, Marang-van de Mheen PJ, Smeets HJ, van der Made WJ, Vree R, Kievit J (2011) [Quality of care and operative complications: comparison of the results of 3 medical departments]. Nederlands tijdschrift voor geneeskunde 155:A1703
Cecatto SB, Soares MM, Henriques T, Monteiro E, Moura CI (2014) Predictive factors for the postlaryngectomy pharyngocutaneous fistula development: systematic review. Braz J Otorhinolaryngol 80(2):167–177
Sankar A, Johnson SR, Beattie WS, Tait G, Wijeysundera DN (2014) Reliability of the American Society of Anesthesiologists physical status scale in clinical practice. Br J Anaesth 113(3):424–432
Ferrier MB, Spuesens EB, Le Cessie S, Baatenburg de Jong RJ (2005) Comorbidity as a major risk factor for mortality and complications in head and neck surgery. Arch Otolaryngol Head Neck Surg 131(1):27–32
Erdag MA, Arslanoglu S, Onal K, Songu M, Tuylu AO (2013) Pharyngocutaneous fistula following total laryngectomy: multivariate analysis of risk factors. Eur Arch Otorhinolaryngol Head Neck Surg 270(1):173–179
Liang JW, Li ZD, Li SC, Fang FQ, Zhao YJ, Li YG (2015) Pharyngocutaneous fistula after total laryngectomy: a systematic review and meta-analysis of risk factors. Auris Nasus Larynx 42(5):353–359
Walton B, Vellucci J, Patel P, Jennings K, McCammon S, Underbrink MP (2017) Post-laryngectomy stricture and pharyngocutaneous fistula: review of techniques in primary pharyngeal reconstruction in laryngectomy. Clin Otolaryngol 1–8. https://doi.org/10.1111/coa.12905
Dias FL, Lima RA, Manfro G, Barbosa MM, Salviano S, Rocha RM et al (2009) Management of the N0 neck in moderately advanced squamous carcinoma of the larynx. Otolaryngol Head Neck Surg 141(1):59–65
Coskun HH, Medina JE, Robbins KT, Silver CE, Strojan P, Teymoortash A et al (2015) Current philosophy in the surgical management of neck metastases for head and neck squamous cell carcinoma. Head Neck 37(6):915–926
Hoofd-Halstumoren NW. Larynxcarcinoom (2010) Landelijke richtlijn, versie 3.0. VIKC, Utrecht
Pezier TF, Nixon IJ, Scotton W, Joshi A, Guerrero-Urbano T, Oakley R et al (2014) Should elective neck dissection be routinely performed in patients undergoing salvage total laryngectomy? J Laryngol Otol 128(3):279–283
Mattioli F, Bettini M, Molteni G, Piccinini A, Valoriani F, Gabriele S et al (2015) Analysis of risk factors for pharyngocutaneous fistula after total laryngectomy with particular focus on nutritional status. Acta Otorhinolaryngol Ital 35(4):243–248
Datema FR, Ferrier MB, van der Schroeff MP, Baatenburg de Jong RJ (2010) Impact of comorbidity on short-term mortality and overall survival of head and neck cancer patients. Head Neck 32(6):728–736
Dirven R, Swinson BD, Gao K, Clark JR (2009) The assessment of pharyngocutaneous fistula rate in patients treated primarily with definitive radiotherapy followed by salvage surgery of the larynx and hypopharynx. Laryngoscope 119(9):1691–1695
Sayles M, Grant DG (2014) Preventing pharyngo-cutaneous fistula in total laryngectomy: a systematic review and meta-analysis. Laryngoscope 124(5):1150–1163
Boyce SE, Meyers AD (1989) Oral feeding after total laryngectomy. Head Neck 11(3):269–273
Acknowledgements
The authors would like to acknowledge Jacqueline Timmermans, resident at VU medical center and Richard Dirven, fellow head and neck surgery at the Netherlands Cancer Institute for their support in clinical interpretation of the data.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
There was no specific funding for this study.
Conflict of interest
The Netherlands Cancer Institute receives a research grant from Atos Medical, Hörby, Sweden, which contributes to the existing infrastructure for health-related quality of life research of the Department of Head and Neck Oncology and Surgery. There are no other conflicts of interest to declare.
Research involving human participants and/or animals
This study does not fall under de scope of the Medical Research Involving Human Subjects Act, which was confirmed by the institutional review board (MREC 17.0439).
Informed consent
Not applicable.
Additional information
All authors of the paper are members of the Dutch Head and Neck Society. They cooperated in this study on behalf of this society.
Rights and permissions
About this article
Cite this article
Lansaat, L., van der Noort, V., Bernard, S.E. et al. Predictive factors for pharyngocutaneous fistulization after total laryngectomy: a Dutch Head and Neck Society audit. Eur Arch Otorhinolaryngol 275, 783–794 (2018). https://doi.org/10.1007/s00405-017-4861-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-017-4861-8