Abstract
Pharyngocutaneous fistula (PCF) is a common postoperative complication in patients undergoing laryngectomy. Many studies have focused on the predisposing factors and their treatment, but there is still controversy on how to identify high-risk patients.PCF is associated with delay in adjuvant treatment, prolonged hospital stay, and the requirement for additional surgical procedures. The increased incidence of post-laryngectomy PCF in the modern era of organ preservation therapy has driven considerable efforts to develop techniques to avoid and treat this complication. The study aims to analyze the incidence, predisposing factors, management, and outcome of PCF in post laryngectomy patients. We reviewed retrospectively the medical records of 72 patients who underwent total laryngectomy during the period from 2013 to 2022 at our institute. Details regarding age, gender, tumor site, comorbidities, radiotherapy, chemotherapy, duration of nasogastric tube feeding, the incidence of PCF and its management, and length of hospital stay. In our analysis of 72 patients, with 38 undergoing upfront laryngectomy and 34 salvage laryngectomy post-chemoradiation, we observed a 23% incidence of Pharyngocutaneous Fistula (PCF). Our univariate analysis revealed that low pre-op albumin levels and advanced stage significantly increased the risk of PCF. Specifically, PCF occurred in 16% of upfront laryngectomy patients and increased to 32% in salvage laryngectomy patients, though there was no significant association with pre-operative radiotherapy (RT).Among PCF cases, those from upfront laryngectomy had a mean onset time of 12 days, while salvage laryngectomy cases had a mean onset time of 8 days. The majority of PCF cases (64%) were managed conservatively, with 11% resolving through secondary suturing and 25% requiring surgical repair using local flaps. Notably, 80% of upfront laryngectomy PCF cases were managed conservatively, compared to 54% in salvage laryngectomy cases.The average hospitalization time for PCF patients was significantly longer at 35.6 days, compared to 12 days for non-PCF patients. Importantly, there were no fatal complications related to PCF in either group. Our study found that Pharyngocutaneous Fistula (PCF) occurs in both irradiated and non-irradiated patients, with T staging and pre-op albumin levels being significant risk factors. While PCF in non-irradiated patients can be treated conservatively, those in chemoradiation patients often require surgical intervention. Postoperative nutritional support like Feeding jejunostomy or Peg tube insertion aids in patient recovery from PCF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Pharyngocutaneous Fistula (PCF) is one of the most common complications after laryngectomy. Billroth performed the first laryngectomy in 1873, and soon after, he was the first surgeon to describe PCF [1]. Increased use of radiation as a primary treatment modality in laryngeal cancer has led to more salvage laryngectomies than upfront laryngectomies, resulting in an increased incidence of PCF. Apart from previous radiation, several risk factors can increase the incidence of PCF. Many studies have attempted to identify the risk factors for PCF to prevent it. However, the same risk factors have not consistently appeared significant in all studies. Thus, there is still controversy in identifying the risk factors and preventing the incidence of PCF. PCF leads to increased hospital stays, the need for additional surgical procedures, nutritional problems, and delays in starting adjuvant treatment. The mainstay of treatment for PCF is conservative management. However, some patients may require surgical intervention ranging from primary closure to flap cover.
Aim
This study aims to analyze the incidence, predisposing factors, management, and outcome of PCF in post-laryngectomy patients Table 1.
Methods
This is a retrospective study that included patients who underwent total laryngectomy for laryngeal cancer in the Department of Surgical Oncology, at a tertiary care center between 2013 and 2023. Patients who underwent any type of flap closure during laryngectomy were excluded from this study. From the cancer diary records, patient details were collected, including age, gender, site, co-morbidities, and stage, which was classified according to the latest TNM system. Preoperative hemoglobin and albumin levels, preoperative treatment details including emergency tracheostomy, radiotherapy, chemotherapy, details of the surgical procedure performed, and the incidence of PCF after surgery were also recorded. For patients who developed PCF, details regarding the postoperative day of PCF development, duration, length of hospital stay, treatment administered, and recovery were collected.
Statistical Analysis
Data analysis was conducted using MS Excel and SPSS 28.0 (Trial version). Frequencies, percentages, ranges, means, and standard deviations were calculated using this software. Chi-square tests, t-tests, and p-values were also calculated.
Results
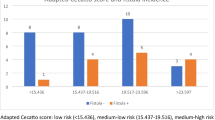
We analyzed 72 patients, among whom 65 were men (90.2%) and seven were women (9.8%), ranging in age from 30 to 79 years (mean 56; median 55). Out of 72 patients, 40 (56%) had glottic cancer, and 32 (44%) had supraglottic cancer. Among them, 38 patients underwent upfront laryngectomy, while 34 patients underwent salvage laryngectomy after chemoradiation. Regarding staging, 47 patients (65%) had T3 disease, and 25 (35%) had T4 disease. The mean preoperative serum albumin level was 3.73 g/dl (median 3.80; range 2.10–4.0). The mean preoperative hemoglobin value was 12.3 g/dl (median 12.0; range 4.8–16.9). Overall, 17 (23%) patients developed PCF. We analyzed various risk factors for the development of PCF.
On multivariate analysis, we found that among the analyzed risk factors, preoperative low albumin and advanced stage were associated with an increased incidence of PCF, which was statistically significant.
All PCF patients are initially managed conservatively with nil per oral, ryles tube feeding, and if necessary, percutaneous gastrostomy for feeding, along with antibiotics, anti-inflammatories, and daily dressing. If the PCF does not heal within 4 weeks, we proceed with surgical management.
Out of the 17 patients with PCF, 11 patients (64%) settled with conservative management. In two patients (11%), PCF resolved with secondary suturing, while in the remaining 4 patients, surgical repair was performed using local flaps. Two patients were treated with a pectoralis major myocutaneous flap, and two patients were treated with a deltopectoral flap.
Comparing the incidence of PCF in patients who underwent upfront laryngectomy and salvage laryngectomy, the incidence was 16% among patients who underwent upfront laryngectomy, while it increased to 32% for patients who underwent salvage total laryngectomy. Patients who underwent upfront laryngectomy showed a mean time of PCF formation of 12 (6–22) days, while for those who developed PCF after salvage laryngectomy, the mean time was 8 (2–20) days. Approximately 80% of patients with PCF after upfront laryngectomy settled with conservative management, whereas only 54% of patients with PCF after salvage laryngectomy settled with conservative management. The mean hospitalization time for fistula patients and non-fistula patients was 35.6 (19–90) days and 12 (10–22) days, respectively. There were no fistula-related fatal complications in either group.
Discussion
Pharyngocutaneous fistula (PCF) is one of the most common complications after total laryngectomy. The incidence of PCF following total laryngectomy in our study was 23%, consistent with earlier reports [2]. PCF represents an inconvenient and troublesome complication in the postoperative period. Prevention is crucial due to its association with prolonged hospitalization, additional procedures, complications, and delays in the start of adjuvant treatment [3]. Although numerous risk factors have been identified, some factors remain controversial, and some potential risk factors have not been thoroughly studied. We analyzed several risk factors for the development of pharyngocutaneous fistula in our patients.
Regarding the primary tumor site, patients with supraglottictumors may have a higher risk for PCF due to significant pharyngeal mucosa resections and resulting suture tension [4]. However, in our study, we found no significant association between the primary site and PCF incidence.
A meta-analysis by Wang et al. demonstrated a significant association between T-stage and PCF. Higher tumor stages with wider invasion, larger surgical resections, and less residual normal mucosa, high suture tension were associated with increased PCF incidence [4]. In our study, we also observed a significant association between T stage and PCF, with advanced stages showing a higher incidence.
Preoperative tracheostomy, often performed as an emergency procedure in patients with stridor due to high disease burden, was considered a potential risk factor for PCF in previous studies [5, 6], but we found no significant association in our study.
Organ preservation protocolis an important option in the treatment of advanced laryngeal cancer. Whether chemoradiation increases the chance of post-operative complications after salvage total laryngectomy has been analyzed in many studies. Many researchers have found that there is an increased incidence of PCF in salvage laryngectomy [7]. Radiation diminishes the healing capacity of the tissues due to a dysfunctional fibroblast population which results in hypovascularity and aggravation of atherosclerosis via induction of myo intimal fibrosis [8]. Some authors reported that there are no significant association [9]. In our study, there was an increase in incidence, early onset of PCF, and delayed healing with increased needfor surgical intervention in salvage laryngectomy. Though there was increased incidence there is no significant statistical association between PCF formation and pre-operative radiation.
A meta-analysis by Paydarfar et al. showed that, although preoperative radiotherapy represented a significant relative risk of PCF formation, there was also heterogeneity of effects among studies. Other radiotherapy-associated variables such as radiotherapy dose and the time frame between the end of radiation and surgery did not demonstrate an increased risk [10].
The median time between radiation and salvage laryngectomy in our study was 8 months slightly lower than the 10 months recorded by Grau et al. [11].While the meantime was 12.2 months, with a mean interval of 12.5 months (range of 3.5–19.4 months) in the group who developed PCF versus 18 months (range 4.2–24.0 months) in those who did not. This association was not statistically significant (p-0.92).
Diabetic mellitus patients are at higher risk of developing PCF due to impairment of wound healing, leukocyte dysfunction with increased susceptibility to infections [12], but in our study, there was no significant association between diabetic mellitus and the incidence of PCF.
Neck dissection with laryngectomy has been evaluated as a risk factor for the incidence of PCF in many studies [9]. In our study, there was no significant association between neck dissection and incidence of PCF.
A meta-analysis by Maohua Wang et al. showed that low pre-operative hemoglobin levels are a significant risk factor for the development of PCF [4]. In our study, there was no statistically significant association between low hemoglobin and the incidence of PCF.
It has been documented that hypoalbuminemia is associated with adverse surgical outcomes in head and neck cancers. Serum albumin is a marker of protein energy malnutrition and it is considered as a better indicator than anthropometry for nutrition status [13]. However, only few data exist for its association with complications after laryngectomy. Schwartz et al. found a significant relationship between low preoperative serum albumin and PCF afterlaryngectomy [14]. In our study, it was shown that a preoperative albumin level of less than 3 g/dl has a statistically significant increase in the incidence of PCF.
On the other hand, till now, there is no guideline for managing PCF. Fistula healing rates between 80 and 90% are commonly reported using conservative measures. In previously irradiated necks, spontaneous closure is less commonly achieved with rates as low as 44% being reported [15]. In our study about 80% of patients with PCF after upfront laryngectomy settled with conservative management. Only 54% of patients with PCF after salvage laryngectomy settled with conservative management The analysis of the literature shows a high variability of treatment approaches; there is no consensus about conservative treatment and waiting time, and neither about the indication for surgical treatment nor the ideal surgical technique.
Conservative management was done in most of the patients with PCF, conservative management includes NPO, ryles tube feeding, daily dressing, antibiotics analgesics.
The debate is how long to wait for spontaneous closure for PCF, In most of the studies this depends on the size of the defect, previous chemoradiation, and the need for adjuvant treatment.
In our study PCF without major wound breakdown and exposure of great vessels, we did conservative management for four weeks. In our study small fistula without radiation responds well to conservative management, but a larger fistula with previous radiation needed surgery often needed local flap reconstruction. It was found that percutaneous gastrostomy tube insertion was done in three patients, which helped in the early recovery and healing of PCF. As the number is less a statistical analysis could not be done.
Conclusion
Pharyngocutaneous Fistula (PCF) remains a challenging complication post-laryngectomy, adding considerable morbidity.Pre operativechemoradiation along with the stage of the disease and serum albumin levels appear to be significant factors in our study.Radiation added to more morbidity as conservative methods were failure.Development of computer based models with larger trials and preemptive reconstruction with vascularised flaps may be a solution.
References
Weir NF (1973) Theodore Billroth: the first laryngectomy for cancer. J Laryngol Otol 87(12):1161–1169
Markou KD, Vlachtsis KC, Nikolaou AC, Petridis DG, Kouloulas AI, Daniilidis IC (2004) Incidence and predisposing factors of pharyngocutaneous fistula formation after total laryngectomy. Is there a relationship with tumor recurrence? Eur Arch Oto-Rhino-Laryngol off J Eur Fed Oto-Rhino-LaryngolSoc EUFOS AffilGerSocOto-Rhino-Laryngol -. Head Neck Surg 261(2):61–67
Cavalot AL, Gervasio CF, Nazionale G, Albera R, Bussi M, Staffieri A et al (2000) Pharyngocutaneous fistula as a complication of total laryngectomy: review of the literature and analysis of case records. Otolaryngol–Head Neck Surg off J Am Acad Otolaryngol-Head Neck Surg 123(5):587–592
Wang M, Xun Y, Wang K, Lu L, Yu A, Guan B et al (2020) Risk factors of pharyngocutaneous fistula after total laryngectomy: a systematic review and meta-analysis. Head Neck Surg 277(2):585–599Eur Arch Oto-Rhino-Laryngol Off J Eur Fed Oto-Rhino-LaryngolSoc EUFOS AffilGerSocOto-Rhino-Laryngol -
Dedivitis RA, Ribeiro KCB, Castro MAF, Nascimento PC (2007) Pharyngocutaneous fistula following total laryngectomy.ActaOtorhinolaryngolItalOrganoUff. Della SocItalOtorinolaringol E ChirCerv-facc 27(1):2–5
Benson EM, Hirata RM, Thompson CB, Ha PK, Fakhry C, Saunders JR et al (2015) Pharyngocutaneous fistula after total laryngectomy: a single-institution experience, 2001–2012. Am J Otolaryngol 36(1):24–31
Sewnaik A, Keereweer S, Al-Mamgani A, Baatenburg de Jong RJ, Wieringa MH, Meeuwis CA et al (2012) High complication risk of salvage surgery after chemoradiation failures. ActaOtolaryngol (Stockh) 132(1):96–100
Sayles M, Grant DG (2014) Preventing pharyngo-cutaneous fistula in total laryngectomy: a systematic review and meta-analysis. Laryngoscope 124(5):1150–1163
Basheeth N, O’Leary G, Sheahan P (2014) Pharyngocutaneous fistula after salvage laryngectomy: impact of interval between radiotherapy and surgery, and performance of bilateral neck dissection. Head Neck 36(4):580–584
Paydarfar JA, Birkmeyer NJ (2006) Complications in head and neck surgery: a meta-analysis of postlaryngectomypharyngocutaneous fistula. Arch Otolaryngol Head Neck Surg 132(1):67–72
Grau C, Johansen LV, Hansen HS et al (2003) Salvage laryngectomy and pharyngocutaneousfistula after primary radiotherapy for head and neck cancer: a national survey from Dahanca. Head Neck 25(9):711–716
Boscolo-Rizzo P, De Cillis G, Marchiori C, Carpenè S, Da Mosto MC (2008) Multivariate analysis of risk factors for pharyngocutaneous fistula after total laryngectomy. Eur Arch Oto-Rhino-Laryngol off J Eur Fed Oto-Rhino-LaryngolSoc EUFOS AffilGerSocOto-Rhino-Laryngol -. Head Neck Surg 265(8):929–936
Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri SF (1999) Preoperative serum albumin level as a predictor of operative mortality and morbidity: results from the National VA Surgical Risk Study. Arch Surg 134:36–42
Schwartz SR, Yueh B, Maynard C, Daley J, Henderson W, Khuri SF (2004) Predictors of wound complications after laryngectomy: a study of over 2000 patients. Otolaryngol Head Neck Surg 131:61–68
Redaelli de Zinis LO, Ferrari L, Tomenzoli D, Premoli G, Parrinello G, Nicolai P (1999) Postlaryngectomypharyngocutaneous fistula: incidence, predisposing factors, and therapy. Head Neck 21(2):131–138
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shanmugam, S., Jebasingh, S.A. & Nagarajan, S. Incidence and Management of Pharyngo Cutaneous Fistula Following Total Laryngectomy - A Single Institutional 10 Years Experience. Indian J Otolaryngol Head Neck Surg (2024). https://doi.org/10.1007/s12070-024-04756-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12070-024-04756-y