Abstract
The objective is to investigate whether there is a correlation between the severity of typical brain lesions in congenital cytomegalovirus (cCMV) infection and cochlear implant (CI) outcome. The design of the study is a retrospective single-institutional chart review (2005–2015), performed in a tertiary academic referral center. 23 children with typical signs of cCMV infection on cerebral magnetic resonance imaging (MRI) and bilateral severe-to-profound sensorineural hearing loss were retrospectively evaluated. They were graded in three groups according to the severity of brain involvement. The average implantation age of the first CI is 1.8 years (range 0.6–5.8). Five patients were implanted unilaterally, 18 bilaterally. The average follow-up time after implantation was 3.3 years (range 0.6–6.9). Hearing performance was assessed using the Categories of Auditory Performance (CAP), and speech development was assessed using Speech Intelligibility Rating (SIR). The outcome in each group showed great variation. The majority of children achieved moderate-to-good auditory and speech rehabilitation. The children with severe MRI changes had comparatively better auditory than speech scores. There were children with good auditory performance (CAP ≥6) both in grades II and III, while poor performers (CAP ≤3) were encountered in each group. The severity of brain lesions on its own does not directly correlate with the outcome of cochlear implantation. Despite good retrospective diagnostic evidence of cCMV infection through MRI patterns, this has no predictive role for future hearing and speech rehabilitation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cytomegalovirus is a DNA virus that belongs to the family Herpesviridae and is the cause of the most common intrauterine virus infection. The affection of the fetus occurs transplacentally in preconceptionally seronegative as well as immune women. The earlier infections are acquired during intrauterine life, and the more severe are clinical manifestations [1,2,3]. In the first trimester of pregnancy, the transmission rate of CMV infection is low (35%) and rises to 73% in the third trimester [4].
About 90% of congenitally infected children are asymptomatic after birth. In the remaining, 10% symptoms are obvious at birth or manifest during childhood. Symptoms of the congenital CMV (cCMV) syndrome vary and comprise sensorineural hearing loss, chorioretinitis, hepatosplenomegaly, jaundice, anemia, purpura, thrombocytopenia, microcephaly, mental retardation, and combinations. While impairment of the reticuloendothelial system during infection is transient, damage to the central nervous system is irreversible [5]. Mental retardation and psychomotor disabilities may ensue depending on the severity of infection. Sensorineural hearing loss is the most common complication of cCMV infection and occurs in 10–15% of infected children [6]. Thus, CMV accounts for approximately 25% of all cases with neonatal nonhereditary hearing loss [7] and may progress postnatally in spite of high antibodies titers [6]. The benefit of cochlear implantation for hearing rehabilitation in patients with cCMV infection has already been proven in comparison with reference groups [8, 9].
Magnetic resonance imaging (MRI) plays a pivotal role in the decision-making process prior to cochlear implantation (CI). High-resolution MRI can rule out cochlear nerve aplasia, cochlear obliteration, congenital malformation as well as neurodevelopmental sequelae following cCMV infection. These range from ventricular dilatation, white matter gliosis, atrophy, parenchymal and ependymal cysts, or calcification to cortical malformations, especially polymicrogyria [1, 3].
It is unclear whether the extent of structural changes identified on MRI can serve as a prognostic marker concerning CI outcome. This study investigates a suspected correlation between the extent of lesions identified on MRI and both auditory performance and speech behavior in the post-implantation period in cases of cCMV infection.
Materials and methods
The retrospective study was carried out in a tertiary referral center. All children with sensorineural hearing loss in the period between 2005 and 2015, who underwent MRI and computed tomography (CT) prior to CI, were evaluated. 23 children with typical patterns according to van der Knaap et al. [10] of cCMV infection on cerebral magnetic resonance imaging (MRI) and bilateral severe-to-profound sensorineural hearing loss were retrospectively verified. cCMV infection was confirmed (by polymerase chain reaction test in serum/urine) in 17 of the 23 children; in the remaining six cases, it was strongly suspected. Hearing loss was diagnosed by means of an auditory brainstem response test under general anesthesia. Children with other etiologies of their sensorineural hearing loss were excluded.
Hearing rehabilitation was done according to a standardized protocol, using up-to-date programming strategies and intensive support through pediatric audiologists and language therapists. Categories of Auditory Performance (CAP) were used to rate the hearing outcome and Speech Intelligibility Rating (SIR) to evaluate speech development. CAP ranges from zero, for no awareness of environmental sounds, to nine, for use of a telephone with an unknown speaker in an unpredictable context [11]. SIR is scaled from one, for unintelligible connected speech (pre-recognisable words in spoken language), to five, for connected speech intelligible to all listeners (child is understood easily in everyday contexts) [12]. Both scores were determined at the same time for each individual.
During the study period, MRI protocols varied, but scanning included at least an axial T2-weighted flair sequence, an axial T2-weighted FSE, a sagittal T2-weighted FSE, an axial T1-weighted SE, and a 3D T2-weighted CISS sequence of the temporal bone. All exams were available for evaluation in a Patient Archiving and Communication System (PACS, GE, Milwaukee, USA).
Two neuroradiologists with extensive experience evaluated all imaging data for pathology of the brain on cranial MRI and of the temporal bone on CT. CMV manifestation is characterized either by migration disorders and/or by multifocal white matter lesions. The largest lesions are mostly found in the parietal area and predominantly involve deep white matter, sparing the immediate periventricular and subcortical white matter. According to the findings of van der Knaap et al. [10], the presence of abnormalities in the anterior part of the temporal lobe—including high signal abnormalities in the temporal white matter, cysts, and focal enlargement of the anterior part of the inferior horn—increases the likelihood that cCMV infection has taken place. All the white matter lesions were listed according to their anatomic localization (in frontal, parietal, occipital, or temporal). Lesion burden was graded as extensive, confluent, or only patchy. Findings, such as temporal involvement, additional ventriculomegaly, migration disorders, hippocampal atrophy, microcephaly, and cerebellar alterations, were noted.
To assess whether there is an association between cerebral MRI lesions in cCMV and the outcome of cochlear implantation, we defined three grades (groups) of MRI manifestations:
-
Grade I (mild): Few white matter abnormalities, defined as patchy lesions found either in up to three lobes, or, if found in all four lobes, lacking extensive or confluent spread. No neuronal migration disorder or microcephaly was present (Fig. 1a, b).
Fig. 1 Representative MRI patterns in each grade. Grade I parietal small subcortical and periventricular patchy T2-hyperintense areas (arrow) on axial (a, b) slices at temporal and parietal levels. Grade II multiple gross confluent patches subcortical, periventricular, and especially parietooccipital (arrows) on axial slices (c, d). Grade III polymicrogyria (arrows) on sagittal (e) and axial planes (f)
-
Grade II (moderate): Extended white matter abnormalities, defined as patchy white matter found in all four lobes: frontal, parietal, temporal, and occipital, and, in addition, extended or confluent white matter involvement in at least one lobe (mostly parietal) present; no additional migration disorders [10] (Fig. 1c, d).
-
Grade III (severe): Migration disorders as polymicrogyria and pachygyria or present heterotopias or a marked microcephaly, regardless of the extent of white matter involvement (Fig. 1e, f).
Finally, we compared the CAP and SIR results of the infants after CI between the aforementioned groups.
Results
All infants (n = 23) presented temporal lobe involvement according to van der Knaap et al. [10]. Eighteen of them had periventricular cysts, but only one was expressed ventriculomegally. In our series, cerebellar hypoplasia was not found. CT of the temporal bone displayed neither inner ear malformations nor obliteration.
The average implantation age at the time of the first CI is 1.8 years (range 0.6–5.8); group 1: 1.7 years, group 2: 1.4 years, and group 3: 2.8 years. The average implantation age at the time of the second CI is 2.2 years (range 0.6–5.8); group 1: 2 years, group 2: 2.1 years, and group 3: 2.6 years. Females outnumbered males 17–6. Five patients were implanted unilaterally [group 1 (n = 2), group 2 (n = 1), and group 3 (n = 2)] and 18 bilaterally. The average follow-up time after implantation was 3.3 years (range 0.6–6.9). The grading of MRI lesions placed 5 patients in the mildly involved group, 12 patients in the moderate group, and 6 patients in the severely affected group.
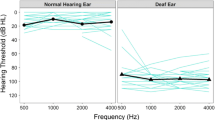
In most of the cases, hearing performance as well as speech development improved with the duration of follow-up (the post-implantation period). Despite differences in the severity of CMV infection, the majority of affected children achieved CAP scores ≥4 after a 2-year follow-up, representing discrimination of speech sounds and common phrases without lip reading (Fig. 2). Regarding speech development, most of the children developed intelligible speech for a concentrated listener (SIR ≥3) after a 2-year follow-up (Fig. 3).
The best performers are found in the group with moderate changes (grade II), but relatively poor performers (CAP ≤3) are found in every group. In most of the children with poor performance, other factors, such as bilingualism, late implantation, or additional handicaps, were present. Surprisingly, most children with mild MRI changes had lower auditory performance in comparison with the ones in grade II, and even to children from grade III, for a similar follow-up time. Three of the children with severe brain lesions, such as microcephaly and polymicrogyria, had lower CAP score than those from groups 1 and 2 with similar follow-up times. Children with severe MRI changes showed comparatively better auditory rehabilitation than speech rehabilitation, although none of them reached the full SIR score. The SIR results are mostly congruent with CAP for grades I and II, but discrepant for grade III.
Discussion
In the present study, we demonstrate that the outcome after cochlear implantation does not directly correlate solely with the degree of cerebral manifestations in MRI after cCMV.
In our cohort, all children except for patient 21 achieved satisfactory results overall in speech perception and production for the respective follow-up times. Neither does polymicrogyria prevent children from reaching average speech and hearing performance, nor do mild MRI findings guarantee an excellent outcome. According to our results, the benefit of CI implantation cannot be predicted solely based on the severity of MRI findings. To the best of our knowledge, no studies correlating CI outcome after cCMV infection with MRI lesions exist.
We present a group of 23 children with typical MR findings of CMV in relation to their CI outcome. Other studies that include children affected by cCMV infection report satisfactory to good hearing results after cochlear implantation. Yoshida et al. found satisfactory language perception in four cochlear-implanted children with cCMV infection [9]. Lee et al. reported good speech perception in 7 out of 11 children with unilateral implantation [8]. The average age at the time of implantation was 5.6 years. A comparison with our results is difficult to make, because their patients presented with progressive and post-lingual hearing loss, whereas ours had pre-lingual deafness. Ramirez et al. found no significant difference in linguistic outcome between children with SNHL due and not due to CMV infection. They underline the influence of manifold factors on outcome, most important multiple handicaps, and bilingual background [13].
Unilateral or bilateral implantation can also influence CAP and SIR results. Moreover, group 2 consists of twice as many children than the other two groups but has half as many unilateral implantations. However, compared to bilaterally implanted children in the same group, there were cases with both better and poorer auditory and speech performance. Another influential factor is age at the time of cochlear implantation. It is apparent that the average age at the time of cochlear implantation in group 3 is higher compared to the other two groups, not only for the first implantation, but also for the second one. One possible explanation is that these children often have other deficits which are initially in focus. Since Philips et al. [14] showed that early implantation of deaf children has a major positive impact on auditory and speech outcome, the later cochlear implantation in most of the children in group 3 is another unfavorable influential factor.
Pyman et al. reported that children with motor and cognitive delay are significantly slower to develop speech perception after CI compared with children without additional handicaps [15]. The outcome of the infants included in the current study is in line with this observation. A possible explanation for this fact is that psychomotor impairment may have a negative influence on compliance during rehabilitation.
Despite the low number of cases, it is obvious that some children from grade III achieved CAP and SIR results comparable to those from grade I despite severe MRI abnormalities. The fact that the most of the children with best CAP and SIR outcome are in group 2 could be explained by dividing the cases into subgroups according to the follow-up (≤3.6 and >3.6 years). Almost, half of the patients in group 2 had a long follow-up time, and thus more rehabilitation time and cochlear implant experience. Many of the children in each subgroup with less than 3.6-year post-implantation time have a better hearing outcome than speech development. This would be in line with the results of Ramirez et al. [13], who describe a better auditory perception than speech intelligibility in some children with CMV compared to a control group. They suspected central pathologies as a cause of the described discrepancy. Thus, severe brain lesions, such as those in group 3 as pathological sign of neurological and psychomotor deficiencies, are essential factors that influence the outcome of hearing and speech rehabilitation. Ciorba et al. also described lower language development overall of 16 infants affected by cCMV in comparison with an age-matched control group of patients with Connexin 26 mutation [16]. As speech intelligibility in children affected by cCMV varies widely after CI and progress may even be slower, [13] an intensive and specific rehabilitation is certainly of importance.
In the US, prenatal CMV infection is the leading cause of issue here, responsible for 15–20% of congenital deafness cases [17]. Fowler and Boppana reported hearing loss in 8.7% of children with asymptomatic infections and in 41% with symptomatic infections [18]. In most countries, there is no general screening for cCMV infection, neither in pregnant women nor in newborns. Because we are also confronted with this problem, we must rely on a retrospective diagnosis of cCMV infection by means of a polymerase chain reaction of preserved umbilical cord blood [19] or cranial MRI. Considering the fact that safe diagnosis through isolation of the virus is only possible during the first weeks of life, the number of cases of cCMV infection has surely been underestimated without established general screenings [20].
MRI findings in our patients are typical and coincide with current literature reports on white matter changes and migration pathologies found in CMV-infected children [2, 3, 10]. In our patients, the whole range of very specific findings, especially temporal lobe involvement as described by van der Knaap et al., was encountered. They diagnosed cCMV infection retrospectively using dried blood spots (Guthrie cards) in 87% of the children with temporal involvement [10]. In our study, 17 of 23 patients (73.9%) had confirmed CMV infection by polymerase chain reaction. Because all patients had temporal involvement in combination with sensorineural hearing loss, the probability of cCMV infection in the six cases with serologically unconfirmed diagnosis should be above 87%. Henneke et al. found MRI changes identical to those described for CMV infection in a rare RNASET2-deficient cystic leukoencephalopathy [21]. In the six cases clinically suspected but not serologically proven, it is possible that we included a child with such aetiology.
MRI findings of CMV-associated migration disorders have not been directly correlated with CI outcome. There are few data on migration disorders and cochlear implantation presented in case reports. Koren et al. [22] observed a child with schizencephaly and cortical dysplasia that benefitted from a cochlear implant. Epilepsy that developed years after implantation was not correlated with electrical stimulation by the implant. None of our patients with polymicrogyria have presented with seizures, neither before nor after CI. Smith et al. presented a child with Perisylvian syndrome implanted at the age of 32 months. Three months after implant activation, the child vocalized and responded to sounds; unfortunately, follow-up data from later on are not given [23]. Among our patients, a child (patient 23) with bilateral polymicrogyria (frontal and parietal, left more than right) and heterotopias was implanted sequentially and bilaterally at age 1.9 and 2.1 years, respectively. Seven-year post-implantation, he achieved a CAP of 8 and an SIR of 4. These few observations suggest that polymicrogyria and migration disorders in general do not prevent hearing rehabilitation by cochlear implantation, although perhaps in less than an average number of cases. Polymicrogyria has been correlated with clinical findings by Mavili et al. [24]. They found mental motor retardation in 89% of their 26 patients and speech problems in 84%. All their six patients with positive serological tests for CMV had bilateral involvement. In contrast, three of our five patients with polymicrogyria have unilateral involvement. Epilepsy was the major symptom encountered in six out of seven patients with unilateral polymicrogyria in the study by Mavili et al., while none of our patients has yet presented with epilepsy. However, our three patients with unilateral polymicorgyria were, on average, 6 years at time of last observation, while Mavili et al. describe the epilepsy in their patients with unilateral polymicrogyria as late onset.
Limitations of the current study are the small number of patients in each group as well as their disproportionate distribution and the varying follow-up.
Conclusion
Auditory performance and speech intelligibility after CI in children affected by cCMV infection are determined by multiple factors and do not solely correlate with the severity of cerebral MRI lesions. Intensive rehabilitation support should be guaranteed, because a discrepancy between hearing and speech outcome is likely. Despite good retrospective diagnostic evidence of cCMV infection through characteristic MRI patterns, the severity alone of these lesions has no predictive role for future rehabilitation results.
References
Barkovich AJ, Girard N (2003) Fetal brain infections. Child’s Nerv Syst 19(7–8):501–507. doi:10.1007/s00381-003-0763-8
Barkovich AJ, Lindan CE (1994) Congenital cytomegalovirus infection of the brain: imaging analysis and embryologic considerations. AJNR Am J Neuroradiol 15(4):703–715
van der Knaap MS, Valk J (2005) Congenital and perinatal cytomegalovirus infection. In: Magnetic resonance of myelination and myelin disorders. Springer, Berlin, Heidelberg, pp 645–657. doi:10.1007/3-540-27660-2_85
Bodeus M, Kabamba-Mukadi B, Zech F, Hubinont C, Bernard P, Goubau P (2010) Human cytomegalovirus in utero transmission: follow-up of 524 maternal seroconversions. J Clin Virol 47(2):201–202. doi:10.1016/j.jcv.2009.11.009
Cheeran MC, Lokensgard JR, Schleiss MR (2009) Neuropathogenesis of congenital cytomegalovirus infection: disease mechanisms and prospects for intervention. Clin Microbiol Rev 22(1):99–126. doi:10.1128/CMR.00023-08 (table of contents)
Ross SA, Fowler KB, Ashrith G, Stagno S, Britt WJ, Pass RF, Boppana SB (2006) Hearing loss in children with congenital cytomegalovirus infection born to mothers with preexisting immunity. J Pediatr 148(3):332–336. doi:10.1016/j.jpeds.2005.09.003
Morton CC, Nance WE (2006) Newborn hearing screening—a silent revolution. N Engl J Med 354(20):2151–2164. doi:10.1056/NEJMra050700
Lee DJ, Lustig L, Sampson M, Chinnici J, Niparko JK (2005) Effects of cytomegalovirus (CMV) related deafness on pediatric cochlear implant outcomes. Otolaryngol-Head Neck Surg 133(6):900–905. doi:10.1016/j.otohns.2005.08.013
Yoshida H, Kanda Y, Takahashi H, Miyamoto I, Yamamoto T, Kumagami H (2009) Cochlear implantation in children with congenital cytomegalovirus infection. Otol Neurotol 30(6):725–730. doi:10.1097/MAO.0b013e3181b1212e
van der Knaap MS, Vermeulen G, Barkhof F, Hart AA, Loeber JG, Weel JF (2004) Pattern of white matter abnormalities at MR imaging: use of polymerase chain reaction testing of Guthrie cards to link pattern with congenital cytomegalovirus infection. Radiology 230(2):529–536. doi:10.1148/radiol.2302021459
Archbold S, Lutman ME, Marshall DH (1995) Categories of auditory performance. Ann Otol Rhinol Laryngol Suppl 166:312–314
Allen MC, Nikolopoulos TP, O’Donoghue GM (1998) Speech intelligibility in children after cochlear implantation. Am J Otol 19(6):742–746
Ramirez Inscoe JM, Nikolopoulos TP (2004) Cochlear implantation in children deafened by cytomegalovirus: speech perception and speech intelligibility outcomes. Otol Neurotol 25(4):479–482
Philips B, Corthals P, De Raeve L, D’Haenens W, Maes L, Bockstael A, Keppler H, Swinnen F, De Vel E, Vinck B, Dhooge I (2009) Impact of newborn hearing screening: comparing outcomes in pediatric cochlear implant users. Laryngoscope 119(5):974–979. doi:10.1002/lary.20188
Pyman B, Blamey P, Lacy P, Clark G, Dowell R (2000) The development of speech perception in children using cochlear implants: effects of etiologic factors and delayed milestones. Am J Otol 21(1):57–61
Ciorba A, Bovo R, Trevisi P, Bianchini C, Arboretti R, Martini A (2009) Rehabilitation and outcome of severe profound deafness in a group of 16 infants affected by congenital cytomegalovirus infection. Eur Arch Otorhinolaryngol 266(10):1539–1546. doi:10.1007/s00405-009-0944-5
Grosse SD, Ross DS, Dollard SC (2008) Congenital cytomegalovirus (CMV) infection as a cause of permanent bilateral hearing loss: a quantitative assessment. J Clin Virol 41(2):57–62. doi:10.1016/j.jcv.2007.09.004
Fowler KB, Boppana SB (2006) Congenital cytomegalovirus (CMV) infection and hearing deficit. J Clin Virol 35(2):226–231. doi:10.1016/j.jcv.2005.09.016
Ogawa H, Baba Y, Suzutani T, Inoue N, Fukushima E, Omori K (2006) Congenital cytomegalovirus infection diagnosed by polymerase chain reaction with the use of preserved umbilical cord in sensorineural hearing loss children. Laryngoscope 116(11):1991–1994. doi:10.1097/01.mlg.0000237633.28017.62
Gross M, Finckh-Kramer U, Spormann-Lagodzinski M (2000) Congenital hearing disorders in children. 1: Acquired hearing disorders. Hno 48(12):879–886
Henneke M, Diekmann S, Ohlenbusch A, Kaiser J, Engelbrecht V, Kohlschutter A, Kratzner R, Madruga-Garrido M, Mayer M, Opitz L, Rodriguez D, Ruschendorf F, Schumacher J, Thiele H, Thoms S, Steinfeld R, Nurnberg P, Gartner J (2009) RNASET2-deficient cystic leukoencephalopathy resembles congenital cytomegalovirus brain infection. Nat Genet 41(7):773–775. doi:10.1038/ng.398
Koren L, Shpak T, Duchman H, Luntz M (2007) Case report: cochlear implant in a child with schizencephaly and cortical dysplasia. Cochlear Implant Int 8(4):200–202. doi:10.1179/cim.2007.8.4.200
Smith W, Axon P (2007) Cochlear implantation in a patient with Perisylvian syndrome. Cochlear Implant Int 8(2):117–121. doi:10.1179/cim.2007.8.2.117
Mavili E, Coskun A, Per H, Donmez H, Kumandas S, Yikilmaz A (2012) Polymicrogyria: correlation of magnetic resonance imaging and clinical findings. Child’s Nerv Syst 28(6):905–909. doi:10.1007/s00381-012-1703-2
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by our institutional ethic committee (Number: 3363-2016) and is in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Research involving human participants, approved by our institutional ethic committee (3363-2016).
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lyutenski, S., Götz, F., Giourgas, A. et al. Does severity of cerebral MRI lesions in congenital CMV infection correlates with the outcome of cochlear implantation?. Eur Arch Otorhinolaryngol 274, 1397–1403 (2017). https://doi.org/10.1007/s00405-016-4408-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4408-4