Abstract
To validate a wrist-worn portable device (WatchPat 200) to diagnose OSA in an Asian cohort. To evaluate its cost-effectiveness. Twenty patients with suspected OSA were recruited and had simultaneous polysomnography (PSG) and WatchPAT assessments concurrently within the hospital’s sleep laboratory. The study population consisted of 18 male and 2 female patients, whose mean age was 39 (±16) years, mean BMI was 27.2 (±5.5) kg/m2, mean Epworth Sleepiness score was 8.55 (±4.8). The correlation between the AHI was assessed using Spearman’s correlation coefficient and agreement was tested via the Bland Altman plot. Sensitivities and specificities were then applied to the various AHI groups. Spearman’s coefficient was 0.94, which suggested that a very strong correlation between the AHI recorded by the WatchPat and the PSG. Bland–Altman plot showed good agreement with the AHI mean difference of about 4.23 with a slight tendency to overscore the AHI at the mild range of OSA and underscore the range at the severe end of OSA. The WatchPat showed 100% sensitivity when compared to PSG for mild OSA and is thus a good screening test for the undiagnosed general population. Furthermore, it also showed 100% specificity when compared to PSG for severe OSA suggesting that it is a good diagnostic test for people with a high suspicion of OSA. This facilitates a timelier diagnosis and a more economical approach with potential cost savings of up to $900 per patient.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnoea (OSA) is a highly prevalent clinical problem—the Wisconsin Sleep Cohort Study estimated a prevalence of 24% among men and 9% among women in that state [1]. The metabolic syndrome, a cluster of cardiovascular risk factors, is associated with obstructive sleep apnoea. Obstructive sleep apnoea has been shown to be an independent risk factor for hypertension and insulin resistance [2]. Hence, screening for sleep apnea and then treating it are is indeed an important aspect of public health.
The current standard for clinical practice, established through evidence-based reviews by the American Academy of Sleep Medicine (AASM), is to confirm the diagnosis of obstructive sleep apnoea (OSA) with in-laboratory polysomnography (PSG) [3].
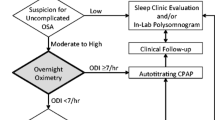
However, PSG is cumbersome, complex, and an expensive technique. In 2007, the Portable Monitoring Task force of the American Academy of Sleep Medicine published Clinical guidelines for the use of unattended portable monitors in the diagnosis of sleep apnoea. In countries like Israel, up to 70% of OSA currently is diagnosed via the use of unattended portable monitors.
The Watch-Pat200 is a six-channel unattended ambulatory device (level 3) that measures the pulse volume of the finger continuously. It is based on the peripheral arterial tone (PAT) signal with three additional channels: heart rate (derived from the PAT signal), pulse oximetry, and actigraphy. The PAT measures the arterial pulsatile volume changes of the finger that are regulated by the alpha-adrenergic innervation of the smooth muscles of the vasculature of the finger, and thus reflects sympathetic nervous system activity. The Watch-Pat200 indirectly detects apnoea/hypopnoea events by identifying surges of sympathetic activation associated with the termination of these events. This information is further combined with heart rate and pulse oximetry data that are analyzed by the automatic algorithm of the system [4]. The Watch-Pat 200 is a slightly smaller device than its predecessor, and it also includes body position leads to monitor for body position. This study aimed to validate the Watch-Pat 200 for the diagnosis of sleep apnoea via the apnoea–hypopnoea index (AHI) as well as to take note of other parameters as well as the total sleep time and the sleep efficiency.
Materials and methods
Twenty subjects with suspected OSA, consisting of eighteen males and two females, were recruited from the period of August 2011–December 2011. All subjects completed a comprehensive sleep and health survey that included an Epworth Sleepiness Scale [5]. All were simultaneously monitored with full overnight PSG and portable monitoring using Watch-Pat200 in the public hospital sleep laboratory in Singapore. Individuals who were medically unstable, using home oxygen therapy, or using alpha-adrenergic receptor blocking agents were not eligible to participate.
Polysomnography (PSG)
All subjects underwent a laboratory-based level 1 PSG evaluation. PSG records included: electrooculogram (EOG), four-channel electroencephalogram, electrocardiogram (ECG), submental and tibial electromyogram (EMG), oronasal airflow, thoracic and abdominal movement, arterial oxygen saturation and snoring intensity. All PSG records were scored using the American Academy of Sleep Medicine (AASM) criteria [6]. In particular, an apnoea was scored if there was a drop in the peak signal excursion by 90% or more for at least 10 s. A hypopnoea was scored if airflow was reduced by at least 30% accompanied with oxygen desaturation of 3% or an arousal. The AHI was defined as the number of apnoeas and hypopnoeas per hour of total sleep time. The PSG was considered unacceptable for data analysis if any of the following rejection criteria occurred: (1) PSG total sleep time less than 1.5 h, and (2) poor quality PSG recording (defined as a substantial portion of the PSG not being interpretable to score sleep and respiratory events).
WatchPat200
All subjects simultaneously underwent in-hospital portable monitoring using the WatchPat200. The device is worn around the wrist. Two finger probes extend from the main body. One detects the PAT signal. The other measures arterial oxygen saturation. The main body contains an actigraph that detects limb activity. The device continuously recorded five physiologic signals through the night: PAT, oxygen saturation, heart rate, actigraphy, and body position. Data were analyzed with an automatic computerized algorithm. A respiratory event was scored if one of the three criteria were met: (1) 30% or greater reduction in PAT amplitude together with a pulse rate acceleration of 10%; (2) 30% or greater reduction in PAT amplitude together with a 3% oxyhemoglobin desaturation; or (3) 4% oxyhemoglobin desaturation [4, 7, 8]. The WatchPat was considered unacceptable for data analysis if any of the following rejection criteria occurred: (1) WatchPat valid sleep time less than 1.5 h, and (2) all WatchPat channels not available for review and analysis [9].
Statistical analysis
Sleep studies were considered acceptable for data analysis if none of the following rejection criteria occurred: (1) PSG total sleep time less than 4 h; (2) WatchPat valid sleep time less than 4 h; (3) poor quality PSG recording (defined as a substantial portion of the PSG being not able to score sleep and respiratory events); and (4) all WatchPat channels not available for review and automatic analysis [9].
Given that the subjects were not normally distributed-judging by the small number of 20 participants and the values of the results, the following statistical tests were used. The Wilcoxon signed rank test was applied to evaluate if the AHI differed significantly between the PSG and the Watch-PAT200. Following that the correlation between the AHI was assessed using Spearman’s correlation coefficient and Bland—Altman plots to test for agreement [10]. These were also applied to the total sleep time and the sleep efficiency. The tests were conducted via the Stata v10.1 done by an independent statistician-based in the public hospital.
Results
The study population consisted of 18 males and 2 females, mean age of 39 ± 16 years, range (18–70). Mean body mass index was 27.2 ± 5.5 kg/m2 range (20–38) and Epworth Sleepiness score was 8.55 ± 4.8. The mean AHI by the PSG was 31.30 ± 23.81, while the mean AHI for the Watch-Pat200 was 27.07 ± 21.47 (Table 1). The Wilcoxon signed rank test showed a significant difference between the AHI PSG and the AHI Watch-Pat200 (adjusted variance = 716.25, P = 0.0094).
Spearman’s coefficient was 0.94 (P < 0.0001), which suggests a very strong correlation between the AHI recorded by the Watch-Pat200 and the PSG. Bland–Altman plot showed an AHI mean difference of about 4.23 with a slight tendency for the Watch-Pat200 to overscore the AHI at the mild range of OSA and to underscore the range at the severe end of OSA (Fig. 1).
With regard to the total sleep time recorded, the mean total sleep time for the PSG recorded was 376 min, while the mean Watch-Pat200 total sleep time was 412.65 min (Table 1). Spearman’s coefficient was 0.6228 (P < 0.0034) which suggests a moderately strong correlation between the two variables. Bland–Altman plot showed a mean difference between of 36.55 min with most scores within ±40 min of this difference (Fig. 2).
The sleep studies of all the 20 participants did not fulfill the rejection criteria and were hence accepted for analysis.
Using AHI thresholds values of more than 5 to diagnose OSA and 30 for severe obstructive sleep apnoea, the WatchPat showed 100% sensitivity when compared to PSG for mild OSA (Table 2) and is thus a good screening test for the undiagnosed general population. Furthermore, it also showed 100% specificity when compared to PSG for severe OSA (Table 2) suggesting that it is a good diagnostic test for people with a high suspicion of obstructive sleep apnoea.
The total sleep time had a moderately strong correlation according to Spearman’s correlation. Of note, all 20 participants had more than 4 h of sleep, which is the targeted amount of time to validate the sleep study. The agreement between Watch-Pat200 and PSG is about +10 to −70 min for most parts. It also showed that in general Watch-Pat200 tended to under record the total sleep time in comparison to the PSG.
Discussion
This study showed that the WP200 is a simple, reliable and accurate device for ambulatory diagnosis of OSA. It detects sympathetic vasoconstriction of digital vascular beds to detect obstructive airway events, in contrast with the expensive and complex measurements of flow and thoracic and abdominal movements used in the PSG. The Bland–Altman plot showed a good agreement in diagnosing OSA. There were a few values that differed by more than 10, but there would not have affected their diagnosis of severe OSA.
We found that the in-laboratory AHI WP200 results were significantly correlated with the in-laboratory PSG results, consistent with several studies. Ayas et al. [7] found in 30 patients a good correlation between the AHI measured by the Watch-PAT100 and the AHI measured by the PSG (Pearson’s coefficient = 0.87, P < 0.001). Pillar et al. [11] also showed significant correlation between the WatchPAT100 AHI and PSG AHI in 68 patients (r = 0.87, P < 0.001). Li et al. [8] found a high correlation between Watch-PAT200 AHI and PSG AHI (Pearson’s coefficient, r = 0.92, P < 0.001). Schnall et al. [12] found a significant correlation between apnoea–hypopnoea events detected in standard PSG and vasoconstriction episodes detected in PAT. O’Donnell et al. [13] showed that in patients with OSA, the degree of induced upper airway obstruction directly correlates with the degree of PAT attenuation.
This study showed a slight tendency for the Watch-Pat200 to overscore the AHI at the mild range of OSA and to underscore the range at the severe end of OSA. Results are different from previous studies [4], which showed a tendency to underscore AHI at the mild range of OSA and overscore at the severe range of AHI. On the contrary, it is consistent with the study by Li et al. [8] that showed overestimation of PAT in the lower range of AHI and underestimation of PAT in the higher range of AHI. Li et al. [8] suggested that PAT overestimated events when the AHI was in the lower range because the Watch-Pat200 detected events that were missed by the standard scoring criteria [7]. Another explanation might be related to sleep fragmentation other than those induced by apnoeas.
Our present study showed sensitivities and specificities for Watch-Pat200 AHI scores greater than 5 and greater than 30 to be 100/75, and 80/100, respectively. Silva et al. [14] similarly showed 100% sensitivity for the use of Watch-Pat200 to diagnose OSA with AHI threshold of 5 in a study population of 20 patients. Li et al. [8] showed that in a study population of 28 participants, the sensitivities and specificities for Watch-Pat200 AHI thresholds of 5 and 30 to be 95.8/100, and 85.7/100, respectively. The high sensitivity of the WatchPat indicates that it is a good screening test for the undiagnosed general population. The high specificity indicates that it is a good diagnostic test for individuals with a high suspicion of OSA.
In terms of financial costs, Watch-Pat200 costs about $300, whereas a privately done PSG study would cost about $1200 and a subsidize PSG study will cost about $700 dollars. Hence, there are significant savings using the Watchpat. Using the 2007 AASM guidelines for portable monitors and using the ESS screening test of 9 or more as significant. Out of 20 patients in our study, 10 patients had an ESS of 9. Of the 10, none had serious comorbidities, but 1 had parasomnias. Excluding that 1 patient, there will be 9 who will have been first subjected to the Watchpat. Of the 9, 7 would have been diagnosed with OSA. This could have led to potential savings of $6300 (Fig. 3).
Furthermore, the waiting time for PSG study is currently at least 3 months in our institution whereas the Watchpat can be organized in the same week, leading to a much earlier diagnosis and starting CPAP earlier. In addition, as a screening test, Watch-Pat200 can be done in the home setting and will not have the first night effect.
There were several limitations to this study. First, although the Watch-Pat200 is designed to be used in a home setting, we evaluated it in a hospital based setting. However, previous studies like Pittman et al. [9] have shown that Watch-Pat100 had good agreement when done at home compared to the in house PSG.
Second, the population cohort in this study is relatively small. However, we compensated for this using the statistical analysis tools that assumed that the scores were not normally distributed, hence allowing some compensation.
Third, Watch-Pat200 like its predecessor is notably unable to differentiate central sleep apnoea from obstructive sleep apnoea. It should be noted that the population we studied did not include the population with central apnoea. However, given the very low prevalence of central sleep apnoea among the referred population to diagnostic sleep laboratories, we do not consider this to be a major disadvantage.
Conclusion
In a population of patients with suspected OSA, the Watch-Pat200 similar to its predecessor can quantify an AHI that compares favorably with the gold standard PSG for the diagnosis of obstructive sleep apnoea. The WatchPat showed 100% sensitivity when compared to PSG for mild OSA and is thus a good screening test for the undiagnosed general population. Furthermore, it also showed 100% specificity when compared to PSG for severe OSA suggesting that it is a good diagnostic test for people with a high suspicion of OSA. This facilitates a timelier diagnosis and a more economical approach with potential cost savings of up to $900 dollars per patient.
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle aged adults. N Engl J Med 328:1230–1235
Sharma SK, Agrawal S, Damodaran D et al (2011) CPAP for the metabolic syndrome in patients with obstructive sleep apnea. N Engl J Med 365:2277–2286
Portable Monitoring Task Force of the American Academy of Sleep Medicine (2007) Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnoea. J Clin Sleep Med 3:737–747
Bar A, Pillar G, Dvir I et al (2003) Evaluation of a portable device based on peripheral arterial tone for unatended home sleep studies. Chest 123:695–703
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Berry R, Budhiraja R, Gottlieb DJ et al (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. J Clin Sleep Med 88:597–619
Ayas NT, Pittman S, MacDonald M, White DP (2003) Assessment of a wrist-worn device in the detection of obstructive sleep apnea. Sleep Med 4:435–442
Li W, Wang R, Huang D, Liu X, Jin W, Yang S (2013) Assessment of a portable monitoring device WatchPAT 200 in the diagnosis of obstructive sleep apnea. Eur Arch Otorhinolaryngol 270:3099–4015
Pittman SD, Ayas NT, Macdonald MM et al (2004) using a wrist-worn device based on peripheral arterial tonometry to diagnose obstructive sleep apnoea. Sleep 27:923–933
Chan YH (2003) Biostatistics 104: correlational Analysis. Singapore Med J 44:614–619
Pillar G, Bar A, Betito M et al (2003) Assessment of a wrist-worn device in the detection of obstructive sleep apnea. Sleep Med 4:207–212
Schnall RP, Shlitner A, Sheffy J, Kedar R, Lavie P (1999) Periodic, profound peripheral vasoconstriction—a new marker of obstructive sleep apnea. Sleep 22:939–946
O’Donnell CP, Allan L, Atkinson P, Schwartz AR (2002) The effect of upper airway obstruction and arousal on peripheral arterial tonometry in obstructive sleep apnea. Am J Respir Crit Care Med 166:965–971
Silva E, Balieiro FO, Xavier SD et al (2013) Comparative analysis of diagnostic methods in obstructive sleep apnea syndrome: polysomnography and use Watch Pat 200. Otolaryngol Head Neck Surg 149:267–270
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was conducted in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was taken from all participants prior to conduct of the study. The disposables for the Watch-Pat 200 were provided by Easmed. No Grant funding was undertaken. The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Rights and permissions
About this article
Cite this article
Gan, Y.J., Lim, L. & Chong, Y.K. Validation study of WatchPat 200 for diagnosis of OSA in an Asian cohort. Eur Arch Otorhinolaryngol 274, 1741–1745 (2017). https://doi.org/10.1007/s00405-016-4351-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-016-4351-4