Abstract
Obstructive sleep apnoea syndrome (OSAS) is associated with inflammatory processes and elevated plasma cytokines. This study assesses the effect of surgery in cytokine levels of OSAS patients. A total of 24 male patients with mild to moderate OSAS, confirmed with polysomnography underwent septoplasty and uvulo-palato-pharyngoplasty in a period of a year. Control group consisted of 12 overweighted subjects and 15 obese subjects. Peripheral venous blood was collected from each patient 1 week before surgical treatment and 6 months postoperatively. Spontaneous production of tumour necrosis factor (TNF-a) by monocytes and serum levels of IL-1β and IL-6 were investigated. Control subjects were also examined for the same pro-inflammatory cytokines. Production of TNF-a and IL-6 were significantly elevated in OSAS patients and obese controls compared with overweighted control subjects (p < 0.05). Serum levels of IL-1β did not differ among the study groups. Preoperative cytokine values were significantly correlated with the preoperative body mass index (BMI) and the apnoea/hypopnoea index (AHI) in OSAS patients. Surgery resulted a significant reduction in the TNF-a and IL-6 values of the study group. Decrease in cytokine level was strongly correlated with the AHI decrease. The postoperative relative percentage change of IL-6 values was significantly higher than this of TNF-a (p < 0.001). Surgical management of mild to moderate OSAS leads to a significant reduction in TNF-a and IL-6 values. Our data indicate that AHI is an independent risk factor of systemic inflammation; however it affects cytokines to a lesser degree compared with the BMI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnoea syndrome (OSAS), characterized by cessation of air flow for a minimum of 10 s despite continuous respiratory effort, is a prevalent condition in our society. Recent studies demonstrate that OSAS is associated with increased cardiovascular morbidity and mortality [1, 2]. These co-morbidities are even consistently found in patients with mild OSAS [3, 4]. Hypoxia causes oxidative stress and may be involved in inflammatory processes resulting elevated pro-inflammatory cytokine levels. Cytokines such as IL-1, IL-6 and TNF-a, have an important role in sleep regulation [5, 6] and some of them have been found to be increased in patients with OSAS [5, 7]. Although there is a strong link between sleep apnoea and cardiovascular morbidities such as atherosclerosis, the underlying mechanisms of this relation are not clarified yet.
Studies of OSAS patients treated with nasal continuous positive airway pressure (nCPAP) showed a reduction of the IL-6 and TNF-a concentrations and decrease of cardiovascular mortality [7, 8].
However, the efficacy of surgical treatment of OSAS patients in cytokine levels has not been extensively assessed. The purpose of the study is to evaluate the influence of surgery in pro-inflammatory cytokine levels in correlation with the body mass index (BMI) and the apnoea-hypopnoea index (AHI) changes in the long term.
Materials and methods
A total of 24 male OSAS-patients (mean age 45.1, range 26–54 years) diagnosed with polysonmography were evaluated in this study. The study group was divided into two subgroups according to their BMI. Specifically, the first subgroup included 13 obese patients (mean BMI 33.4 ± 1.5) and a second subgroup included 11 overweighted patients (mean BMI 26.1 ± 1.1). The control group consisted of 12 overweighted subjects (mean BMI 27.4 ± 0.8) and 15 obese control subjects (mean BMI 34.9 ± 1.8) of similar age and sex distribution with the study group. Polysomnography confirmed the absence of OSAS in all subjects of the control group and BMI was used to identify obese subjects among control and OSAS group. Specifically a BMI value ≥30 means obesity and a value between 25 and 29.9 indicates overweight. Exclusion criteria of OSAS patients were prior surgery for OSAS, chronic inflammation (e.g. chronic tonsillitis), systemic disease and acute infection within the previous 2 weeks. None of the patients had been under steroidal, anti-inflammatory, sympatheticomimetic or sympatheticolitic medications in the course of this study. Patients over 55 years old were also excluded from the study to avoid any potential age effects on the plasma cytokines [9]. The study was approved by the Ethics Committee of Aristotle University, Medical School, and all the patients signed informed consent after detailed description of the study.
At the baseline visit, all the patients underwent detailed ear, nose and throat examination and flexible endoscopy in which Mueller’s maneuver was performed. All the patients had an at least two-level airway obstruction with significant septal deviation causing nasal congestion symptoms and prolonged soft palate (Mallampati III to IV) with significant oropharyngeal obstruction during Mueller’s maneuver. The clinical assessment was followed by a polysomnographic evaluation (Compu Medic, Abbotsford, Australia) of one night with at least 8 h of sleep in the sleep laboratory. Electrocardiography, electrooculography and electromyography recordings were obtained with surface electrodes according to standard methods [10]. Nasal and mouth airflow were measured with thermistors. Ventilatory movements of chest and abdomen were also monitored.
The diagnosis of OSAS was based on the AHI results. AHI was calculated as the total number of episodes of apnoea and hypopnoea per hour of sleep. Specifically an AHI >5 was diagnostic of OSAS. An AHI ≥5 to <20 indicated a mild OSAS, ≥20 to <30 indicated moderate OSAS and ≥30 indicated severe OSAS. The OSAS group consisted of patients with mild to moderate OSAS with a mean AHI of 23.2 ± 3.6 without significant difference between weight subgroups. The control group had a mean AHI of 3.5 ± 0.4. All AHI values of the study subgroups are presented in Table 1.
Surgical management included a two-level procedure including the nose and the palate: septoplasty and uvulo-palato-pharyngoplasty (UPPP) in one stage. Key steps of UPPP included bilateral tonsillectomy, partial resection of the anterior pillar of the soft palate, sutures between posterior and anterior pillar with the posterior pillar pulled forwards away from the posterior pharyngeal wall, closure of the tonsillar fossa, and maximized lateralization of the posterior pillar, partial removal of the uvula greater than 1.5 cm, to reduce the uvula to approximately 1 cm.
Postoperative complications included a primary bleeding from the uvula controlled with cauterization in operating theatre. Two more patients had excessive pain resulting poor feeding. Oral morphine solution was given in cases of excessive pain with immediate improvement of food intake. One patient presented a transient palatal insufficiency with complete recovery within a month. In a follow-up appointment 6 months postoperatively a second polysomnography performed.
Peripheral venous blood was collected from each patient at 8 o' clock in the morning, 1 week preoperatively and 6 months postoperatively. Blood samples were stored at −72°C until assay. Serum IL-1β and IL-6 were measured by ELISA (R & D Systems, Minneapolis, MN, USA). Peripheral blood mononuclear cells were isolated with a Ficoll-Hypaque gradient. Monocytes (1 × 105/ml) were cultured for 24 h and counted. TNF-a measured with an enzyme linked immunosorbent assay kit.
Results were analyzed using SPSS version 12.0 for Windows (SPSS Inc., Chicago, IL, USA). Descriptive statistics are presented within the body of the text as mean values ± standard deviation (SD). The alpha level was set at 0.05. The significance of differences within groups was analyzed with a Student paired t test and the significance of differences between groups was performed by analysis of variance first followed by t tests with Bonferroni correction. Correlation analysis between cytokines and AHI or BMI was based on Spearman rank correlation. The impact of the possible contributing factor of cytokine serum levels such as BMI and AHI was assessed with a multiple regression analysis with serum level of cytokine as dependent variables.
Results
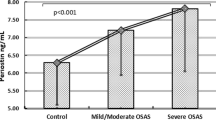
The TNF-a from monocytes and serum IL-6 concentrations were significantly increased in OSAS-patients (63.8 ± 22.2 and 0.21 ± 0.08 pg/ml respectively) compared with the control group (115.4 ± 23.7 pg/ml, p = 0.032 and 0.64 ± 0.09 pg/ml and p < 0.001 respectively). No difference was found regarding the IL-1β values between the two study groups. Further analysis of cytokine results after division of the two groups in subgroups of obese and overweighted subjects showed that obese subjects had significantly elevated TNF-a and IL-6 cytokines compared with overweighted subjects in both groups. Obese—OSAS patients had the higher values of the above cytokines followed by the obese control subjects, overweighted OSAS patients and the lower values found in overweighted control subjects (Table 1). Interestingly the obese control subjects presented slightly higher values than overweighted OSAS patients, but this difference was not significant (p = 0.07).
Spearman correlation analysis showed a positive correlation between cytokine plasma levels and variables like BMI and AHI (Table 2). Multiple regression analysis showed that the strongest predictor of TNF-a production in mild to moderate OSAS was the BMI (p = 0.005) followed by AHI (p = 0.022). Similarly IL-6 serum level had as independent predictors first the BMI (p = 0.003) followed by AHI (p = 0.011).
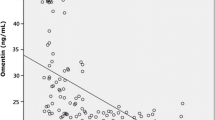
Postoperatively the AHI was significantly improved in 20 patients, however 4 patients presented slight or no improvement. The mean preoperative value presented a significant reduction from a mean of 23.2 ± 3.6 to a mean of 9.8 ± 1.5 (p = 0.004). Postoperatively TNF-a and IL-6 values were also significantly reduced in the study group (Fig. 1a, b), however IL-1β values did not significantly differed from the preoperative results. The relative percentage change of AHI after surgical treatment was correlated with the relative percentage changes in TNF-a and IL-6 levels (r = 0.56, p = 0.044 and r = 0.67, p = 0.021, respectively). The mean of BMI did not differed significantly postoperatively. A change in BMI was noted only in four patients and this number does not allow correlation analysis. However, their improvement in cytokine levels was higher than the mean percentage change of the patients without BMI change. Comparison between TNF-a and IL-6 relative percentage change revealed a more significant reduction for IL-6 values (p < 0.001) (Fig. 2).
Discussion
Considering that a significant percentage of the general population (2% for females and 4% for males) suffers from OSAS [11] and that levels of TNF-a and IL-6 are increased in OSAS patients; it is necessary to assess whether a surgical treatment of OSA affects the blood levels of the above cytokines.
Our study confirmed the fact that TNF-a and IL-6 levels are significantly higher in patients with mild to moderate OSAS than in healthy overweighted subjects. However, OSAS overweighted patients appeared to have similar cytokine levels in comparison with obese control subjects. These results suggest that both OSAS and obesity increase cytokine level acting as independent factors and TNF-a and IL-6 levels are affected in mild OSAS equally by obesity and hypoxia. Limitations on this conclusion are that we did not assess patients with severe OSAS and that our sample size is considerably small.
Other authors suggest that in patients with severe OSAS, TNF-a serum level was mainly affected by the severity of hypoxia during sleep rather than the BMI [7]. It is possible that elevation of cytokine level is accelerated from mild to severe OSAS with hypoxia being the predominant factor only in patients with severe disease.
The OSAS treatment remains controversial. Although the clinical efficacy of nCPAP is widely accepted, its compliance is actually much lower for patients with mild disease than patients with severe disease [3]. It is important to note that in patients who discontinued the nCPAP-therapy symptoms recurred [1, 12]. Moreover nCPAP-therapy is the cause of other morbidities especially in nasal functions [13, 14]. Surgical management in patients with mild to moderate OSAS and marked anatomical structures causing airway obstruction still has a place. This is supported by studies suggesting surgical treatment as a sensible alternative to nCPAP therapy [15–17]. For some patients surgical improvement of nasal respiratory passage or pharyngeal walls collapse increases nCPAP tolerance. Thus the assessment of surgical treatment of OSAS in a cytokine level is useful as surgery usually offers permanent results.
Postoperative results in our study showed a significant reduction of the TNF-a and IL-6 values after surgical intervention in OSAS-patients. This was accompanied by a significantly decreased AHI postoperatively. In addition we found a strong correlation between AHI changes and cytokine plasma level changes. The reduction of the TNF-a and IL-6 values as a result of improvement of sleep parameters is already suggested by other authors [7, 8]. Moreover an opposite interaction is reported where pharmaceutically decreased cytokine levels result improvement of sleep parameters [18]. Kataoka et al. [19], showed a significant TNF-a reduction 1 week after UPPP, tonsillectomy and adenoidectomy in OSAS-patients, results which are in agreement with our study. However this study presented short term results and did not correlated cytokine changes with the BMI. In our study the reduction of TNF-a and IL-6 values seem to be permanent as our assessment was 6 months after surgical treatment. BMI decrease in the early postoperative period after UPPP can be related with painful food intake. This is the reason why cytokine level immediately after surgery cannot predict the long term result as often BMI reaches the preoperative values in a period of a few months. This is in agreement with our study as only four patients presented significant BMI decrease postoperatively. However, their cytokine values presented a remarkable decrease and this fact indicates a positive effect of weight loss in postoperative cytokine level. In any case obesity has a significant role in the regulation of plasma cytokine level and it should always be included in the assessment of any OSAS treatment modality.
It is important to note that both TNF-a and IL-6 cytokines presented similar behaviour pre- and post-surgery a fact which indicates a common triggering factor, and probably an interaction as shown in a study in which a neutralizing factor of TNF-a resulted a reduction of the IL-6 values [18].
The fact that IL-6 values showed a higher relative improvement compared with the changes in TNF-a values is an indication that IL-6 seems to respond better in surgical management of OSAS.
Based on the findings of this study, we can suggest that surgical management of mild to moderate OSAS is indicated for the reduction of pro-inflammatory cytokines, which are related to cardiovascular complications of the disease.
References
He J, Kryger MH, Zorick FJ, Conway W, Roth T (1998) Mortality and apnoea index in obstructive sleep apnea. Experience in 385 male patients. Chest 94:9–14
Lavie L (2003) Obstructive sleep apnoea syndrome—an oxidative stress disorder. Sleep Med Rev 7:35–51
Sahlman J, Pukkila M, Seppä J, Tuomilehto H (2007) Evolution of mild obstructive sleep apnoea after different treatments. Laryngoscope 117:1107–1111
Woodson BT, Garancis JC, Toohill RJ (1991) Histopathologic changes in snoring and obstructive sleep apnea syndrome. Laryngoscope 101:1318–1322
Vgontzas AN, Papanicolaou DA, Bixler EO (1997) Elevation of plasma cytokines in disorders of excessive daytime sleepiness: role of sleep disturbance and obesity. J Clin Endocrinol Metab 82:1313–1316
Krüger JM, Obal F Jr, Fang J, Kubota T, Taishi P (2001) The role of cytokines in physiological sleep regulation. Ann N Y Acad Sci 933:211–221
Minoguchi K, Tazaki T, Yokoe T, Minoguchi H, Watanabe Y, Yamamoto M, Adachi M (2004) Elevated production of tumor necrosis factor-a by monocytes in patients with obstructive sleep apnoea syndrome. Chest 126:1473–1479
Yokoe T, Minoguchi K, Matsuo H, Oda N, Minoguchi H, Yoshino G, Hirano T, Adachi M (2003) Elevated levels of C-reactive protein and interleukin-6 in patients with obstructive sleep apnea syndrome are decreased by nasal continuous positive airway pressure. Circulation 107:1129–1134
Daynes RA, Araneo BA, Ershler WB, Maloney C, Li G, Ryu S (1993) Altered regulation of IL-6 production with normal aging: possible linkage to the age-associated decline in dehydroepiandrosterone and its sulphated derivative. J Immunol 150:5219–5230
Rechtshaffen A, Kales A (1986) A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. NIH Publication No. 204. US Government Printing Office, Washington
Deegan PC, McNicholas WT (1996) Predictive value of clinical features for the obstructive sleep apnoea syndrome. Eur Respir J 9:117–124
Partinen M, Jamieson A, Guilleminault C (1988) Long-term outcome for obstructive sleep apnoea syndrome patients. Mortality. Chest 94:1200–1204
Jenkison C, Davies RJO, Mullins R, Stradling JR (1999) Comparison of therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised prospective parallel trial. Lancet 353:2100–2105
Constantinidis J, Knöbber D, Steinhart H, Kuhn J, Iro H (2000) Fine-structural investigations of the effect of nCPAP-mask application on the nasal mucosa. Acta Otolaryngol 120:432–437
Sundaram S, Bridgman SA, Lim J, Lasserson TJ (2005) Surgery for obstructive sleep apnoea. Cochrane Database Syst Rev 11(4):106, CD001004
Sher AE, Schechtman KB, Piccirillo JF (1996) The efficiency of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 19:156–177
Friedman M, Lin HC, Gurpinar B, Joseph NJ (2007) Minimally invasive single-stage multilevel treatment for obstructive sleep apnea/hypopnea syndrome. Laryngoscope 117:1859–1863
Vgontzas AN, Zoumakis E, Lin HM, Bixler EO, Tragada G, Chrousos GP (2004) Marked decrease in sleepiness in patients with sleep apnea by etanercept, a tumor necrosis factor-a antagonist. J Clin Endocrinol Metab 89:4409–4413
Kataoka T, Enomoto F, Kim R, Yokoi R, Fujimori M, Sakai Y, Ando I, Ichikawa G, Ikeda K (2004) The effect of surgical treatment of obstructive sleep apnea syndrome on the plasma TNF-a levels. Tohoku J Exp Med 204:267–272
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Constantinidis, J., Ereliadis, S., Angouridakis, N. et al. Cytokine changes after surgical treatment of obstructive sleep apnoea syndrome. Eur Arch Otorhinolaryngol 265, 1275–1279 (2008). https://doi.org/10.1007/s00405-008-0627-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-008-0627-7