Abstract
Retroglossal obstruction is one of the etiologies causing obstructive sleep apnea (OSA) and can be addressed by removing some tissues of the tongue base. However, because of its deep-seated location, its surgical removal is still challenging. Although coblation technique has been introduced, its efficacy and morbidity need further evaluation, particularly in Asians. This study aimed to assess its safety and effectiveness and to identify outcome prognosticators. Forty-seven OSA patients who underwent coblation lingual tonsil removal were included. Retroglossal obstruction was confirmed by drug-induced sleep videofluoroscopy. Attended full-night polysomnography was performed twice; before and 6 months after surgery in 27 patients. The tongue base was fully exposed with three deep-seated traction sutures, visualized with a 30° or 70° endoscope, and ablated using a coblator. Surgical success was defined with postoperative apnea hypopnea index (AHI) <20 and reduction >50 %. Postoperative morbidities were evaluated. Demographic and polysomnographic parameters between success and failure groups were compared. None of the patients had immediate postoperative hemorrhage. Postoperatively, one patient had delayed hemorrhage and one patient severe respiratory difficulty. Taste loss, tongue dysmotility, dental injury or severe oropharyngeal stricture were absent. A mean AHI decreased from 37.7 ± 18.6 to 18.7 ± 14.8/h (P < 0.001). The success rate was 55.6 %. Their mean minimal oxygen saturation was significantly lower (P = 0.004) in the failure group. Coblation lingual tonsil removal technique showed minimal morbidity and favorable outcome in Koreans. The surgical outcome might be associated with the severity of single respiratory events.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The tongue base is frequently involved in upper airway obstruction in patients with obstructive sleep apnea (OSA). Various methods have been introduced to enlarge retroglossal airway space. Non-surgical treatment such as continuous positive airway pressure therapy and mandibular advancement splints can be advantageous as they are non-invasive. However, patients who are not compliant to the devices will need surgical treatment. Surgical techniques can be divided into two types: (1) enlargement of bony framework such as genioglossus advancement, maxillomandibular advancement and hyoid suspension; and (2) volume reduction such as midline glossectomy [1, 2], submucosal lingual excision [3] and transoral robotic tongue base resection [4]. Recently, endoscopic coblation of the tongue base including the lingual tonsils was introduced [5–7]. However, more studies showing the efficacy and morbidities of coblation technique are needed, particularly in Asians who generally have smaller bony framework than the Caucasians. The aim of the present study was to describe the endoscopic coblation lingual tonsil removal technique, to evaluate its effectiveness and morbidities and to identify its prognosticators for successful treatment.
Patients and methods
Study samples and localization of obstruction site
The present study included patients who underwent endoscopic coblation lingual tonsil removal consecutively due to OSA at Seoul National University Bundang Hospital from 2009 through 2013. Their medical records were reviewed retrospectively. All of the patients underwent attended in-lab full-night polysomnography (PSG). The inclusion criteria were as follows: (1) older than 18 years of age; (2) apnea hypopnea index (AHI) equal to 5/h or more; and (3) involvement of the tongue base in upper airway obstruction. The retroglossal obstruction was determined by preoperative midazolam-induced sleep videofluoroscopy as previously described [8]. This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital.
Surgical technique and postoperative management
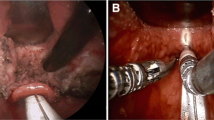
Under general anesthesia via a nasotracheal tube, lingual tonsil ablation was performed using Coblator EVAC70 (Arthrocare ENT, Sunnyvale, CA). All of the patients underwent operation from a single surgeon. The mouth was kept open during surgery by employing a dental mouth gag between the maxillary and mandibular molars on the left side of the mouth. The tongue was taken out of the mouth by making three traction sutures at the level of circumvallate papillae to expose the tongue base (Fig. 1). The tongue base could be fully visualized by administering a 30 or 70° rigid endoscope. The operation was conducted on the right side of patients as in endoscopic sinus surgeries. The operative field was bordered by the circumvallate papillae anteriorly, epiglottis posteriorly and tonsillar fossa laterally on either side. Surgical removal included most of the lingual tonsils and submucosal glands of the tongue base. Ablation proceeded from the circumvallate papillae down to the epiglottis. Its central part was ablated first until muscular tissues of the tongue base were identified, and then its lateral part was ablated leaving several millimeters of intact mucosa on both sides to prevent formation of oropharyngeal stricture (Fig. 2). Most of the patients were transferred to the intensive care unit (ICU) immediately after surgery and the nasotracheal intubation was maintained overnight to avoid airway obstruction. The endotracheal tube was removed in the next morning and the patients were discharged from the hospital 2–3 days after the surgery.
Coblation lingual tonsil resection. The tongue base is visualized using a 30° endoscope (top left). Surgery begins in the midline (top middle) and a deep central furrow is made by coblation (top right). Thereafter, right (bottom left) and left lateral sides of the lingual tonsils are coblated (bottom middle), leaving several millimeters of intact mucosa at far lateral region to prevent postoperative oropharyngeal stricture (bottom right)
Evaluation of morbidity and surgical outcomes
Postoperative hemorrhage was divided into immediate (≤24 h after surgery) and delayed (>24 h after surgery). Dental injury, respiratory difficulty and abnormality of tongue movement were evaluated while in the hospital. Taste loss, severe oropharyngeal stricture causing difficulty in swallowing or respiration and re-hypertrophy of the lingual tonsils were assessed at 6 months.
Attended in-lab full-night PSG was recommended postoperatively 6 months after surgery. Success of surgery was determined using the criteria of postoperative AHI less than 20 with reduction more than 50 % [9]. To determine prognosticators for successful treatment, patients were divided into success or failure groups.
Statistical analysis
All continuous data were presented as means ± standard deviations. A nonparametric paired test was performed to compare continuous variables between before and after surgery using the Wilcox on signed rank test. Comparisons between the success and failure groups were performed using the Mann-Whitney test for continuous variables and Chi-square test for discrete variables. Statistical analyses were performed using SPSS 18.0 software (SPSS Inc, Chicago, IL). P < 0.05 was considered statistically significant.
Results
A total of 47 patients (40 men and 7 women) underwent endoscopic coblation lingual tonsil removal. All but one of the patients had never undergone any form of upper airway surgery. Their mean age was 40.9 ± 11.4 years and mean body mass index (BMI) was 26.5 ± 3.9 kg/m2.
Morbidities
During surgery, rescue diathermy cauterization was not necessary. None of the patients experienced immediate postoperative hemorrhage. One patient (1/47, 2.1 %) revisited an emergency center due to delayed hemorrhage 19 days after surgery. The bleeding site was observed at the upper part of the tongue base. Under general anesthesia, the bleeding point was visualized with three traction sutures as in the lingual tonsil ablation surgery. Hemostasis was performed by bipolar diathermy cauterization. One patient (1/47, 2.1 %) complained of severe respiratory difficulty postoperatively soon after she was directly transferred to her ward. Because the respiratory distress did not resolve with high flow mask oxygen, she was re-intubated and transferred to the ICU. None of the patients had dental injury or abnormality of tongue mobility. Re-hypertrophy of the lingual tonsils was not observed (Fig. 3). None of the patients had loss of taste or oropharyngeal stricture causing swallowing or respiratory difficulties.
Surgical outcomes
Twenty-seven (24 men and 3 women)of the 47 patients underwent both pre- and postoperative PSG and their mean age was 42.4 ± 10.7 years and mean BMI was 27.5 ± 3.6 kg/m2. The other 20 patients had only preoperative PSG due to refusal of postoperative examination or loss of follow-up. However, there were no significant differences between the patients with postoperative PSG and ones without postoperative PSG in age, sex, preoperative AHI.
Most of the 27 patients with postoperative PSG underwent concomitant surgeries at the same time such as tonsillectomy (n = 24), uvulopalatopharyngoplasty (n = 24), septoturbinoplasty (n = 8) and genioglossus advancement (n = 4). There was a significant difference between their mean preoperative (37.7 ± 18.6/h) and postoperative AHI (18.7 ± 14.8/h) (P < 0.001) (Fig. 4). The improvement rate (AHI reduction >50 %) was 66.7 % (18/27). The success rate (AHI reduction >50 % and postoperative AHI <20/h) was 55.6 % (15/27). The mean oxygen desaturation index (ODI) also significantly decreased from 31.7 ± 20.7/h to 14.7 ± 13.1/h (P = 0.001) and the mean minimal oxygen saturation significantly increased from 78.0 ± 9.1 to 83.1 ± 6.4 % (P = 0.001) after surgery.
Prognostic factors
The success group included 15 patients (12 men and 3 women) and the failure group included 12 patients (12 men and no woman). The mean minimal oxygen saturation was significantly lower in the failure group (72.4 ± 9.4 %) than in the success group (82.9 ± 5.4 %) (P = 0.004). Although the mean AHI, AI and ODI were higher in the failure group, there was no statistical significance (Table 1).
Discussion
Because the tongue base is a deep-seated structure in the oropharynx, it is challenging not only to visualize the region, but also to remove the hypertrophic tongue base. Several studies [1–3] described different techniques for tongue base resection including lingual tonsillectomy. The procedures are often associated with intra- or postoperative complications such as bleeding, respiratory difficulty, swallowing difficulty, dental injury and taste change. Robinson et al. [10]. First presented coblation technique, which allows a submucosal minimally invasive tongue base resection. However, because they used suspension laryngoscopy, there were some limitations in terms of direct and clear visualization of the tongue base. Recently, endoscopic coblation of the tongue base was introduced [5–7]. However, these studies were about only introduction or safety evaluation of the surgical procedure. Studies to investigate its morbidity, efficacy and prognosticators are not sufficient. Although a study also assessed the effectiveness of coblation of tongue base on the basis of PSG results [11], they excised only midline tissue of the tongue base. In another study investigating the safety and surgical outcomes of Z-palatopharyngoplasty combined with endoscopic coblator open tongue base resection [12], patients with severe OSA (AHI greater than 30/h) were enrolled. However, prognosticator for successful outcome was not evaluated. In particular, there have been a very few studies performed in Asians. Because the Asians have smaller bony maxillomandibular framework than the Caucasians, the surgical result of the soft tissue resection in the upper airway should be independently evaluated in Asians.
As transoral minimally invasive surgery is becoming the preferred choice, endoscopic approach can be more beneficial in many ways. In this study, we were able to maximally expose the surgical field and visualize the tongue base without compression of the tongue and risk of dental injury. The simple three traction sutures provided a wider range of motion for surgical devices than a single stay suture [5–7]. It is well known that the coblator has working temperature in the range of only 40–70 °C [6]. Therefore, thermal injury associated with the coblator is less severe compared to bovie or laser surgeries. This endoscopic coblation technique can also be used for patients with small mouth opening. However, this technique also has its own limitations. As coblation involves ablation of hypertrophic tissues and is not a surgical plane-wise dissection, it may be more difficult to identify the surgical plane and to evaluate the exact amount of tissues removed during surgery. Therefore, there may be a risk to make an injury to the important underlying neurovascular structures. In addition, contraction of the underlying muscles which is induced by coblation may hinder the operation.
Recently, transoral robotic surgery was introduced to address surgical difficulties of the tongue base [4, 13] and the efficacy of the surgery has been shown in several studies. A study of transoral robotic surgery performed along with other concomitant upper airway procedures in 20 patients showed a significant decrease of AHI from 36.3 to 16.4/h [13]. In another recent study of 12 patients who underwent only transoral robotic surgery of the tongue base, AHI decreased from 43.9 to 17.6/h (response rate of 50 %) [4]. These results are almost comparable to those of multilevel surgeries [14] and superior to those of uvulopalatopharyngoplasty alone [8, 9]. The outcome in the present study was also comparable to those of the robotic surgeries or other multilevel surgeries. Robotic surgery may be superior in terms of exposure and resection but its use may be hindered by some drawbacks such as: (1) high medical cost; (2) longer setup time; (3) longer compression time of the tongue; (4) use of bovie spatula with higher working temperature; (5) suction which is operated by an assistant and not the surgeon and (6) need for sufficient mouth opening.
It still remains a challenge for otolaryngologists to predict which patients will have a successful result postoperatively. In the present study, we found that BMI and AHI were not significant factors associated with surgical outcome. Interestingly, minimal oxygen saturation was the only finding to differentiate the success group from the failure group. The reason why more severe oxygen desaturation is a determining factor for surgical failure may not be clearly explainable. This might be related to the severity of single respiratory events because minimal oxygen desaturation may be more severe when the patients have single more severe respiratory distress events regardless of the frequency of the respiratory events. It has been shown that patients with excessive daytime sleepiness had longer mean duration of apnea events and lower minimal oxygen saturation compared to patients with similar AHI but no excessive daytime sleepiness [15], which supports longer and deeper events may have more severe physiological consequences. There was a proposal of an “obstruction severity” parameter, which was defined as a sum of apneas followed by a desaturation within the next 60 s, to estimate the severity of OSA [16]. Patients with similar AHI showed a significant difference in the values of the “obstruction severity” parameter and mortality of patients with higher values of the parameter was found to be elevated. They suggested the importance of the duration and morphology of breathing cessation and oxygen desaturation.
The present study had some limitations. Firstly, lingual tonsil removal surgery was not performed as a single procedure. However, in that the outcome was superior to our previous stand-alone uvulopalatopharyngoplasty series, coblation lingual tonsil removal could be interpreted to result in favorable outcome. Furthermore, the morbidity of coblation lingual tonsil surgery was demonstrated in our study. Secondly, we included a small number of patients. However, because there have been a very few studies on the surgical outcome of endoscopic coblation lingual tonsil removal and, in particular, there were few studies performed in Asians, our study may be appreciable as a preliminary study.
In conclusion, the retroglossal obstruction in patients with OSA was treated with coblation-assisted removal of the lingual tonsils, showing minimal morbidity and favorable outcome in the present study. The surgical outcome might be associated with the severity of single respiratory events. Further studies including randomized controlled trials are required to prove its validity in a larger number of patients.
References
Suh GD (2013) Evaluation of open midline glossectomy in the multilevel surgical management of obstructive sleep apnea syndrome. Otolaryngol Head Neck Surg 148:166–171
Fujita S, Woodson BT, Clark JL, Wittig R (1991) Laser midline glossectomy as a treatment for obstructive sleep apnea. Laryngoscope 101:805–809
Friedman M, Soans R, Gurpinar B, Lin HC, Joseph N (2008) Evaluation of submucosal minimally invasive lingual excision technique for treatment of obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg 139:378–384 discussion 385
Lin HS, Rowley JA, Badr MS et al (2013) Transoral robotic surgery for treatment of obstructive sleep apnea-hypopnea syndrome. Laryngoscope 123:1811–1816
Bock JM, Trask DK (2008) Coblation-assisted lingual tonsillectomy for dysphagia secondary to tongue base hypertrophy. Ann Otol Rhinol Laryngol 117:506–509
Rotenberg B, Tan S (2011) Endoscopic-assisted radiofrequency lingual tonsillectomy. Laryngoscope 121:994–996
Leitzbach SU, Bodlaj R, Maurer JT, Hormann K, Stuck BA (2014) Safety of cold ablation (coblation) in the treatment of tonsillar hypertrophy of the tongue base. Eur Arch Otorhinolaryngol 271:1635–1639
Lee CH, Hong SL, Rhee CS, Kim SW, Kim JW (2012) Analysis of upper airway obstruction by sleep videofluoroscopy in obstructive sleep apnea: a large population-based study. Laryngoscope 122:237–241
Sher AE, Schechtman KB, Piccirillo JF (1996) The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 19:156–177
Robinson S, Ettema SL, Brusky L, Woodson BT (2006) Lingual tonsillectomy using bipolar radiofrequency plasma excision. Otolaryngol Head Neck Surg 134:328–330
Babademez MA, Ciftci B, Acar B et al (2010) Low-temperature bipolar radiofrequency ablation (coblation) of the tongue base for supine-position-associated obstructive sleep apnea. ORLJ Otorhinolaryngol Relat Spec 72:51–55
Lin HC, Friedman M, Chang HW, Yalamanchali S (2014) Z-palatopharyngoplasty combined with endoscopic coblator open tongue base resection for severe obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg 150:1078–1085
Vicini C, Dallan I, Canzi P et al (2012) Transoral robotic surgery of the tongue base in obstructive sleep apnea-hypopnea syndrome: anatomic considerations and clinical experience. Head Neck 34:15–22
Lin HC, Friedman M, Chang HW, Gurpinar B (2008) The efficacy of multilevel surgery of the upper airway in adults with obstructive sleep apnea/hypopnea syndrome. Laryngoscope 118:902–908
Mediano O, Barcelo A, de la Pena M, Gozal D, Agusti A, Barbe F (2007) Daytime sleepiness and polysomnographic variables in sleep apnoea patients. Eur Respir J 30:110–113
Kulkas A, Tiihonen P, Julkunen P, Mervaala E, Toyras J (2013) Novel parameters indicate significant differences in severity of obstructive sleep apnea with patients having similar apnea-hypopnea index. Med Biol Eng Comput 51:697–708
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wee, J.H., Tan, K., Lee, WH. et al. Evaluation of coblation lingual tonsil removal technique for obstructive sleep apnea in Asians: preliminary results of surgical morbidity and prognosticators. Eur Arch Otorhinolaryngol 272, 2327–2333 (2015). https://doi.org/10.1007/s00405-014-3330-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3330-x