Abstract
Cephalic resection of the lateral crura of the alar cartilages, lateral osteotomies, and removal of the nasal hump during rhinoplasty may cause collapse of the internal nasal valve angle. This study was performed to compare preventive effects of two techniques (spreader grafts and flaring sutures) on rhinoplasty by rhinomanometry. Two hundred and forty-eight patients participated in this semi-experimental study. The patients were assigned into two groups. 28 of them were not available for follow-up. All patients had a straight nose in the midline and no severe septal deviations. 87 of 220 patients underwent the spreader grafts technique and the flaring sutures technique was performed in 133 patients. The nasal airway resistance was calculated by active anterior rhinomanometry on admission to hospital and again between 3 and 6 months following surgery. The mean of follow-up was 20.9 ± 2.9 weeks. After rhinoplasty, nasal airway resistance decreased in 46 patients (52.9 percent) of spreader grafts group and in 84 patients (63.2 percent) of flaring sutures group. The median nasal airway resistance difference (before–after surgery) of spreader grafts and flaring sutures groups was 0.027 Pa/ml/s (range −110 to 130) and 0.017 Pa/ml/s (range −0.690 to 0.790), respectively. The difference of nasal airway resistance between before and after rhinoplasty in two groups was insignificance (Mann–Whitney U test, P = 0.5). The spreader grafts and flaring sutures move the dorsal border of the upper lateral cartilage in a lateral direction and had similar preventive effect on nasal airway resistance after rhinoplasty.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
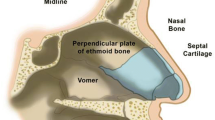
A humpy nose is among the main reasons for rhinoplasty. It can be inherited or posttraumatic and the skeletal framework of the hump may contain cartilaginous or bony components. The middle third of the nose consists of the paired upper lateral cartilages, the dorsal part of the septum, and the scroll of the upper lateral cartilages upon the lower lateral cartilages. This area plays an important role in the nasal valve function. The internal nasal valve is defined as the area between the caudal end of the upper lateral cartilages and the cartilaginous septum. This angle is normally 10°–15° in the white (leptorrhine) nose and is more obtuse in African American and Asian (platyrrhine) noses [1]. Anatomical distortion of this area during rhinoplasty by cephalic resection of the lateral crura of the alar cartilages, as well as lateral osteotomies, can weaken the physiological support of the upper lateral cartilages; this results in the medialization of these tissues. In addition, removal of the nasal hump during rhinoplasty may distort the junction of the upper lateral cartilages and the septum, causing collapse of the internal nasal valve angle. Nasal valve collapse is related to deficiencies in the structural support of the lateral nasal wall. Surgeons should be aware not to overzealously remove nasal tissues and ensure that the nasal valve angle is not compromised during the surgical procedure. This can significantly complicate functional and esthetic results after rhinoplasty [2]. This problem can occur after resection of a cartilaginous-bony hump with paramedian and lateral osteotomies for closing the “open roof”. It is maintained that the resection of just 2 mm of cartilaginous vault during resection of the hump is sufficient to weaken the junction of the septum and the upper lateral cartilages, thus making the latter more liable to inferomedial collapse [3].
Collapse of the ULC after dorsal hump reduction in rhinoplasty can be repaired with spreader grafts, flare or suspension sutures, and butterfly grafts. Dynamic collapse of the LLC and supra-alar tissue can be remedied by alar batten grafts [4]. The technique of spreader grafts devised by Sheen in 1984 uses two rectangular strips of cartilage taken from the nasal septum and secured between the upper lateral cartilages and the dorsal septum [5]. The method was developed to prevent collapse of the middle nasal vault after hump excision in primary rhinoplasty. Some authors have advocated using spreader grafts preventatively in primary rhinoplasty patients who have short nasal bones and long, weak upper lateral cartilages [6]. The importance of this procedure in preventing complication in primary rhinoplasty is generally stressed [2, 7]. Whether in primary or secondary cases spreader grafts have been reported to improve nasal valve patency by over 80 % [8].
Flaring sutures widen the nasal valve angle. A non-absorbable suture is placed for the caudal/lateral border of one ULC, across the nasal dorsum, and through the contralateral ULC. Tightening of the suture pulls the ULCs laterally and opens the nasal valve angle [9].
Rhinomanometry and peak nasal inspiratory flow (PNIF) are the common objective tests which could be used to assess nasal obstruction. Bermüller et al. [10] compared accuracy of these tests in the diagnosis of functionally relevant structural nasal deformities. They showed both diagnostic techniques are effective to identify subjects with clinically relevant nasal stenosis but a negative test outcome does not exclude functionally relevant nasal stenosis. Schumacher suggests that since rhinomanometry is a functional test of the nasal airway, it may be a better screening tool for nasal airway obstruction [11]. Advantages of rhinomanometry include the possibility to detect side differences and the fact that more physiological airflow conditions prevail during measurement [12].
Rhinomanometry measures both the intranasal air pressure and the rate of airflow during breathing. Active anterior rhinomanometry (the patient is actively breathing through one nasal cavity while the narinochoanal pressure difference is assessed in the contralateral nasal cavity) is the most commonly used method of rhinomanometry. Rhinomanometry measures the pressure difference (Δp) and airflow (V˚) between the posterior and the anterior of the nose during inspiration and expiration. Nasal airway resistance is calculated according to Ohm’s law (R = ΔP/V˚) and is given at a designated point of the pressure-flow curve. According to the ISCR [13] the resistance should be given at a fixed pressure of 150 Pa (R150) or as in Broms’ model as v2. In a normal nose and with the resistance given at 150 Pa according to the ISCR, the median value for unilateral inspiratory nasal airway resistance in the undecongested nose is 0.36 Pa/ml/s (range 0.34–0.40), and for the decongested nose during inspiration 0.26 Pa/ml/s (range 0.25–0.30).
We designed a study to evaluate the results clinical outcomes after using two techniques in open rhinoplasty to reconstruct the middle third of the nose. We analyzed the outcome of surgery with a subjective assessment and objective measurements of nasal patency with rhinomanometry.
Materials and methods
A prospective study was planned on 248 consecutive patients (88 men and 160 women) who were operated on for cosmetic nose deformities at otolaryngology department of Amiralmomenin Hospital between March 2010 and December 2013. This study was supported and approved by the Institutional Review Board (IRB) of Guilan University of Medical Sciences. Informed consent for participating in the study was obtained from all the subjects. These patients were asked to participate in the present study by undergoing a preoperative and a follow-up postoperative rhinomanometry. All patients were questioned pre-operatively regarding any longstanding nasal obstruction and postoperatively (3–6 months after surgery) each was asked whether a change in the function of the nose had been experienced.
The main complaint of all patients was appearance of the nose. None of them had nasal respiratory obstruction linked to the internal or external nasal valve or nasal septum or different combinations of all of them. Inclusion criteria was no septum perforation that can alter the rhinomanometry measurements. Only minor septal deviations were included in this study. Patients were considered affected by septal deviation if the bony and cartilaginous deviation were particularly significant. Exclusion criteria were structural problems such as nasal obstruction, deviated septum, hardening surgery, revision cases, and new clinical conditions or a change in therapeutic techniques. Twenty-eight patients were not available for follow-up and therefore were excluded from the study. The investigation is based on the results from the remaining 220 patients (67 men and 153 women).
The spreader graft or flaring suture technique was selected according to aesthetic and therapeutic parameters. For example, the flaring suture technique was used only in open rhinoplasty. All patients had a straight nose in the midline. At operation 56 of the patients underwent removal of the hump and infracture without alar reduction. In 142 patients alar cartilage reduction was performed in addition to hump removal and infracture. Twenty-two patients had infracture and transposition of alar flaps to lengthen the columella.
Rhinomanometry
All patients in the study were tested by rhinomanometry on admission to hospital and again between three and 6 months following surgery. Patients who complained of a cold or unusual stuffiness were, if seen pre-operatively, excluded from the study or, for the purpose of postoperative assessment, asked to attend at a later date. Active anterior rhinomanometry was performed 10 min after decongestion with phenylephrine nasal spray to minimize the effects of mucosal factors and the nasal cycle. The measurement was done during spontaneous breathing with the patient in a sitting position. Rhinomanometry data were presented as nasal inspiratory resistances indirectly measured from the flow at a reference pressure 150 Pa [13].
Statistical analysis
Distribution of data was analyzed by the kolmogorov–smirnov test. T test and Mann-Whithney U were used to compare parametric and non-parametric data, respectively. Values of P < 0.05 were considered significant.
Results
248 patients (88 men and 160 women; mean age, 28.3 years; SD, 6.9 years) underwent two operations to prevent nasal valve dysfunction in primary rhinoplasty. Twenty-eight patients were unavailable for follow-up. Fifty-one patients had previously undergone septoplasty. All procedures were performed using an open approach; Spreader grafts were placed in 87 (39.5 %) of 220 procedures and flaring sutures were placed in 133 cases. None patients of two groups complained cosmetic problems related to these techniques.
The mean of follow-up was 20.9 ± 2.9 weeks. In spreader grafts and flaring sutures groups, the mean follow-up was 20.5 and 21 weeks, respectively. The difference between mean follow-up of two groups was insignificant. As seen in Table 1, the mean age of the spreader graft group is more than other (P value <0.006). The other demographic variables of patients in both groups were similar.
Before surgery, the median nasal airway resistance of spreader grafts and flaring sutures groups was 0.247 Pa/ml/s (range 0.110–0.250) and 0.247 Pa/ml/s (range 0.120–0.930), respectively. Difference between two groups was insignificant (Mann–Whitney U, P value 0.07). After rhinoplasty, nasal airway resistance decreased in 46 patients (52.9 percent) of spreader grafts group and in 84 patients (63.2 percent) of flaring sutures group. The median nasal airway resistance difference (before–after surgery) of spreader grafts and flaring sutures groups was 0.027 Pa/ml/s (range −0.110 to 0.130) and 0.017 Pa/ml/s (range 0.690–0.790), respectively. Applying the Mann–Whitney U test to compare the change in nasal airway resistance, made by rhinoplasty in the spreader grafts group and in the flaring sutures, the z value was −0.674 and the P value was 0.5 indicating that the difference between two groups was not statistically significant.
One hundred twenty-two patients stated that their noses had felt clearer following rhinoplasty, but in only 104 of these, we could demonstrated any improvement by rhinomanometry. Other patients noticed no change in the function of the nose after surgery, but in 55 of them nasal airway resistances were not changed measurably. Thus, in 159 of 220 patients (72.3 percent) there was a positive correlation between subjective and objective results (Table 2).
In spreader grafts group, follow up evaluation showed a complication in six patients (6.9 %). In four patients, the complication was synechiae between caudal part of the upper lateral cartilage and septum which was treated with local anesthesia. There was a slight posterior upward dislocation of the graft in two female patients. None of them wish for further corrective surgery. We did not observe any complication in flaring sutures group. None of the patients in both groups reported impaired nasal breathing subjectively.
Discussion
There are several works to assess effect of rhinoplasty on nasal breathing. However, there currently exists little work concerning the objective effects of various surgical maneuvers on the nasal airway resistance. In this study, a significant difference between the mean age of two groups could be seen. One assumption to explain this difference could be related to the methodology of study and we tried to match the important factors affecting the nasal resistance in two groups. Additionally, Crouse et al. [14] showed that unlike the pediatric population, age had no effect on nasal airflow rate and nasal or differential pressure in adults. Therefore this difference had no clinical importance.
There was a good agreement between change in nasal airway resistance and change in nasal function in our patients (72.3 percent). Jessen et al. [15] showed that there was agreement for 76 percent between the subjective and rhinomanometric changes. Gordon et al. [16] found that 22 % of patients undergoing septoplasty had persistent subjective obstruction postoperatively despite showing improved rhinomanometric scores. Possible reasons for inaccuracy of rhinomanometry include random error and operating errors. Also rhinomanometry may not accurately reflect changes of nasal airflow in the anterior segments of the nose. This may be due to coupling of nozzles to the external nasal ostium or stabilization of nasal soft tissues by the face mask. It is well known that manipulation of nasal structures may cause turbulences or focus air to limited mucosal areas. These are often sensed as nasal obstruction, but may not be detected by rhinomanometry [12].
The study showed that spreader grafts and flaring sutures improved the nasal airway resistance equally. This finding is contrary to Schlosser’s study on cadavers showed the spreader grafts and flaring sutures alone produced insignificant improvements [1]. In the opinion of Schlosser et al. flaring sutures have a greater impact than spreader grafts and can often be used alone with comparable clinical results. Also Zijlker and Quaedvlieg [8], who used only spreader grafts and noted improved patency in 81 % of their patients. Some authors have challenged the utility of spreader grafts, as they may eliminated to a tendency for the upper lateral cartilages to form a rounded arch and thus narrow the angle of the internal valve [17]. According to Bloching experience, however, this results in an insignificant enlargement of the cross section of the internal nasal valve only since the angle of the nasal valve is changed only negligibly [18].
Procedures that destabilize the fibrous attachments of the upper lateral cartilages, such as dorsal hump reductions, may lead to progressive collapse of the sidewall. When performing such procedures, it is advisable to reattach the upper lateral cartilage to the dorsal cartilaginous septum if the stability of the upper later cartilage is in doubt. Displaced nasal bones may contribute to valvular obstruction because of their relationship to the upper lateral cartilages. For most cases, spreader grafts and flaring sutures are effective in prevention of internal valve narrowing. Ideally, the rhinological surgeon will be able to determine preoperatively which patients will benefit from specific maneuvers. Both methods could be achieved similar results after primary rhinoplasty. Prior septal surgery is not uncommon in patients who are seeking cosmetic surgery. In this condition, Cartilage grafts can be easily achieved. Also in the surgery on the nose with deviation in the midline, the spreader grafts can be useful in improving esthetically and functionally results. The spreader grafts technique can be done in closed rhinoplasty. But when septal cartilage is severely damaged and good cartilage for grafts cannot be harvested, or when septoplasty surgery does not require in conjunction with rhinoplasty, the flaring sutures technique can be useful.
None of the patients of both groups did not report incompetence of the nasal valve. In no cases were there any noteworthy complications caused by the spreader grafts or flaring sutures techniques. However, the scar formation in four patients in the spreader grafts group was reflected to accidental damage to nasal mucosa during the insertion of the graft. The spreader graft displacement was observed in two female patients who had relatively thin nasal skin. Although there was no widening in our patients with spreader grafts, it should be remembered that overwidened nose could be created. Also, graft shifting may result in a palpable or visible irregularity. No complication related to flaring sutures has been reported so far.
Conclusion
We assume that the spreader grafts and the flaring sutures could have similar effect on prevention of nasal airway dysfunction in primary rhinoplasty and should be considered in this cosmetic surgery. However, the importance of these techniques cannot be overemphasized in the clinical setting, unless the results of the present study are reproduced in randomized clinical trials with using objective tests with higher diagnostic accuracy such as combination of rhinomanometry and PNIF methods. Further studies about the effect of combining these techniques for the prevention or management of nasal valve dysfunction are therefore warranted.
References
Schlosser RJ, Park SS (1999) Surgery for the dysfunctional nasal valve. cadaveric analysis and clinical outcomes. Arch Facial Plast Surg 1(2):105–110
Toriumi DM (1995) Management of the middle nasal vault in rhinoplasty. Operat Tech Plast Reconstr Surg 2:16–30
Teller DC (1997) Anatomy of a rhinoplasty: emphasis on the middle third of the nose. Facial Plast Surg 13:241–252
Omranifard M, Abdali H, Rasti Ardakani M, Ahmadnia AY (2013) Comparison of the effects of spreader graft and overlapping lateralcrural technique on rhinoplasty by rhinomanometry. World J Plast Surg 2(2):99–103
Sheen JH (1984) Spreader graft: a method of reconstructing the roof of the middle nasal vault following rhinoplasty. Plast Reconstr Surg 73:230–239
Boccieri A, Macro C, Pascali M (2005) The use of spreader grafts in primary rhinoplasty. Ann Plast Surg 55:127–131
Constantian MB (2000) Four common anatomic variants that predispose to unfavorable rhinoplasty results: a study based on 150 consecutive secondary rhinoplasties. Plast Reconstr Surg 105:316
Zijlker TD, Quaedvlieg PC (1994) Lateral augmentation of the middle third of the nose with autologous cartilage in nasal valve insufficiency. Rhinology 32:34–41
Park SS (1998) The flaring suture to augment the repair of the dysfunctional nasal valve. Plast Reconstr Surg 101:1120–1122
Bermüller C, Kirsche H, Rettinger G, Riechelmann H (2008) Diagnostic accuracy of peak nasal inspiratory flow and rhinomanometry in functional rhinosurgery. Laryngoscope 118(4):605–610
Schumacher MJ (2002) Nasal congestion and airway obstruction: the validity of available objective and subjective measures. Curr Allergy Asthma Rep 2(3):245–251
Chandra RK, Patadia MO, Raviv J (2009) Diagnosis of nasal airway obstruction. Otolaryngol Clin N Am 42(2):207–225
Clement PAR, Gordts F (2005) Consensus report on acoustic rhinometry and rhinomanometry. Rhinology 43:169–179
Crouse U, Laine-Alava MT (1999) Effects of age, body mass index, and gender on nasal airflow rate and pressures. Laryngoscope 109(9):1503–1508
Jessen M, Jacobsson S, Malm L (1988) On rhinomanometry in rhinoplasty. Plast Reconstr Surg 81(4):506–511
Gordon AS, McCaffrey TV, Kern EB, Pallanch JF (1989) Rhinomanometry for preoperative and postoperative assessment of nasal obstruction. Otolaryngol Head Neck Surg 101:20–26
Gassner HG, Friedman O, Sherris DA, Kern EB (2006) An alternative method of middle vault reconstruction. Arch Facial Plast Surg 8(6):432–435
Bloching MB (2007) Disorders of the nasal valve area. GMS Curr Top Otorhinolaryngol Head Neck Surg 6:Doc07 (Epub 2008 Mar 14)
Acknowledgments
I thank the patients for their participation in this study.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jalali, M.M. Comparison of effects of spreader grafts and flaring sutures on nasal airway resistance in rhinoplasty. Eur Arch Otorhinolaryngol 272, 2299–2303 (2015). https://doi.org/10.1007/s00405-014-3327-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3327-5