Abstract
This prospective study assesses outco mes at 6 weeks and 7 months after radical ethmoid surgery in 65 patients with nasal polyposis using a new and detailed instrument, the DyNaChron questionnaire, which was filled in the day prior to surgery and at 6 weeks and 7 months after surgery at follow-up visits. Before surgery, the leading bothersome symptoms were olfactory disturbances (7.74 ± 2.81) and nasal obstruction (6.66 ± 2.28). After surgery (6th week and 7th month), there was a clear improvement of all symptoms including nasal obstruction, olfactory disturbances, anterior rhinorrhea, postnasal discharge, facial pain/headache and cough in comparison to baseline (p < 0.0001). Nasal obstruction was the most improved symptom (effect size of 2.24). At 7th post-operative month, the sense of smell continued to improve slightly. By contrast, the postnasal discharge score that was significantly improved at 6th post-operative week tended to worsen at 7 months (p = 0.0045). Before surgery, strong psychosocial impacts were observed in association with nasal obstruction and anterior rhinorrhea. The physical impacts of each symptom were proportionally correlated to the symptom score before and after surgery. The quality of life (QOL) related to each symptom was clearly better at 6 weeks and remained steady at 7 months after surgery. In conclusion, olfactory disorders and postnasal rhinorrhea were the main remaining symptoms after sinus surgery despite a global improvement of symptoms and quality of life. The earlier time point to stabilize QOL outcomes of endoscopic sinus surgery could be suggested at 6 weeks after surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic dysfunction of the nose and sinuses remains a common medical complaint in the practice of otorhinolaryngology. Assessing objective outcomes after treatment in chronic sinonasal diseases is difficult. For this reason, numerous tools to describe burden of disease illness and treatment outcomes were developed. However, a poor relationship between symptoms and health-related quality of life (QOL) reported by patients and medical findings like those observed with computer tomography (CT) has been showed in many studies [1–4]. Wright and Agrawal [5] found that, in patients with nasal polyposis (NP), there was no significant correlation between patients’ response on the Chronic Sinusitis Survey questionnaire and endoscopic examination scores at any specific time after surgery. Numerous tools under questionnaire forms were developed to try to evaluate disease-related symptoms and treatment outcomes as well as the interactions of symptoms on QOL.
A large number of papers assess patients’ symptoms in chronic rhinosinusitis (CRS) without making the difference between CRS with or without nasal polyps because CRS and NP are currently considered as a continuum of diseases [6]. There are, however, arguments supporting that NP could be a specific disease of the ethmoid [7, 8]. In general, patients with NP have more severe loss of smell [9–11] and nasal obstruction [10, 12] compared with patients without polyps while they report less facial pain and headache [10–12]. Deal et al. [13] also showed that patients with NP have more severe symptoms with less improvement after surgery, higher CT scores at presentation, and a significantly higher need for revision surgery than those without polyps.
Patients with NP reported symptomatic benefits from the endoscopic surgery, independently of the type of surgery (polypectomy, functional ethmoidectomy, or radical ethmoid surgery) [14–16]. The assessment of QOL is recognized as an important alternative outcome measure after treatment [17]. Until now, many specific questionnaires have been developed to assess the QOL of patients with CRS. However, no validated disease-specific instrument is available to assess patients’ QOL linked to NP disease [17].
The aims of the present study were to assess quality-of-life outcomes at 6 weeks and 7 months after radical ethmoid surgery for NP, using a new and detailed instrument—the DyNaChron questionnaire (Dysfonctionnement Nasal Chronique in French or Chronic Nasal Dysfunction in English) which has been validated on a large sample of patients in a prospective multicenter study [18].
Patients and methods
Patients
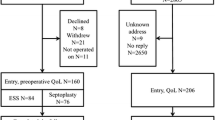
All patients suffering from NP who were operated in our university hospital from January 2010 to December 2011 were enrolled in this prospective study. Only patients filling in the DyNaChron questionnaire before 6 weeks and 7 months after surgery were taken into account to analysis. NP was diagnosed with endoscopic examination and CT scan at initial visit. Surgery was indicated when medical treatment failed to control the symptoms. All patients were operated on both ethmoid using the nasalization procedure [16, 19, 20] with middle and superior turbinate preservation. Additionally, septoplasty was performed if necessary. No systemic corticosteroid or antibiotic treatment was given before or after the surgery. Washing the nose with isotonic saline by means of a syringe at least three times a day and once daily intranasal steroid treatment were started the day after surgery and strongly recommended for the long term. This study was approved by the Institutional Review Board of Nancy University Hospital, France.
Evaluation of symptoms and quality of life
All data were collected prospectively using the DyNaChron questionnaire. This questionnaire includes 78 items divided into 6 domains and explores both the physical and psychosocial repercussions of functional chronic nasal diseases. Each item is scored 0–10, with 0 meaning no discomfort at all and 10 meaning unbearable discomfort. The six main symptoms of chronic nasal dysfunction explored with this tool are nasal obstruction, anterior rhinorrhea, postnasal discharge, olfactory disturbances, facial pain/headache and cough. Physical and psychosocial impacts are assessed for each symptom with different number of items. Psychosocial impacts of each main symptom are assessed with the same four questions. Physical impacts are assessed with different number and specific questions related to each main symptom, 8 for nasal obstruction, 7 for anterior rhinorrhea, 6 for postnasal discharge, 8 for olfactory/gustative disturbances, 13 for facial pain, and 6 for cough. Patients were asked to rate their symptoms and related impacts on the DyNaChron questionnaire by considering their nasal discomfort over the last 15 days. The questionnaire was filled in the day prior to surgery and at 6 weeks and 7 months after surgery at follow-up visits in the waiting room before the medical visit.
Statistics
Continuous variables were expressed as mean ± standard deviation and categorical variables were expressed as frequencies and percentages. The paired Student’s t test was used to evaluate the improvement of each symptom and each impact in comparison with pre-operative scores. For physical impacts, because of the unbalanced number of items in each domain, we rescaled by summing of all physical items of each domain, then dividing by the number of items of each domain. These results were finally multiplied by 10. So, the total physical impact scores of each symptom varied from 0 to 100. Regarding psychosocial impacts, there were four items for each main domain. We converted the total score of psychosocial impacts related to each domain on a 0–100 scale (total scores were divided by 4 then multiplied by 10). The effect size—the average change divided by the baseline standard deviation—at ≥0.5 was defined as the threshold of discrimination for changes in health-related QOL for chronic diseases [21]. Statistical analyses were performed using SAS V9.1 software (SAS Inst., Cary, NC) and two-sided p value <0.05 was considered significant.
Results
A total of 65 patients (mean age 51 ± 12.8 years) answered the DyNaChron questionnaire before surgery, 6 weeks (mean 40.9 ± 9.7 days) and 7 months (mean 261.7 ± 29.8 days) after surgery. Of those, 34 patients (52.31 %) were male and 38 patients (58.46 %) had a history of previous sinus surgery.
Main symptoms before surgery (Table 1)
Before surgery, the leading bothersome symptoms in patients with NP were sense of smell disturbances (score was 7.74 ± 2.81) and nasal obstruction (6.66 ± 2.28). The anterior rhinorrhea and postnasal discharge scores were similar (4.85 ± 3.42 and 5.08 ± 3.20, respectively, p = 0.66). There was a significant difference between nasal obstruction score and anterior rhinorrhea (p < 0.0001) or postnasal discharge scores (p = 0.0027). The facial pain score (4.12 ± 3.59) was significantly lower than scores for nasal obstruction (p < 0.0001) and olfactory disturbances (p < 0.0001), but was not significantly different from anterior rhinorrhea (p = 0.13), postnasal discharge (p = 0.0503) and cough (p = 0.056). The cough score (3.05 ± 3.22) was lower than the other symptom scores (p < 0.0001 for nasal obstruction, anterior rhinorrhea, postnasal discharge, and olfactory disturbances).
Evolution of symptoms after surgery (Table 1; Fig. 1)
At 6 weeks after surgery, there was a clear improvement of all symptoms in comparison to baseline (p < 0.0001). Nasal obstruction was the most improved symptom (score from 6.66 to 1.56 corresponding to an effect size of 2.24, which, by convention, is considered a large improvement in health-related QOL [21]). The effect-size for other symptoms was 1.42 (sense of smell), 1.04 (postnasal drip), 1.0 (anterior rhinorrhea), 0.62 (pain), and 0.58 (cough).
At 7 months after surgery, nasal obstruction showed a steady improvement, whereas sense of smell continued to improve slightly (the score was 3.75 ± 3.56 at 6 weeks and became 3.46 ± 3.60 at 7 months, p = 0.49). By contrast, the postnasal discharge score tended to worsen (the score changed from 1.75 ± 2.18 at 6 weeks to 2.82 ± 2.78 at 7 months, p = 0.0045).
Figure 1 shows that the nasal obstruction score was strongly reduced at 6 weeks (p < 0.0001) and remained steady at 7 months after surgery. The olfactory disturbance score was strongly reduced at 6 weeks (p < 0.0001) and continued to decrease slightly (p = 0.49). Also, the anterior rhinorrhea and postnasal discharge scores were strongly reduced at 6 weeks (p < 0.0001), but went up strongly for postnasal discharge (p = 0.0045) at 7 months. The facial pain and cough scores diminished moderately at 6 weeks and remained stable at 7 months after surgery.
Physical impacts (Table 2 and Fig. 2)
The physical impacts of each symptom were proportionally correlated to the symptom score and strongly improved after surgery (p < 0.05, all results of statistical tests were not shown in the Table 1). Physical impacts were the highest for olfactory disturbances before and after surgery, whereas nasal obstruction, anterior rhinorrhea and postnasal discharge impact moderately on physical fields. Facial pain and cough had the less physical impacts.
Table 1 shows that nasal obstruction had pre-operatively strong impacts on the ability to smell (mean score was 7.68 ± 2.96), to breathe through the mouth (6.12 ± 3.03), to fall asleep (5.37 ± 2.90) and to exercise (5.65 ± 3.28). For anterior rhinorrhea, the need to blow the nose in the morning was the most bothering impact (mean score was 6.0 ± 3.01) then the need to sniff the nose (5.93 ± 2.86). For postnasal discharge, the more bothersome impacts were the need to clear the throat (mean score was 4.58 ± 3.14), the feeling of mucus stuck in the throat (4.65 ± 3.36), the need to spit (4.67 ± 3.29), hoarseness (4.39 ± 3.32) and the disturbance of sleep (3.83 ± 3.23). Sense of smell had the highest impact scores before and after surgery with the inability to detect dangerous smells (mean score was 7.0 ± 3.65) and cooking smells (7.06 ± 3.50), to smell hygiene products (7.05 ± 3.42), to smell personal body odors her/him-self (6.92 ± 3.45), to detect unpleasant smells (6.65 ± 3.71). Physical impacts of other domain are detailed in Table 1.
Psychosocial impacts
Pre- and post-operative psychosocial impacts of each domain are detailed in Table 1. Before surgery, strong psychosocial impacts were observed in association with nasal obstruction and anterior rhinorrhea (with a similar psychosocial score, p = 0.13), then to facial pain and olfactory disturbances. At the two assessment points after surgery, the psychosocial impacts of all symptoms were decreased. Facial pain and olfactory disturbances became, however, the most bothersome psychosocial impacts in comparison to the other symptom-related impacts (p < 0.05) at 6 weeks after surgery. At 7 months, facial pain remained the main symptom that impacted severely on the psychosocial side in comparison to nasal obstruction (p = 0.008), or postnasal drip (p = 0.026) (Fig. 3). There was no significant difference between psychosocial impacts of facial pain and those of olfactory disturbances (p = 0.4), anterior rhinorrhea (p = 0.052) and cough (p = 0.22).
Discussion
NP is not a life-threatening disease, but our study shows that this chronic disease can severely disturb patients’ QOL. These interactions on QOL were closely related to six main symptoms of NP: nasal obstruction, anterior rhinorrhea, postnasal drip, loss in the sense of smell, facial pain/headache, and cough. Improvement of symptoms and QOL after surgery for NP was well documented [9, 14, 22–26].
Patients’ reports of symptoms and impacts on QOL revealed to be different among studies. Olfactory disturbances have been reported either as the most severe [27] or the least severe symptom [28] when assessing symptoms before surgery. Headache as well as postnasal discharge has been reported either to improve after surgery [11] or not at all [29]. These controversies may be explained by heterogeneity in studied populations (including the mixture of CRS with or without polyps) as well as in instruments for assessment. Our findings are in accordance with the results of some studies in which CRS and NP are considered as two different entities [9, 11, 30]. Before treatment, major complaints of patients with NP were found to be impairment/loss of smell, nasal obstruction [9, 11], and rhinorrhea [30] while patients with CRS presented with more facial pain and headache [11, 30].
Our results show that NP patients with nasal obstruction rated a high score of discomfort for smelling, breathing, sleep, and physical exertion. Serrano et al. [31] reported that NP had a twofold higher risk of sleep disturbance than controls. Nasal obstruction is due to polyps which block the nasal airflow. This blockage disturbs the nasal respiration and by consequence the sleep. Sleep impairment can likewise be caused by the release of inflammatory mediators [32]. By consequence, patients feel tired during the day influencing the psychosocial side. In our study, patients reported an important improvement of nasal obstruction as well as its physical and psychosocial impacts after surgery as nasal cavities becomes free.
The sense of smell is essential in our everyday life in exploring the environment. The olfactory disturbances lead to concerns related to food enjoyment, self-hygiene maintenance, domestic accidents as well as mood disorders and sexual activities [33]. Our results showed the same ascertainments in patients with NP, in whom the impairment/loss of smell was the leading complaint before surgery. The importance of olfactory loss in patients with NP may be due to the presence of respiratory epithelial adenomatoid hamartoma besides eosinophilic polyps in the olfactory clefts [34]. Despite the important change of olfactory scores after surgery for NP, the impairment/loss of smell remained an important residual symptom at 6 weeks and 7 months postoperatively. After surgery, patients still had the same concerns, but the intensity was less important than before surgery thanks to surgical benefit. We observed that smell disturbances were rated with a highest score of symptom discomfort, but were not rated as the most unbearable psychosocial impacts. It could be explained by the patients’ ignorance or habituation for these troubles.
Rhinorrhea may reflect indirectly the inflammatory phenomenon of the sinonasal mucosa. Rhinorrhea is the most bothersome symptom in some patients and the main symptom which patients wished to get rid of. We showed the postnasal rhinorrhea tended slightly to go up at 7 months after surgery. This useful information allows clinician to warn their patients before surgery. The increased postnasal rhinorrhea scores at 7 months after surgery probably reflects the chronic state of the inflammatory disease which underlines NP. In our practice, the endonasal steroid treatment is systematically recommended for the long term in patients with NP after surgery to control the inflammatory phenomenon. We did not assess, however, the possible relationship between the compliance of intranasal steroid treatment and recurrence of postnasal discharge.
Moderate or severe facial pain/headache was reported in only 16–18 % of patients with NP [35, 36]. The co-existence of neurologic facial pain/headache and nasal disease complicates the diagnosis and the adapted treatment. Daudia and Jones reported 29 % of patients with migraine (15/51) had co-existing nasal disease [37]. About a half of patients with NP reported very mild to severe pain in our study. This could be due to the tool used to assess the pain. In fact, the 0- to 10-point analog scale is shrewder than the 5-point or 3-point scales and allows to detect a minimal complaint. The mean score of facial pain/headache was considered as mild–moderate pre-operatively (4.12/10) and very mild postoperatively (1.89 and 1.98/10). It signifies that surgery of NP improved facial pain/headache. Physical impacts of facial pain/headache were decreased more importantly than psychosocial impacts.
Cough was the least complaint in terms of frequency as well as intensity among six main domains. Its impacts seem more important on psychosocial field than physical field before surgery. Once again, endoscopic surgery can improve cough and its impacts in patients with NP. The cough improvement may be due to improvement of either postnasal rhinorrhea or lower airway inflammation [22].
QOL in patients with NP was assessed, over different studies, by different instruments including generic and specific questionnaires. In 1997, the American Academy of Otolaryngology—Head and Neck Surgery Rhinosinusitis Task Force suggested that the results of endoscopic outcome studies are best evaluated by both VAS severity scoring and QOL assessment [38]. Van Oene et al., in a systematic review published in 2007, identified that the RQLQ and RSOM-31 were the top scoring instruments with adequate levels of discriminate validity and responsiveness for rhinosinusitis on the basis of criterion for quality-assessment [39]. In 2012, we published a new questionnaire (DyNaChron) to assess six main symptoms (nasal obstruction, anterior rhinorrhea, postnasal drip, olfactory reduction or loss, facial pain/headache, and cough) and consequences in patients with a chronic nasal dysfunction [18]. This questionnaire includes items evaluated with a 0–10 point scale allowing to assess small changes and responds to criterion for quality-assessment. The DyNaChron questionnaire allows not only to globally assess the symptoms’ severity and interactions with QOL, but also to evaluate outcomes of NP treatment.
Our results show that QOL outcomes tend to stabilize at 6 weeks after surgery for NP in the majority of nasal symptoms except rhinorrhea. This study does not allow conclusions about sustained benefit for symptoms and QOL changes that would occur beyond 7th post-operative months. However, Soler et al. found that QOL outcomes after ESS stabilized among 6-, 12-, and 20-month follow-up time points [26]. Also, Hopkins et al. found a relative stabilization of SNOT-22 scores at 3, 12 and 36 months after surgery for NP [14]. Thus, we could speculate that the early time point to evaluate stabilized QOL outcomes of ESS is at 6 weeks after surgery.
Treatment decision of NP is essentially based on subjective patients’ complaints. So, treatment outcomes of NP have to be assessed with symptom-related questionnaires looking at interaction with QOL. It means that surgical success should be determined by the patient and not the surgeon [25]. Awareness of the probability of specific symptom improvement after endoscopic surgery permits more accurate estimations of surgical success in individual patients [40]. This information allows clinician to know what their patients wait for and to inform them of possible outcomes of the treatment. It also aids the patient to consider the risks and benefits of the surgical treatment even if there is a low surgery-related complication [14]. In terms of follow-up, the questionnaire DyNaChron can give to the clinician important feedback. It also guides the physician, in terms of future care, to draw a strategy in order to better treat his patients according to their complaints.
Conclusion
The DyNaChron questionnaire allows assessing the symptom-related severity and QOL before as well as after surgery for NP. This study shows that impairment in or loss of smell and postnasal rhinorrhea were the main remaining symptoms after sinus surgery despite a global improvement of symptoms and QOL. The earlier time point to stabilize QOL outcomes of ESS could be suggested at 6 weeks after surgery.
References
Bhattacharyya T, Piccirillo J, Wippold FJ 2nd (1997) Relationship between patient-based descriptions of sinusitis and paranasal sinus computed tomographic findings. Arch Otolaryngol Head Neck Surg 123(11):1189–1192
Shields G, Seikaly H, LeBoeuf M, Guinto F, LeBoeuf H, Pincus T, Calhoun K (2003) Correlation between facial pain or headache and computed tomography in rhinosinusitis in Canadian and US subjects. Laryngoscope 113(6):943–945
Hwang PH, Irwin SB, Griest SE, Caro JE, Nesbit GM (2003) Radiologic correlates of symptom-based diagnostic criteria for chronic rhinosinusitis. Otolaryngol Head Neck Surg 128(4):489–496
Basu S, Georgalas C, Kumar BN, Desai S (2005) Correlation between symptoms and radiological findings in patients with chronic rhinosinusitis: an evaluation study using the Sinonasal Assessment Questionnaire and Lund-Mackay grading system. Eur Arch Otorhinolaryngol 262(9):751–754
Wright ED, Agrawal S (2007) Impact of perioperative systemic steroids on surgical outcomes in patients with chronic rhinosinusitis with polyposis: evaluation with the novel Perioperative Sinus Endoscopy (POSE) scoring system. Laryngoscope 117(11 Pt 2 Suppl 115):1–28
Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F et al (2012) European position paper on rhinosinusitis and nasal polyps. Rhinol Suppl 23:1–298 (3 p preceding table of contents)
Jankowski R (2011) Revisiting human nose anatomy: phylogenic and ontogenic perspectives. Laryngoscope 121(11):2461–2467
Jankowski R (2013) The evo-devo origin of the nose. Anterior Skull Base and Midface, Springer Verlag Paris. ISBN 978-2817804217
Alobid I, Benítez P, Bernal-Sprekelsen M, Roca J, Alonso J, Picado C, Mullol J (2005) Nasal polyposis and its impact on quality of life: comparison between the effects of medical and surgical treatments. Allergy 60(4):452–458
Banerji A, Piccirillo JF, Thawley SE, Levitt RG, Schechtman KB, Kramper MA, Hamilos DL (2007) Chronic rhinosinusitis patients with polyps or polypoid mucosa have a greater burden of illness. Am J Rhinol 21(1):19–26
Bugten V, Nordgård S, Romundstad P, Steinsvåg S (2008) Chronic rhinosinusitis and nasal polyposis; indicia of heterogeneity. Rhinology 46(1):40–44
Poetker DM, Mendolia-Loffredo S, Smith TL (2007) Outcomes of endoscopic sinus surgery for chronic rhinosinusitis associated with sinonasal polyposis. Am J Rhinol 21(1):84–88
Deal RT, Kountakis SE (2004) Significance of nasal polyps in chronic rhinosinusitis: symptoms and surgical outcomes. Laryngoscope 114(11):1932–1935
Hopkins C, Browne JP, Slack R, Lund V, Topham J, Reeves B, Copley L, Brown P, van der Meulen J (2006) The national comparative audit of surgery for nasal polyposis and chronic rhinosinusitis. Clin Otolaryngol 31(5):390–398
Devars du Mayne M, Prulière-Escabasse V, Zerah-Lancner F, Coste A, Papon JF (2011) Polypectomy compared with ethmoidectomy in the treatment of nasal polyposis. Arch Otolaryngol Head Neck Surg 137(2):111–117
Jankowski R, Bodino C (2003) Evolution of symptoms associated to nasal polyposis following oral steroid treatment and nasalization of the ethmoid–radical ethmoidectomy is functional surgery for NPS. Rhinology 41(4):211–219
Alobid I, Bernal-Sprekelsen M, Mullol J (2008) Chronic rhinosinusitis and nasal polyps: the role of generic and specific questionnaires on assessing its impact on patients’ quality of life. Allergy 63(10):1267–1279
Kacha S, Guillemin F, Jankowski R (2012) Development and validity of the DyNaChron questionnaire for chronic nasal dysfunction. Eur Arch Otorhinolaryngol 269(1):143–153
Jankowski R, Pigret D, Decroocq F, Blum A, Gillet P (2006) Comparison of radical (nasalisation) and functional ethmoidectomy in patients with severe sinonasal polyposis. A retrospective study. Rev Laryngol Otol Rhinol (Bord) 127(3):131–140
Jankowski R (2010) Nasalisation in the surgical treatment of nasal polyposis. In: Onerci M, Ferguson BJ (eds) Nasal polyposis: pathogenesis, medical and surgical treatment. Springer, Berlin, pp 265–274
Norman GR, Sloan JA, Wyrwich KW (2003) Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 41(5):582–592
Ehnhage A, Olsson P, Kölbeck KG, Skedinger M, Dahlén B, Alenius M, Stjärne P, NAFS Study Group (2009) Functional endoscopic sinus surgery improved asthma symptoms as well as PEFR and olfaction in patients with nasal polyposis. Allergy 64(5):762–769
Ehnhage A, Olsson P, Kölbeck KG, Skedinger M, Stjärne P, NAFS Study Group (2012) One year after endoscopic sinus surgery in polyposis: asthma, olfaction, and quality-of-life outcomes. Otolaryngol Head Neck Surg 146(5):834–841
Radenne F, Lamblin C, Vandezande LM, Tillie-Leblond I, Darras J, Tonnel AB, Wallaert B (1999) Quality of life in nasal polyposis. J Allergy Clin Immunol. 104(1):79–84
Conte LJ, Holzberg N (1996) Functional endoscopic sinus surgery, symptomatic relief: a patient perspective. Am J Rhinol 10(3):135–140
Soler ZM, Smith TL (2010) Quality-of-life outcomes after endoscopic sinus surgery: how long is long enough? Otolaryngol Head Neck Surg 143(5):621–625
Young J, Frenkiel S, Tewfik MA, Mouadeb DA (2007) Long-term outcome analysis of endoscopic sinus surgery for chronic sinusitis. Am J Rhinol 21(6):743–747
Bhattacharyya N (2004) Symptom outcomes after endoscopic sinus surgery for chronic rhinosinusitis. Arch Otolaryngol Head Neck Surg 130(3):329–333
Soler ZM, Mace J, Smith TL (2008) Symptom-based presentation of chronic rhinosinusitis and symptom-specific outcomes after endoscopic sinus surgery. Am J Rhinol 22(3):297–301
Dietz de Loos DA, Hopkins C, Fokkens WJ (2013) Symptoms in chronic rhinosinusitis with and without nasal polyps. Laryngoscope 123(1):57–63
Serrano E, Neukirch F, Pribil C, Jankowski R, Klossek JM, Chanal I, El Hasnaoui A (2005) Nasal polyposis in France: impact on sleep and quality of life. J Laryngol Otol 119(7):543–549
Craig TJ, Ferguson BJ, Krouse JH (2008) Sleep impairment in allergic rhinitis, rhinosinusitis, and nasal polyposis. Am J Otolaryngol 29(3):209–217
Temmel AF, Quint C, Schickinger-Fischer B, Klimek L, Stoller E, Hummel T (2002) Characteristics of olfactory disorders in relation to major causes of olfactory loss. Arch Otolaryngol Head Neck Surg 128(6):635–641
Nguyen DT, Gauchotte G, Nguyen-Thi PL, Jankowski R (2013) Does surgery of the olfactory clefts modify the sense of smell? Am J Rhinol Allergy 27(4):317–321
Fahy C, Jones NS (2001) Nasal polyposis and facial pain. Clin Otolaryngol Allied Sci 26(6):510–513
Eweiss AZ, Lund VJ, Barlow J, Rose G (2013) Do patients with chronic rhinosinusitis with nasal polyps suffer with facial pain? Rhinology 51(3):231–235
Daudia AT, Jones NS (2002) Facial migraine in a rhinological setting. Clin Otolaryngol Allied Sci 27(6):521–525
Lanza DC, Kennedy DW (1997) Adult rhinosinusitis defined. Otolaryngol Head Neck Surg 117(3 Pt 2):S1–S7
Van Oene CM, van Reij EJ, Sprangers MA, Fokkens WJ (2007) Quality-assessment of disease-specific quality of life questionnaires for rhinitis and rhinosinusitis: a systematic review. Allergy 62(12):1359–1371
Chester AC, Antisdel JL, Sindwani R (2009) Symptom-specific outcomes of endoscopic sinus surgery: a systematic review. Otolaryngol Head Neck Surg 140(5):633–639
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nguyen, D.T., Guillemin, F., Arous, F. et al. Assessment of quality-of-life outcomes after surgery for nasal polyposis with the DyNaChron questionnaire. Eur Arch Otorhinolaryngol 272, 367–375 (2015). https://doi.org/10.1007/s00405-014-3109-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-3109-0