Abstract
The objective of the study was to determine the temporal occurrence of cochlear obliteration following translabyrinthine vestibular schwannoma resection. A retrospective chart review, cross-sectional study, and sequential analysis of the time series were performed. The retrospective study included patients undergoing translabyrinthine resection for stage T1–T2 vestibular schwannoma from 2007 to 2010 without prior therapy and postoperative follow-up including MRI of the brain and the cerebellopontine angle. Already 3 months after surgery a radiographic labyrinthine change was observed in 66.7 %, a partial obstruction in 50 %, and an obstruction limited to the saccule in 16.7 %. Only 33.3 % of the patients showed an unchanged inner ear. In consideration of early cochlear obstruction after translabyrinthine vestibular schwannoma resection, temporary follow-up is necessary. Since the indications for cochlear implantation (CI) have been extended, especially concerning patients with single-side deafness, a simultaneous or early second-stage CI after tumour removal should be discussed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Fibrosis or ossification of the inner ear arises from vascular compromise and inflammatory processes such as middle ear infection, meningitis, labyrinthitis, and sepsis. Labyrinthine ossification is also observed after previous trauma or surgery of the temporal bone [1, 2]. Vascular occlusions were found to play an important role in the pathogenesis [3, 4]. Experimental occlusion of the labyrinthine artery in animals results in progressive fibrosis and osteoneogenesis of the cochlea [3, 4]. Therefore, neo-ossification does not only occur soon after surgical destruction of the cochlea during translabyrinthine vestibular schwannoma removal and labyrinthectomy, but also after middle fossa approaches. Histological examinations of temporal bones demonstrated severe haemorrhages of the cochlea at 17 h and consecutive ossification and damage of the spiral ganglion cells and cochlear nerve 4–11 years after translabyrinthine surgery [5]. These early degenerations of the cochlea limit the hearing rehabilitation by cochlear implantation (CI), especially if there is a significant delay between vestibular schwannoma surgery and CI, although sparing the cochlea nerve [6]. As hearing loss is the most common complaint after vestibular schwannoma surgery, implicating a worse quality of life [7, 8], it is important to detect the right time interval for a possible CI. Many authors recommend a simultaneous or subsequent CI soon after surgery without specifying the remaining scope [6, 9–11]. There are numerous histological studies demonstrating the changes in the cochlea of the temporal bones after vestibular schwannoma surgery during the lifetime [5, 12, 13]. Furthermore, examination of the signal intensity change of the cochlea in two- or three-dimensional FLAIR sequence MR imaging (MRI) of vestibular schwannoma patients without prior surgery [14, 15] and studies describing early cochlea ossification after meningitis in high-resolution computed tomographic scans [16] are available. The MRI is an excellent tool to show details concerning fibrous or osseous changes to the cochlea in the membranous labyrinth, with a sensitivity of 100 % in predicting cochlear obstruction [17]. However, magnetic resonance appearances of the inner ear were described in patients who underwent surgery of acoustic neuroma after a middle fossa approach [2]. The objective of this examination was to document the onset and extent of labyrinthine obliteration after translabyrinthine vestibular schwannoma resection was detected in T2-weighted high-resolution MRI.
Materials and methods
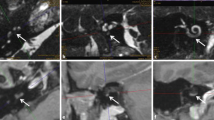
Twenty-six patients surgically treated for unilateral T1–T2 vestibular schwannoma via a translabyrinthine approach at the Department of Otorhinolaryngology, Head and Neck Surgery of the Duesseldorf University Hospital were retrospectively reviewed for a 3-year period between 2007 and 2010. Patients with vestibular schwannomas operated via other approaches (e.g. retrosigmoid, middle fossa approach), a prior conventional or gamma knife surgery, or without at least 14 months of follow-up including MRI of the brain and the cerebellopontine angle were not evaluated. Twelve of 26 patients were excluded because the MRI scans were not performed in our neuroradiology department and were not available or insufficient for an assessment of the cochlea. The patient characteristics of the remaining 14 patients are demonstrated in Table 1. The IRB approval was obtained in May 2012 by the Institutional Review Board of Duesseldorf University. Patients obtained one to three postoperative MRI scans, which were performed annually during regular follow-up visits. Additional scans were performed when patients were symptomatic. A neuroradiologist retrospectively reviewed each MRI scan and classified each ear into four groups: absence of any morphologic labyrinthine change (e.g. Fig. 1), obliteration of the saccule, partial obliteration of the cochlea (e.g. Fig. 2), and complete obliteration of the cochlea (e.g. Fig. 3) based on T2-weighted scans. From a total of 25 postoperative routine T2-weighted scans, 23 high-resolution 3D-CISS (constructive interference in steady state) data sets with 0.6- to 0.8-mm slice thickness and two postoperative conventional T2-weighted data sets with 5-mm slice thickness and satisfactory visualisation of the labyrinth were evaluated. All examinations were performed on 1.5- or 3-Tesla units. MRI scans were performed between 2009 and 2012, with a follow-up ranging from 1 to 47 months postoperatively. The data were entered into an Excel spreadsheet (Table 2), and a descriptive statistic was compiled in terms of two cross-sectional studies and one sequential analysis of the time series (Table 3).
Results
Twenty-five MRI scans were reviewed to assess the time course of signal intensity of the inner ear after removal of the translabyrinthine vestibular schwannoma. In a total of 14 patients, a high rate of morphologic labyrinthine changes in the postoperative routine T2-weighted MRI was noticed independently of the time interval or frequency of examination.
To focus on the time of diagnosed radiographic cochlear obstruction we established a first cross-sectional study after 1 year. 88.9 % of our patients had evidence of labyrinthine obstruction: there was complete cochlear obstruction in 33.3 %, the cochlea was partially obstructed in 22.2 %, and the obstruction was limited to the saccule in 33.3 %. There was a low rate in the remaining 11.1 % without any change of signal intensity 1 year or later after translabyrinthine surgery.
Due to these distinctive morphologic changes of the inner ear, a second cross-sectional study after a considerably shorter time slice of 3 months after surgery was issued. In this study a radiographic labyrinthine change was observed in 66.7 %. A partial obstruction was observed in 50 % and an obstruction limited to the saccule in 16.7 %. Only 33.3 % showed an unaffected inner ear 3 months after vestibular schwannoma resection (Table 3).
The sequential analysis of the time series showed a severe increase of labyrinthine obliteration in 50 % on comparing the MRI scans performed 3 months post-surgery to those performed after 1 year or later.
Discussion
If hearing was lost after unilateral resection of a vestibular schwannoma, a cochlear implant (CI) would be one possible strategy for acoustic rehabilitation to reach a binaural/stereophonic hearing. Hearing loss not only occurs suddenly during the course of operation in translabyrinthine procedures attributed to surgical trauma, but a decrease in hearing is also observed over time in the majority of patients after a middle fossa or retrosigmoid approach with initial hearing preservation, possibly due to a loss of terminal blood supply via the labyrinthine artery [2–4, 6, 18]. Cochlear implantation was successfully performed after a retrosigmoid and middle fossa approach as well as after labyrinthectomy [11, 19, 20]. This strategy implies not only a preserved cochlear nerve, but also patency of the cochlear turns. Fibrosis and ossification of the cochlea after tumour removal can lead to surgical failure of a delayed CI insertion, as described by Aristegui [19] 1 year after translabyrinthine VS removal in the case of a neurofibromatosis 2 (NF-2). Subsequent [9, 21] and simultaneous [19, 22, 23] CI after vestibular schwannoma surgery is discussed by several authors with different outcomes. The first simultaneous resection of a VS and CI in an NF-2 patient was presented by Arriaga and Marks [23] in 1995. The following simultaneous and early implantations 6 weeks to 4 months after tumour removal showed good postimplantation outcomes [9, 19, 21, 24]. There were also delayed but successfully performed implantations after 5–96 months [25–27]. Most authors recommend a simultaneous or early second-stage implantation before degenerative changes affect the cochlea [5, 6, 12, 19, 22], but there has been no other report on radiographic cochlear obstruction after translabyrinthine vestibular schwannoma resection in MR imaging. Our results already show a radiographic labyrinthine change in 66.7 % after 3 months postoperatively, and 88.9 % of our patients had evidence of labyrinthine obstruction after 1 year, making insertion of an intracochlear electrode impossible. Focusing on our very early findings in MRI scans after 3 months, the progress of labyrinthine obliteration of each patient shows a high individual range: two of our patients showed no or only a partial obliteration of the cochlea that ended up in total obliteration at 1 year; two patients remained only partially obstructed at 1 year. The reason for such a different progression is still unclear. Various etiologies for cochlear obliteration are discussed, with the most early and extensive being observed after meningitis [1–5, 28]. The reason for a fast advance of cochlear obliteration after a translabyrinthine approach might be the combination of different causes, such as surgical trauma and consecutive labyrinthine infection [28].
The two rapid developments of total cochlear obliterations show how tight the time frame for uneventful hearing rehabilitation by cochlear implantation can be, which are implications for early implantation. None of our retrospectively analysed patients received a cochlear implant, and one patient with a good contralateral hearing status required a CROS-BAHA rehabilitation.
Although our retrospective data sets show inhomogeneity concerning the postoperative time interval of the MRI and the performance with different scanner magnet strengths, they underline the advice of a contemporary follow-up and the implication for early implantation. It should include very early high-resolution MRI of the inner ear and a discussion of a CI after translabyrinthine VS resection in one procedure, or a sequential or sleeper cochlea electrode array which is replaced in the subsequent CI placement. Among the ossifications, a prolonged postoperative time interval, inappropriate electrophysiological testing as well as good contralateral hearing can influence the performance after CI implantation [29, 30]. The easier control of early complication after tumour surgery and the attempt of hearing augmentation with hearing aids including CROS rehabilitations argue for a contemporary sequential procedure within 3–4 months, provided that early control MRI were conducted.
In small intralabyrinthine vestibular schwannomas, a simultaneously performed procedure may be reasonable.
Future prospective studies with predetermined time intervals of postoperative high-resolution 3D-CISS MRI scans with equal scanner magnet strengths would be of great interest and helpful to integrate the here-presented data to the literature.
Conclusion
After translabyrinthine vestibular schwannoma resection, cochlea changes occur earlier than expected. An early follow-up should be offered to these patients and a contemporary sequential cochlear implant or a placeholder electrode array discussed before tumour removal.
References
Swartz JD, Mandell DM, Faerber EN et al (1985) Labyrinthine ossification: etiologies and CT findings. Radiology 157(2):395–398
Warren FM 3rd, Kaylie DM, Aulino JM, Jackson CG, Weissman JL (2006) Magnetic resonance appearance of the inner ear after hearing-preservation surgery. Otol Neurotol 27(3):393–397
Perlmann H, Kimura R, Fernandez C (1959) Experiments on temporary obstruction of the internal auditory artery. Laryngoscope 69:591–612
Belal A (1980) Pathology of vascular sensorineural hearing impairment. Laryngoscope 90:1831–1839
Belal A (2001) Is cochlea implantation possible after acoustic tumor removal? Otol Neurotol 22:497–500
Zanetti D, Campovecchi CB, Pasini S, Nassif N (2008) Simultaneous translabyrinthine removal of acoustic neuroma and cochlea implantation. Auris Nasus Larynx 35:562–569
Rahmeh C, Magnan J (2010) Quality of life of patients following stages III–IV vestibular schwannoma surgery using the retrosigmoid and translabyrinthine approaches. Auris Nasus Larynx 37(5):546–552 Epub 2010 Feb 24
Wiegand DA, Fickel V (1989) Acoustic neuroma—the patient’s perspective: subjective assessment of symptoms, diagnosis, therapy, and outcome in 541 patients. Laryngoscope 99(2):179–187
Hoffmann R, Kohan D, Cohen N (1992) Cochlea implants in management of bilateral acoustic neuromas. Am J Otol 13:525–528
Shin YJ, Frayssee B, Sterkers O, Bouccara D, Rey A, Lazorthes Y (1998) Hearing restoration in posterior fossa tumours. Am J Otol 19:649–653
Hulka F, Benard EJ, Pillsburg HC (1995) Cochlea implantation in a patient after removal of an acoustic neuroma. The implication of magnetic resonance imaging with gadolinium on patient management. Arch Otolaryngol Head Neck Surg 121:465–468
Chen DA, Linthicum FH, Rizer FM (1988) Cochlea histopathology in the labyrinthectomized ear: implications for cochlea implantation. Laryngoscope 98(11):1170–1172
Belal A Jr, Linthicum FH Jr, House WF (1982) Acoustic tumor surgery with preservation of hearing. A histopathologic report. Am J Otol 4(1):9–16
Lee IH, Kim HJ, Chung WH et al (2010) Signal intensity change of the labyrinth in patients with surgically confirmed or radiologically diagnosed vestibular schwannoma on isotropic 3D fluid-attenuated inversion recovery MR imaging at 3 T. Eur Radiol 20:949–957
Bhadelia RA, Tedesco KL, Hwang S et al (2008) Increased cochlear fluid-attenuated inversion recovery signal in patients with vestibular schwannoma. Am J Neuroradiol 29:720–723
Durisin M, Bartling S, Arnoldner C et al (2010) Cochlea osteogenesis after meningitis in cochlear implant patients: a retrospective analysis. Otol Neurotol 31(7):1072–1078
Brandon I, Booth T, Kutz JW, Lee KH, Roland PS (2009) Labyrinthitis ossificans: How accurate is MRI in predicting cochlea obstruction? Otolaryngol Head Neck Surg 140:692–696
Thomsen J, Stougaard M, Becker B, Tos M, Jennum P (2000) Middle fossa approach in vestibular schwannoma surgery. Postoperative hearing preservation and EEG changes. Acta Otolaryngol 120:517–522
Aristegui M, Denia A (2005) Simultaneous cochlea implantation and translabyrinthine removal of vestibular schwannoma in an only hearing ear: report of two cases (neurofibromatosis type 2 and unilateral vestibular schwannoma). Otol Neurotol 26:205–210
Kveton JF, Abbot C, April M, Drumheller G, Cohen N, Poe DS (1989) Cochlear implantation after transmastoid labyrinthectomy. Laryngoscope 99:610–613
Tono T, Ushisako Y, Morimitsu T (1997) Cochlear implantation in an intralabyrinthine acoustic neuroma patient after resection of an intracanalicular tumor. Adv Otorhinolaryngol 52:155–157
Ahsan S, Telischi F, Hodges A, Balkany T (2003) Cochlea implantation concurrent with translabyrinthine acoustic neuroma resection. Laryngoscope 113:472–474
Arriga MM, Marks CS (1995) Simultaneous cochlea implantation and acoustic neuroma resection: imaging considerations, technique and functional outcome. Otolaryngol Head Neck Surg 112:325–328
Zwolan TA, Shepard NT, Niparko JK (1993) Labyrinthectomy with cochlea implantation. Am J Otol 14:220–223
Lustig LR, Yeagle J, Niparko JK, Minor LB (2003) Cochlear implantation in patients with bilateral Ménière′s disease. Otol Neurotol 4:397–403
Graham J, Lynch C, Weber B, Stollverck L, Wei J, Brookes G (1999) The magnetless Clarion cochlear implant in a patient with neurofibromatosis 2. J Laryngol Otol 113:458–463
Temple RH, Axon PR, Ramsden RT, Keles N, Deger K, Yucel E (1999) Auditory rehabilitation in neurofibromatosis type 2: a case of cochlea implantation. J Laryngol Otol 113:161–163
Xu HX, Joglekar SS, Paparella MM (2009) Labyrinthitis ossificans. Otol Neurotol 30(4):579–580
Roehm PC, Mallen-St Clair J, Jethanamest D, Golfinos JG, Shapiro W, Waltzman S, Roland JT Jr (2011) Auditory rehabilitation of patients with neurofibromatosis Type 2 by using cochlea implants. J Neurosurg 115(4):827–834
Carlson ML, Breen JT, Driscoll CL, Link MJ, Neff BA, Gifford RH, Beatty CW (2012) Cochlea implantation in patients with neurofibromatosis type 2: variables affecting auditory performance. Otol Neurotol 33(5):853–862
Caye-Thomasen P, Dethloff T, Hansen S, Stangerup SE, Thomsen J (2007) Hearing in patients with intracanalicular vestibular schwannomas. Audiol Neurootol 12(1):1–12
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beutner, C., Mathys, C., Turowski, B. et al. Cochlear obliteration after translabyrinthine vestibular schwannoma surgery. Eur Arch Otorhinolaryngol 272, 829–833 (2015). https://doi.org/10.1007/s00405-013-2877-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-013-2877-2