Abstract
Ototoxicity is a common side effect of cisplatin chemotherapy. This study was undertaken to determine the potential protective effects of a systemic administration of dexamethasone against cisplatin-induced ototoxicity. A prospective controlled trial conducted in an animal model. The setting was Animal care research facilities of the Montreal Children’s Hospital Research Institute. An experimental guinea pig model was used. The animals were divided as follows: group 1 (n = 10): 12 mg/kg intraperitoneal (IP) cisplatin, group 2 (n = 14): 15 mg/kg/day dexamethasone IP for 2 days followed by cisplatin 12 mg/kg IP, group 3 (n = 14): 10 mg/kg/day dexamethasone IP for 2 days, on day 3, they received cisplatin 12 mg/kg IP followed by 20 mg/kg/day dexamethasone for 2 days and group 4 (n = 5): 10 ml of saline IP twice a day for 3 days. Auditory brainstem response (ABR) threshold shifts were measured at four frequencies (8, 16, 20 and 25 kHz) for groups 1, 2 and 3. Histological changes in the organ of Corti, the stria vascularis, the spiral ligament and the spiral ganglion neurons as well as scanning electron microscopy for outer hair cells were completed. Immunohistochemistry for tumour necrosis factor-alpha (TNF-α) was performed. ABR threshold shifts were similar in all groups. Histological and scanning electron findings demonstrate that dexamethasone has greater protective effect on the stria vascularis. Systemic dexamethasone administration in a guinea pig model did not provide significant protection against cisplatin-induced ototoxicity. Dexamethasone may be useful in future applications as a complementary treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cisplatin is a widely used chemotherapeutic agent in pediatric and adult oncology protocols. Unfortunately, hearing loss is a major dose-limiting side effect presenting as a bilateral, irreversible and progressive sensorineural hearing loss leading to a decrease in quality of life of cancer patients [1]. In the inner ear, cisplatin targets the organ of Corti, the spiral ganglion neurons (SGNs), the stria vascularis and the spiral ligament [2, 3]. Once cisplatin enters the cell, it induces cell death mainly by apoptosis resulting from two main processes: oxidative stress and inflammation [4].
Cisplatin stimulates the inner ear local inflammatory response. Through the production of reactive oxygen species, cisplatin activates nuclear transcription factor-kappa B (NF-κB) which can regulate the expression of pro-inflammatory cytokines such as interleukin-1β (IL-1β), tumour necrosis factor-α (TNF-α) and interleukin-6 (IL-6) [4–6]. TNF-α can activate NF-κB, resulting in a positive feedback loop and increase the inflammatory response [7]. TNF-α also recruits inflammatory cells into the inner ear [8].
Glucocorticosteroids have a history of use for inner ear conditions and have been proven non toxic for the cochlear structures [9, 10]. Glucocorticosteroids inhibit mitogen-activated protein kinases, important regulators of pro-inflammatory transcription factors [11], by activating mitogen-activated protein kinase phosphatase-1 [12]. They can also induce nuclear factor of kappa light polypeptide gene enhancer in B-cells inhibitor alpha (IκB-α) expression which suppresses NF-κB inhibiting the inflammatory signaling cascade [13]. Transtympanic injections of glucocorticosteroids have been evaluated as potential treatment strategies for cisplatin-induced ototoxicity with variable degrees of protection [10, 14–16]. We hypothesized that the variability in the effectiveness of transtympanic dexamethasone might be caused, in part, by a variable degree of penetration of the dexamethasone reaching the inner ear from the middle ear space.
This led us to conduct the current study investigating the potential protective effect of a systemic administration of dexamethasone against the toxicity caused by cisplatin in the inner ear. This is the first publication, to our knowledge, addressing the systemic administration of dexamethasone for cisplatin-induced ototoxicity.
Materials and methods
Animals
Forty-three female albino Hartley guinea pigs weighing 500–800 g (Charles River Laboratory, Senneville, QC, Canada) were used in the current study. The animals had free access to water and food. The animals were kept in the animal care research facilities of the Montreal Children’s Hospital Research Institute under standard laboratory conditions; housed in a room at 20 ± 4 °C ambient temperature and a 12 h light/dark cycle. The study was approved and monitored by the Animal Care Committee in accordance with the Canadian Council of Animal Care guidelines.
Experimental design
The guinea pigs (43) were assigned to four groups: group 1 (n = 10) received 12 mg/kg of intraperitoneal (IP) cisplatin; group 2 (n = 14) received 12 mg/kg cisplatin IP followed by 15 mg/kg/day of dexamethasone IP for 3 days; group 3 (n = 14) received 10 mg/kg/day of dexamethasone IP for 2 days, on day 3, 12 mg/kg of cisplatin IP was administered followed by 20 mg/kg/day of dexamethasone IP for 3 days; group 4 (n = 5) received 10 ml of isotonic saline IP for 3 days. Dexamethasone injections for groups 2 and 3 were dissolved in saline, therefore the negative control group (group 4) received saline only and were employed as normal controls.
Since dexamethasone reaches a maximal concentration in perilymph 2 h following an IP injection [17], it was decided to administer cisplatin an hour and a half following the dexamethasone injections in order to obtain the greater concentrations of both products simultaneously in the inner ear.
The dosage of cisplatin has been determined by previous research at our laboratory [15]. It was demonstrated that this dose causes sufficient ototoxicity as a model yet very low mortality rates.
Cisplatin and dexamethasone treatment
Animals were anesthetized with isoflurane. The animals received 12 mg/kg of cisplatin IP under anesthesia. A subcutaneous bolus of 10 ml of sterile isotonic saline was injected following the cisplatin administration for hydration. Once treatment with cisplatin (1 mg/ml, Hospira, Canada) began, animals received two subcutaneous injections of sterile saline (10 ml) per day for hydration. The dexamethasone injections were prepared by dissolving the dexamethasone 21-phosphate disodium salt (Cat. No. D1159, Sigma-Aldrich Canada) in 0.9 % NaCl in order to obtain a concentration of 5 mg/ml. Animals were euthanized after 72 h following the cisplatin administration.
Auditory brainstem response
The auditory brainstem response (ABR) was performed prior to any injection (baseline measurement) and 72 h following the cisplatin IP administration (post measurement) in order to determine the ABR threshold shifts (SPL dB). Hearing threshold was defined as the lowest intensity of stimulation that resulted in a clear reproducible waveform. The tympanic membranes and external auditory canals were inspected prior to the ABR measurement using an operating microscope. Animals with preexisting hearing loss and/or any abnormality in the external or middle ear were excluded from the study. The active electrode was placed subcutaneously within the pinna of the tested ear, the reference electrode at the vertex and the ground electrode on the pinna of the contralateral pinna. The ABR was measured at four frequencies (8, 16, 20 and 25 kHz) on the Smart EP device (Intelligent Hearing Systems) using tone burst stimulus with a rate of 39.1 bursts/s and alternating polarity. The response to the stimulus was averaged from 1,600 sweeps. The measurements began at 80 dB and subsequently being decreased or increased by 20 dB and then 10 dB until the last three clear reproducible waveforms were obtained. Threshold shifts were calculated by comparing the pre- and post-cisplatin hearing threshold values. Two animals in group 3 died before completing the post measurement ABR.
Histological evaluation
Immediately following the post-ABR measurement, the animals were euthanized and the cochleae were dissected. The cochleae were fixed in 10 % neutral buffered formalin for 48 h at room temperature. Subsequently, decalcification was achieved by submerging the samples in 10 % EDTA at room temperature for 7 days with daily change of the solution. The specimens were then processed for an hour in 10 % neutral buffered formalin, next in 50 % alcohol and were maintained in 70 % alcohol until preparation for paraffin embedding. Once embedded in paraffin, the specimens were then mounted in order to obtain midmodiolar plane cuts. Sections of 5 μm of thickness were collected on glass slides and stained with haematoxylin and eosin staining. Sections were examined using a Zeiss Axiophot light microscope equipped with a Zeiss AxioCam MRc camera in which digitalized images were obtained.
Strial cross-sectional area
The strial cross-sectional area analysis was performed using the public domain NIH ImageJ program (U.S. National Institutes of Health; http://rsb.info.nih.gov/ij/). The periphery of the stria vascularis was delineated in every half turn of the cochlea in three segments: apex, middle and base and the cross-sectional area was determined (μm2) (Fig. 1). Six different measurements were made and averaged for every region. Subsequently, the areas from the groups were compared.
Spiral ganglion cell densities
Spiral ganglion cell densities were determined with the use of the NIH ImageJ program. Images of the cochleae (TIFF) were obtained, the boundaries of Rosenthal’s canal were outlined and the areas of the outlined spaces were calculated in mm2 (Fig. 1). The number of perikarya within the outlined spaces was counted and densities (number of perikarya/area in mm2) were determined as previously described [18].
Scanning electron microscopy
Cochlear samples were processed as previously described [19]. The samples were analyzed under a field emission scanning electron microscope (Hitachi S4700, Hitachi Ltd., Tokyo, Japan) in order to visualize and evaluate outer hair cell morphology.
Immunohistochemistry: TNF-alpha
Microtome sections were evaluated by immunohistochemical staining for the detection of TNF-α using a biotin-free detection system. Sections were deparaffinized with xylene and ethanol baths. Slides were then heated in a microwave oven with 0.01 M citrate buffer for 10 min followed by 3 % H2O2 in ethanol for 10 min at room temperature. Slides were washed three times with 0.1 M phosphate buffered saline (PBS) at pH 7.4 for 5 min and were then incubated overnight with the primary antibody at room temperature. Slides were washed with PBS for 15 min and then incubated with the enhancer reagent for 30 min at room temperature. After washing with PBS, slides were incubated with polymer–horseradish peroxidase for 45 min. After a final wash in PBS, slides were treated with diaminobenzidine to visualize the immunoreaction, counterstained with Mayer’s hematoxylin for 2 min, dehydrated in ethanol, cleared in xylene and mounted in Eukitt.
All slides were evaluated in a blinded fashion, without knowledge of the treatment administered. The expression of TNF-α was graded as faint, moderate or strong.
Statistical analysis
The data were analyzed using analysis of variance (one way ANOVA). Post hoc comparisons were made with Tukey’s multiple comparison test. Statistical significance was set at p value ≤0.05. Sample size for the experimental groups were calculated using the sample size calculator from the Department of Statistics of the University of British Columbia using the following criteria: power = 0.08, α = 0.05, σ = 15, μ1 = 0 and μ2 = 25 (http://www.stat.ubc.ca/~rollin/stats/ssize/n2.html).
Results
Auditory brainstem response
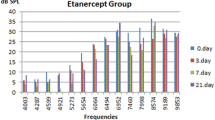
Intraperitoneal cisplatin administration caused a marked hearing loss. The average threshold shifts in the group receiving cisplatin only are 46 ± 9 dB at 8 kHz, 47 ± 7.1 dB at 16 kHz, 38 ± 4.3 dB at 20 kHz and 47 ± 4.4 dB at 25 kHz (Fig. 2). Therefore, a single injection of 12 mg/kg IP resulted in intense hearing loss throughout all of the frequencies tested.
Auditory brainstem response (ABR) threshold shifts in decibels (mean ± SEM) for cisplatin (CDDP) and CDDP + dexamethasone treated guinea pigs. ABR measurements were taken before and 72 h following the CDDP injection. No statistically significant difference was observed between the group receiving CDDP only and the groups receiving CDDP + dexamethasone. *p < 0.05
Guinea pigs receiving cisplatin and dexamethasone (group 2) also presented marked hearing loss with threshold shifts of 48 ± 5.4 dB at 8 kHz, 51 ± 4.8 dB at 16 kHz, 51 ± 3.7 dB at 20 kHz and 41 ± 4.3 dB at 25 kHz (Fig. 2). There was no otoprotection following this scheme of treatment.
Guinea pigs treated with dexamethasone in a greater dose (group 3) also demonstrated a marked hearing loss in the ABR measurements. The threshold shifts were 61 ± 16.5 dB at 8 kHz, 52 ± 10.2 dB at 16 kHz, 43 ± 9.5 dB at 20 kHz and 48 ± 9.1 dB at 25 kHz (Fig. 2). There was no otoprotection observed following a 2 day prophylaxis and a high dose dexamethasone treatment.
No statistically significant difference in ABR threshold shifts was observed between the groups (p > 0.05 for all frequencies tested). No significant otoprotection on ABR measurements was conferred by the use of systemic dexamethasone on cisplatin-induced ototoxicity.
Light microscopy examination
Light microscopy of cochlear samples was performed in order to obtain general histological characteristics. Cochlear samples obtained from animals receiving only cisplatin demonstrated partial loss of outer hair cells (OHCs) with collapse of the tunnel of Corti and Nuel’s space. The lateral wall findings consisted of protrusion of marginal cells into the endolymphatic space as well as strial edema. SGNs displayed partial detachment of the myelin sheath (Fig. 3b). These results were observed in the three cochlear segments (apex, middle, base). A very slight detachment was also observed in animals receiving saline only (Fig. 3a).
Sections of cochlear samples: base of cochlea: a saline (negative control), b cisplatin (positive control), c cisplatin + dexamethasone (group 2) and d cisplatin + greater dose of dexamethasone (group 3). Hematoxylin and eosin stain. Collapse of the tunnel of Corti and Nuel’s space is observed in cisplatin-treated animals as well as protrusion of marginal cells into the perilymphatic space and strial edema. Similar changes are visible in c
Samples obtained from animals receiving cisplatin and dexamethasone (group 2) revealed disruption of the microarchitecture of the organ of Corti similar to the samples obtained from the animals receiving cisplatin only (Fig. 3c). The lateral wall and SGN findings were also similar. On the other hand, animals treated with cisplatin and a greater dose of dexamethasone (group 3) exhibited preserved morphology of the tunnel of Corti and Nuel’s space (Fig. 3d). Also, strial edema was decreased as compared to the cisplatin animal samples (Fig. 4). However, the SGN myelin sheath detachment findings did not differ from the animals receiving cisplatin only.
Strial cross sections. a Saline (negative control), b cisplatin (positive control), c cisplatin + dexamethasone (group 2) and d cisplatin + greater dose of dexamethasone (group 3). Hematoxylin and eosin stain. Greatest strial edema and increased cross-sectional areas were observed in cisplatin-treated animals (b)
Strial cross-sectional area
The strial cross-sectional areas were calculated for all of the groups. Saline-treated animal samples were used to establish the area of the half sections for the apex, middle and base segments of the cochlea in normal guinea pigs. The cross sections observed in the saline-treated group demonstrated dense striae and clearly defined nuclei with no bulging of cells into the endolymphatic space (Fig. 4a).
The cross sections pertaining to the animals treated only with cisplatin revealed decreased strial density, increased cellular vacuolization (Fig. 4b) and greater cross-sectional areas as compared to the saline-treated animals (Fig. 5).
Cross-sectional area (μm2) of the apex, middle and base of the cochleae. Measurements for the right and left cochleae were averaged. Six different measurements were assessed for every segment of every cochlea in order to increase the precision of the measurements. The cisplatin (CDDP)-treated group demonstrated the greatest areas. No statistically significant difference was observed between CDDP-treated animals and animals receiving CDDP and dexamethasone in low or high dosage (Dex.)
The areas calculated for samples obtained from the animals treated with cisplatin and dexamethasone (group 2) were greater compared to the saline-treated group and slightly lower compared to the cisplatin-treated group (Fig. 5); the striae were denser and exhibited less vacuolization (Fig. 4c). Samples from group 3 also demonstrated reduced areas as compared to the cisplatin-treated group, yet no statistically significant difference was observed. We can appreciate dense striae, minimal bulging into the endolymph and a rather conserved morphology (Fig. 4d). No statistically significant difference was detected between the groups in terms of strial areas (p > 0.05 for all segments of the cochlea).
Spiral ganglion neuron densities
SGN densities were calculated for all groups. No statistically significant difference was detected between the groups in terms of SGN densities (p > 0.05) (Fig. 6).
Spiral ganglion cell densities. The control group consisted of the saline-treated animals. Treatment with cisplatin (CDDP) did not significantly decrease the SGN densities as compared to the control group. No statistically significant difference was observed between any of the groups and for any segment of the cochlea. *p < 0.05
Scanning electron microscopy
Animals receiving saline did not present with OHC loss or irregularities of stereocilia (Fig. 7a). Damage and loss of stereocilia as well as rupture of the cuticular plate were clearly visible in cisplatin-treated animals (Fig. 7b) and in animals receiving cisplatin and the lower dose of dexamethasone (Fig. 7c). Greater preservation of OHCs was detected in the group receiving cisplatin and the greater dose of dexamethasone (Fig. 7d).
Scanning electron microscopy of outer hair cells (OHCs). a Saline b cisplatin, c cisplatin + lower dose of dexamethasone (group 2) and d cisplatin + greater dose of dexamethasone (group 3). Greater loss of OHCs is observed in b and c. Animals receiving saline did not present with OHC loss. Some OHC loss was detected in d
Immunohistochemistry
Immunohistochemical detection of TNF-α in the normal cochlea was faint; the OHCs, stria vascularis, spiral ligament and SGNs stained weakly (Fig. 8a), whereas strong immunostaining was observed in the cisplatin-treated animal samples for the above mentioned cochlear areas (Fig. 8b). Strong immunostaining was also observed for the samples obtained from group 2 (Fig. 8c). Most interesting was the staining observed for the last group, receiving cisplatin and the greater dose of dexamethasone (group 3). Here, moderate immunostaining was observed (Fig. 8d).
TNF-α immunoexpression in cochlear samples: a saline, b cisplatin, c cisplatin + lower dose of dexamethasone (group 2) and d cisplatin + greater dose of dexamethasone (group 3). Counterstained with Mayer’s haematoxylin. Strong immunostaining is observed in b and c, moderate immunostaining is observed in d and very faint immunostaining is observed in a
Discussion
Cisplatin is a commonly used chemotherapeutic agent. It has potent antineoplastic activity and can cause important adverse effects such as nephrotoxicity, ototoxicity and neurotoxicity which limit its clinical use [20]. Cisplatin ototoxicity leads to a bilateral and irreversible sensorineural hearing loss that is progressive from higher to the lower frequencies [1]. It quickly binds DNA and proteins and thereby inhibits their functions. Once bound, cisplatin induces the generation of reactive oxygen species and initiates the inflammatory cascade. These events can lead to apoptosis and therefore to a decrease in the number of cells in the cochlea necessary for an adequate function of the inner ear [4].
To date, the literature on transtympanic administration of dexamethasone against cisplatin-induced ototoxicity presents different magnitudes of protective effects. Hill et al. [10], Daldal et al. [14] and Murphy et al. [15] previously reported that intratympanic dexamethasone injections may provide some protection against cisplatin-induced ototoxicity in a mouse [10] and guinea pig model, respectively [14, 15]. Paksoy et al. [16] observed a significant protective effect from intratympanic dexamethasone injections in a rat model with decreased threshold shifts on ABR testing. The previously mentioned studies only reported hearing test results (ABR or distortion product otoacoustic emissions) as evidence. A transtympanic administration can avoid systemic side effects, nevertheless the technique can cause local complications [21]. Also, concentrations reached in cochlear fluids are unpredictable [22]. To our knowledge, no previous study has evaluated the protective effect of a systemic administration of glucocorticosteroids on cisplatin-induced ototoxicity. It has been demonstrated that an intraabdominal or intratympanic injection of dexamethasone provides similar concentrations in perilymph in 30 min [17]. A systematic approach is the easiest route of administration and is easily controlled. In addition, dexamethasone does not interfere with the cytotoxic action of cisplatin [23], a frequently cited concern.
In our study, ABR outcomes did not demonstrate a functional protection from dexamethasone on cisplatin-induced ototoxicity. No difference was detected comparing animals treated with cisplatin alone or with cisplatin and dexamethasone. All experimental animals presented significant hearing loss at all frequencies tested (Fig. 2).
Cisplatin is known to target the organ of Corti, the OHCs, the SGNs, the stria vascularis and the spiral ligament [2, 3]. Morphological alterations were observed following cisplatin administration. Partial loss of OHCs with collapse of the tunnel of Corti and Nuel’s space, protrusion of marginal cells into the endolymphatic space, strial edema as well as partial detachment of the myelin sheath of SGN were observed. Similar findings have been previously reported [3, 18, 24]. OHC loss was further demonstrated with scanning electron microscopy which allowed detection of missing OHCs as well as rupture of the cuticular plates. A high dose of dexamethasone preserved the morphology of the tunnel of Corti, Nuel’s space and the stria vascularis and decreased the strial edema.
Various authors [3, 24–27] have aimed to assess the histological pattern of injury to the stria vascularis caused by cisplatin. We observed decreased strial density, increased cellular vacuolization and increased cross-sectional areas in cisplatin-treated animals. The cross-sectional area measurements coincide with previous studies [24, 25]. The group that received the highest dose of dexamethasone in addition to cisplatin demonstrated similar area measurements to the saline-treated group (Fig. 5). Statistical analysis of the strial measurements are limited by the number of animals in each group seen as cochleae that did not meet histological criteria were discarded, i.e., section not in midmodiolar plane, broken cochleae from dissection. We can observe a tendency but further studies with a greater number of animals are required.
The reason for greater morphological preservation of the stria vascularis is unclear. Glucocorticosteroid receptors are highly expressed in the spiral ligament, stria vascularis and OHCs [28, 29]. Yet, our results demonstrate the lack of protection from dexamethasone on OHCs. Dexamethasone has also been shown to increase cochlear blood flow [9]. It may be that since the stria vascularis is highly vascularised and that cochlear blood flow is increased, the quantity of dexamethasone reaching the lateral wall may be greater as compared to other areas of the cochlea.
The SGNs displayed partial detachment of the myelin sheath when exposed to cisplatin. Findings did not differ from the animals receiving cisplatin and dexamethasone at any dosage. As for SGN densities, no statistically significant difference was detected between the groups. As previously reported, our results also suggest that cisplatin administration may not result in SGN loss (12 mg/kg IP) [18].
TNF-α has been shown to be a key pro-inflammatory cytokine in cisplatin-induced ototoxicity [6]. Immunohistochemistry for TNF-α was performed in order to detect whether dexamethasone administration decreases the expression of this cytokine. Cisplatin administration led to a strong immunoexpression of TNF-α in OHCs, the stria vascularis, the spiral ligament and in SGNs. Concomitant administration of dexamethasone in a high dose provided only a slight reduction in staining. It seems that the inflammatory component of cisplatin-induced ototoxicity may play a small role in the pathophysiology, given that when administering a high dose of dexamethasone, cochlear morphological and functional alterations are still observed. A limitation of the study is the lack of long-term follow-up. The guinea pig model used allows post-ABR testing to be performed on day 3, a situation not occurring in a clinical setting. Further studies employing different animal models allowing for long-term treatment and follow-up would be required.
Conclusion
We studied the protective effect of a systemic dexamethasone administration against cisplatin-induced ototoxicity in a guinea pig model. We did not observe significant protection against cisplatin-induced ototoxicity. Dexamethasone seems to decrease TNF-α expression slightly as well as protect the stria vascularis from morphological alterations. Dexamethasone may be useful in future applications as a complementary treatment for cisplatin-induced ototoxicity.
References
Rybak LP, Ramkumar V (2007) Ototoxicity. Kidney Int 72:931–935
Watanabe K, Inai S, Jinnouchi K, Baba S, Yagi T (2003) Expression of caspase-activated deoxyribonuclease (CAD) and caspase 3 (CPP32) in the cochlea of cisplatin (CDDP)-treated guinea pigs. Auris Nasus Larynx 30:219–225
van Ruijven MW, de Groot JC, Klis SF, Smoorenburg GF (2005) The cochlear targets of cisplatin: an electrophysiological and morphological time-sequence study. Hear Res 205:241–248
Rybak LP, Whitworth CA, Mukherjea D, Ramkumar V (2007) Mechanisms of cisplatin-induced ototoxicity and prevention. Hear Res 226:157–167
Rybak LP (2007) Mechanisms of cisplatin ototoxicity and progress in otoprotection. Curr Opin Otolaryngol Head Neck Surg 15:364–369
So H, Kim H, Lee JH, Park C, Kim Y, Kim E, Kim JK, Yun KJ, Lee KM, Lee HY, Moon SK, Lim DJ, Park R (2007) Cisplatin cytotoxicity of auditory cells requires secretions of proinflammatory cytokines via activation of ERK and NF-kappaB. J Assoc Res Otolaryngol 8:338–355
Barnes PJ (1997) Nuclear factor-kappa B. Int J Biochem Cell Biol 29:867–870
Keithley EM, Wang X, Barkdull GC (2008) Tumor necrosis factor alpha can induce recruitment of inflammatory cells to the cochlea. Otol Neurotol 29:854–859
Shirwany NA, Seidman MD, Tang W (1998) Effect of transtympanic injection of steroids on cochlear blood flow, auditory sensitivity, and histology in the guinea pig. Am J Otol 19:230–235
Hill GW, Morest DK, Parham K (2008) Cisplatin-induced ototoxicity: effect of intratympanic dexamethasone injections. Otol Neurotol 29:1005–1011
Barnes PJ (2005) Molecular mechanisms and cellular effects of glucocorticosteroids. Immunol Allergy Clin North Am 25:451–468
Wang D, Lippard SJ (2005) Cellular processing of platinum anticancer drugs. Nat Rev Drug Discov 4:307–320
Auphan N, DiDonato JA, Rosette C, Helmberg A, Karin M (1995) Immunosuppression by glucocorticoids: inhibition of NF-kappa B activity through induction of I kappa B synthesis. Science 270:286–290
Daldal A, Odabasi O, Serbetcioglu B (2007) The protective effect of intratympanic dexamethasone on cisplatin-induced ototoxicity in guinea pigs. Otolaryngol Head Neck Surg 137:747–752
Murphy D, Daniel SJ (2011) Intratympanic dexamethasone to prevent cisplatin ototoxicity: a guinea pig model. Otolaryngol Head Neck Surg 145:452–457
Paksoy M, Ayduran E, Sanlı A, Eken M, Aydın S, Oktay ZA (2011) The protective effects of intratympanic dexamethasone and vitamin E on cisplatin-induced ototoxicity are demonstrated in rats. Med Oncol 28:615–621
Liu HJ, Dong MM, Chi FL (2006) Dexamethasone pharmacokinetics in Guinea pig inner ear perilymph. ORL J Otorhinolaryngol Relat Spec 68:93–98
van Ruijven MW, de Groot JC, Smoorenburg GF (2004) Time sequence of degeneration pattern in the guinea pig cochlea during cisplatin administration. A quantitative histological study. Hear Res 197:44–54
Waissbluth S, Dupuis I, Daniel SJ (2011) Protective effect of erdosteine against cisplatin-induced ototoxicity in a guinea pig model. Otolaryngol Head Neck Surg 146:627–632
Hartmann JT, Lipp HP (2003) Toxicity of platinum compounds. Expert Opin Pharmacother 4:889–901
Rutt AL, Hawkshaw MJ, Sataloff RT (2011) Incidence of tympanic membrane perforation after intratympanic steroid treatment through myringotomy tubes. Ear Nose Throat J 90:E21
Banerjee A, Parnes LS (2004) The biology of intratympanic drug administration and pharmacodynamics of round window drug absorption. Otolaryngol Clin North Am 37:1035–1051
Wagenblast J, Arnoldner C, Gstöttner W, Bisdas S, Mörtel S, May A, Hambek M (2010) Does dexamethasone inhibit the antineoplastic effect of cisplatin and docetaxel in head and neck cancer cells? Anticancer Res 30:123–127
Meech RP, Campbell KC, Hughes LP, Rybak LP (1998) A semiquantitative analysis of the effects of cisplatin on the rat stria vascularis. Hear Res 124:44–59
Sluyter S, Klis SF, de Groot JC, Smoorenburg GF (2003) Alterations in the stria vascularis in relation to cisplatin ototoxicity and recovery. Hear Res 185:49–56
Kohn S, Fradis M, Podoshin L, Ben David Y, Zidan J, Robinson E, Nir I (1991) Toxic effects of cisplatin alone and in combination with gentamicin in stria vascularis of guinea pigs. Laryngoscope 101:709–716
Tange RA, Vuzevski VD (1984) Changes in the stria vascularis of the guinea pig due to cis-platinum. Arch Otorhinolaryngol 239:41–47
Rarey KE, Curtis LM, ten Cate WJ (1993) Tissue specific levels of glucocorticoid receptor within the rat inner ear. Hear Res 64:205–210
ten Cate WJ, Curtis LM, Small GM, Rarey KE (1993) Localization of glucocorticoid receptors and glucocorticoid receptor mRNAs in the rat cochlea. Laryngoscope 103:865–871
Acknowledgments
The authors wish to thank Rujuan Huo from the Centre for Bone and Periodontal Research for their invaluable technical assistance.
Conflict of interest
The authors do not have any conflict of interest for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Waissbluth, S., Salehi, P., He, X. et al. Systemic dexamethasone for the prevention of cisplatin-induced ototoxicity. Eur Arch Otorhinolaryngol 270, 1597–1605 (2013). https://doi.org/10.1007/s00405-012-2150-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-012-2150-0