Abstract
Utricular dysfunction has been indirectly measured with subjective visual horizontal or vertical testing. Video-oculography equipment with integrated head position sensor allows direct evaluation of head tilt. The aim was to assess head tilt after peripheral vestibular lesion by recording tilting of the head after excluding visual cues (static test condition), and after three lateral head tilts to both sides [subjective head vertical (SHV)]. Thirty patients with unilateral, peripheral vestibular loss were measured in the acute state, and 3 months later. Twenty healthy, age- and sex-matched subjects served as controls. Mean static tilt of 2.6 ± 1.1° in patients with acute vestibular loss differed significantly from that of 1.0 ± 0.4° in healthy subjects (p = 0.004), and from that of 1.1 ± 0.5° during the follow-up visit (p = 0.008). The mean SHV of 3.4 ± 0.7° in patients with acute vestibular loss was significantly more than that of 1.2 ± 0.5° in controls (p < 0.001). The SHV towards the lesion was 4.9 ± 1.0° while returning from the lesion side and 2.0 ± 1.0° while returning from the healthy side. The SHV was definitely abnormal in 60%, moderately abnormal in 20% and normal in 20% of the patients in acute state. Abnormal SHV persisted in only 20% of the patients indicating that recovery of the peripheral utricular function is occurring within months. In summary, head tilts slightly towards acute peripheral lesion, and this tilting is reinforced, when the head is actively moved on the lesion side.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Utricles sense linear acceleration in mainly horizontal plane. Unilateral loss of utricular function causes ocular tilt reaction consisted of head tilt, skew deviation, and eye torsion towards the lesion. [1]. Asymmetry in utricular function has been quantified with subjective visual horizontal (SVH) or subjective visual vertical (SVV) testing [2, 3]. In these tests, a healthy subject can typically align illuminated bar within two degrees of true earth horizontal or vertical in total darkness. Instead, acute unilateral peripheral vestibular loss causes a moderate tilt of visual surroundings towards the affected side. This tilt of visual surroundings in SVH and SVV has been shown to concur closely with eye torsion, which is initiated by asymmetry of utricular input in the level of vestibular nuclei [4].
Video-oculography (VOG) has increasingly replaced other techniques in eye movement recordings during the last decade [5, 6]. In addition to eye movement recording, the position of the head may be monitored directly during VOG recordings via sensor attached to the mask worn by the patient. This continuous head position information allows a novel technique to evaluate the head tilt as a part of the VOG recording.
In the present study, we wanted to assess directly possible head tilt after vestibular lesion by recording tilting of the head in primary central position after excluding visual cues (static test condition), and after lateral head tilts (dynamic test condition) using a commercially available VOG. We aimed also to quantify possible asymmetry in tilt, and if head tilt correlates with other vestibular signs and symptoms.
Subjects and methods
Patients
Thirty patients with acute unilateral vestibular loss (17 right-sided and 13 left-sided) were included. The patients did not have any chronic otoneurological diseases or medications in their history. There were 12 men and 18 women with a mean age of 48 (range 14–71) years. The patients were admitted to inpatient ward of tertiary referral center due to strong vertigo. Most patients were measured within a mean of 3 days (range 1–9) after the onset of symptoms. The diagnosis of vestibular neuritis was based on clinical history and findings with typical peripheral nystagmus without any central findings. Most suffered from vestibular symptoms only, although additional hearing loss (neurolabyrinthitis) or facial nerve dysfunction (Ramsay-Hunt syndrome) was encountered in nine patients. Negative brain imaging with CT or MRI was performed in majority of the patients either acutely or during follow-up period to rule out other causes. Clinical follow-up visit with a control test was scheduled on average 3 months later.
Twenty healthy subjects without any otoneurological diseases or medications were measured as controls. Their mean age of 43 (range 27–62) years and sex distribution of 8 males and 12 females did not differ significantly from the patient group.
The ethics committee of the Helsinki University Hospital approved the study, and each patient gave a written informed consent.
Equipment and measurement
We recorded head position with a mask-mounted head position sensor in a dimly lighted room (The 3-D VOG, Version 5, Sensomotoric Instruments, Berlin, Germany).
The patients were prone and head straight ahead. Head position was recorded in same order for each patient: the patients were informed to keep their heads as straight as possible in a dimly lighted test room with eyes uncovered. Next, the subjects were instructed to maintain their head position while the eyes were covered using usual VOG mask cover. Possible tilting of the head after exclusion of visual cues was monitored during following 30 s interval (static tilt).
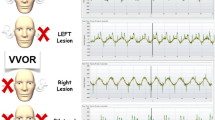
Dynamic part of the recording included three lateral tilts of the head (30–40°) towards each shoulder for approximately 15 s, and thereafter, the patients were instructed to return to head straight position for approximately 15 s. The angle of head tilt after return to assumed straight head position called SHV was measured at the end of the each position. The mean deviation from the midline of three returns was calculated for each side, and as a mean for both sides.
Subjective sensation
Subjective assessment of severity of dizziness, and quality of life was performed in five grade scale.
Statistics
We used SPSS v. 17.0 software (SPSS Inc., Chicago, IL, USA), and p value of <0.05 was considered statistically significant. The non-paired t test was applied to compare the groups, and the Spearman correlation test was used for correlations between subjective sensations and signs in vestibular tests. Data are expressed as mean ± 95% confidence interval.
Results
Static tilt of the head in controls was on average 1.0 ± 0.4°. Mean static tilt of 2.6 ± 1.1° in patients with acute vestibular loss differed significantly from that of healthy subjects (p = 0.004), and from their own control measurement of 1.1 ± 0.5° during the follow-up visit (p = 0.008). Static tilt was definitely abnormal in 37% (3° or more), moderately abnormal in 23% (2–3°), and normal (<2°) in 40% of the patients.
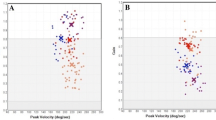
The mean SHV in patients with acute vestibular loss of 3.4 ± 0.7° towards lesion side was significantly more than the mean tilt in controls of 1.2 ± 0.5° (p < 0.001) (Fig. 1). The SHV while returning from the lesion side was incomplete with a mean of 4.9 ± 1.0°, and the head tilted towards lesion side even while returning from the healthy side for 2.0 ± 1.0°. In 80% of the patients, the SHV was greater while moving on the lesion side. Until the follow-up visit, the SHV had recovered to 1.7 ± 0.7° (Fig. 1) (p = 0.23).
Mean subjective head vertical angles ± confidence intervals in patients with acute state (black square), during follow-up visit (open square), and in controls (black triangle). The SHV in patients with acute state was significantly larger than that of during follow-up visit and to that of controls (p < 0.001 for both comparisons).The SHV did not differ significantly between the patients during follow-up visit and the controls (p = 0.23)
The SHV was definitely abnormal in 60% of the patients in acute state, moderately abnormal in 20% and normal in 20% of the patients. No patients had a head tilt towards the healthy side. After follow-up period of some months, abnormal SHV was seen in only 20% of the patients.
Subjective sensation of dizziness decreased significantly from 3.1 ± 0.4 to 1.4 ± 0.4 during follow-up period (p < 0.001). Quality of life score of 3.8 ± 0.6 improved significantly to 1.7 ± 0.5 (p < 0.001).
There was no association between the head tilt and subjective sensations. Head tilt correlated significantly with asymmetry in gain of horizontal semicircular canal (r = 0.87, p < 0.0001), and slow-phase velocity of the spontaneous nystagmus (r = 0.85, p < 0.0001) in patients with the acute vestibular loss.
Discussion
The amount of head tilt after unilateral, peripheral vestibular lesion can easily be assessed using standard three-dimensional VOG—equipment with an integrated head position sensor. The head deviates slightly toward the side of the lesion when visual input is blocked. This asymmetric head tilt is strengthened when the head is actively leaned to the lesion side and back. In the acute state, the head movements on the healthy side are better controlled, although a mild head tilt towards the lesion side can still be revealed. Significant head tilt could be detected in 80% of the patients in acute state, but in only 20% of the patients some months after the lesion indicating that recovery of the peripheral utricular function is occurring within months for most of the patients.
Ocular torsion correlates with perceived visual horizontal after unilateral vestibular loss [4]. However, measurement of eye torsion is complicated due to small and variable gain of torsional eye movements. Prominent head tilts are the common finding in rodents after unilateral vestibular lesion [7]. On the contrary, head-based graviceptive signals provide predominant input for visual vertical in man, which explains that the head tilt after even total unilateral vestibular loss may be difficult to notice with inspection only in patients [8]. Simple and sensitive tools as used in the present study to reveal even minor head tilt should therefore be appreciated by clinicians [9].
Subjective head horizontal tilting seems to be well comparable to the subjective visual horizontal/vertical values presented after acute unilateral vestibular loss. Depending on the study design, the tilt of subjective visual has varied from 2 to 10°, and the recovery has been fast for most of the patients [2, 3, 10, 11]. The etiology, time interval from the beginning, grade of the disease, patient population, and the exact method used affect the results. For example, the SVH at 1 month declines to half of that at 1 week [4]. In the present study, the patients with more severe loss of semicircular canal function showed more head tilt than those with better function, and SVH normalized during the follow-up period in most of the patients. In the clinical setting, the SHV as employed in present study may be easily added to standard VOG test pattern. It does not require any extra, complex device to be used for otolith examination.
Directional asymmetry in tilt responses has been detected earlier by Bergenius et al. [12], who examined subjective visual horizontal in unilateral vestibular loss patients while tilted in chair. Their patients corrected the tilt angle more insufficiently, when tilted on the diseased side, and this feature prevailed for months in some patients. Our findings of worse SHV after moving on the lesion side agree with these findings indicating that the utricle on the side of the tilt is predominant in sensing the gravity. During head tilt neural population on one side of the striola is excited, and the other is inhibited. The response from each utricle is directionally asymmetric due to uneven amount of hair cells on different sides of the striola. As the total neural input from lesion side is weaker, the utricle from the healthy side drives the eyes and head towards the lesion side.
In conclusion, utricular function displayed as head tilt may be evaluated using commercial VOG with integrated head position sensor. Acute peripheral loss of vestibular function causes often a mild head tilt towards the lesion, and in addition, head motion on the lesion side further aggravates this inaccuracy of sensing gravitation.
References
Halmagyi GM, Gresty MA, Gibson WPR (1979) Ocular tilt reaction with peripheral vestibular lesion. Ann Neurol 6:80–83
Tabak S, Collewijn H, Boumans LJ (1997) Deviation of the subjective vertical in long-standing unilateral vestibular loss. Acta Otolaryngol 117:1–6
Min KK, Ha JS, Kim MJ, Cho CH, Cha HE, Lee JH (2007) Clinical use of subjective visual horizontal and vertical in patients of unilateral vestibular neuritis. Otol Neurotol 28:520–525
Curthoys IS, Dai MJ, Halmagyi GM (1991) Human ocular torsional position before and after unilateral vestibular neurectomy. Exp Brain Res 85:218–225
Schworm HD, Ygge J, Pansell T, Lennerstrand G (2002) Assessment of ocular counterroll during head tilt using binocular video oculography. Invest Ophthalmol Vis Sci 43:662–667
Zingler VC, Kryvoshey D, Schneider E, Glasauer S, Brandt T, Strupp M (2006) A clinical test of otolith function: static ocular counterroll with passive head tilt. Neuroreport 17:611–615
Hirvonen TP, Minor LB, Hullar TE, Carey JP (2005) Effects of intratympanic gentamicin on vestibular afferents and hair cells in the chinchilla. J Neurophysiol 93:643–655
Tarnutzer AA, Bockisch CJ, Straumann D (2010) Roll-dependent modulation of the subjective visual vertical: contributions of head- and trunk-based signals. J Neurophysiol 103:934–941
Zwergal A, Rettinger N, Frenzel C, Dieterich M, Brandt T, Strupp M (2009) A bucket of static vestibular function. Neurology 72:1689–1692
Choi KD, Oh SY, Kim HJ, Koo JW, Cho BM, Kim JS (2007) Recovery of vestibular imbalances after vestibular neuritis. Laryngoscope 117:1307–1312
Kim HA, Hong JH, Lee H, Yi HA, Lee SR, Lee SY, Jang BC, Ahn BH, Baloh RW (2008) Otolith dysfunction in vestibular neuritis: recovery pattern and a predictor of symptom recovery. Neurology 70:449–453
Bergenius J, Tribukait A, Brantberg K (1996) The subjective horizontal at different angles of roll-tilt in patients with unilateral vestibular impairment. Brain Res Bull 40:385–390
Acknowledgments
The study was supported by research grants from Helsinki University Central Hospital.
Conflict of interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hirvonen, T.P., Jutila, T. & Aalto, H. Subjective head vertical test reveals subtle head tilt in unilateral peripheral vestibular loss. Eur Arch Otorhinolaryngol 268, 1523–1526 (2011). https://doi.org/10.1007/s00405-011-1560-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-011-1560-8