Abstract
Laryngeal cancer is the second most common cancer of the respiratory tract with a relative 5-year survival over all tumour sites in the USA (61.6%; SEER 2009), which is much better than other head and neck cancers. The aim of this paper is to review and summarise data on the survival of laryngeal cancer patients. Literature search was conducted to identify articles in PubMed up to June 2009. Thirty studies with different study aims including sufficient information on survival of laryngeal cancer patients were identified. The 5-year overall survival ranged from 0 to 100%, depending on the T- and N-category, therapeutic approach and tumour location. The involvement of other factors such as genetics, nutrition and lifestyle habits remains uncertain. Our meta-analysis on a subgroup of published studies yielded an overall 5-year relative survival rate of 64.2% (95% confidence interval 63.7–64.7%). Different study aims and patient selection criteria prohibit general conclusions. However, this review may provide an actual picture of the complexity of factors influencing the survival of laryngeal cancer patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head and neck squamous cell carcinoma (HNSCC) includes cancer of the nasal cavity, paranasal sinuses, oral cavity, nasopharynx, oropharynx, hypopharynx and larynx. Laryngeal cancer is the second most common cancer of the respiratory tract with an estimated incidence rate of 5.1/100,000 cases in males worldwide in the year 2008 and a European incidence rate of 10/100,000. The age-standardised mortality (world standard) in laryngeal cancer for males is 2.2/100,000 [1].
The major risk factors for laryngeal cancer are tobacco smoking and alcohol consumption, as has been consistently demonstrated by a variety of epidemiological studies [2–4]. There is a dose–response relationship for tobacco consumption for all laryngeal tumour sites, which is higher for supraglottic than for glottic and subglottic tumours. For glottic and subglottic tumour sites, there is an increased risk in light and heavy smokers, and for supraglottic tumours in heavy smokers only [2]. The risk decreases with increasing time since quitting smoking [5]. In terms of passive smoking, the available studies do not allow a clear conclusion [6]. However, a recent publication highlighted the effect of involuntary smoking [7], as was also found in head and neck cancer patients [8]. The effect of alcohol consumption is not as strong as that of smoking, although an increased risk has been observed with increase in alcohol intake. Differences have also been observed with regard to tumour site, i.e. a higher risk for supraglottic than for glottic and subglottic tumours [2]. Additionally, an interaction effect between tobacco and alcohol consumption on the risk of laryngeal cancer has been observed, inducing a sub-multiplicative but more than additive effect of the joint consumption of tobacco and alcohol [2, 5]. There are also occupational risk factors for which there is some evidence of a link to laryngeal cancer. These include exposure to asbestos, polycyclic aromatic hydrocarbons, dust and solvents [3, 9–12].
In the USA, the relative 5-year survival of patients with laryngeal cancer is 61.6%. Thus, it has a better 5-year overall survival rate than oropharyngeal (39.2%), hypopharyngeal (29.2%) or oesophageal cancer (16.8%) [13]. According to recent research, the overall survival in patients with laryngeal cancer as with any other head and neck cancer has not increased remarkably, despite advanced surgical techniques, new chemotherapeutic drugs and improvements in radiotherapy within the last 30 years. A recent analysis by the EUROCARE-4 working group analysed about 3 million adult cancer cases from 82 cancer registries in 23 European countries, diagnosed in 1995–1999 and followed to December 2003 [14]. The overall survival for laryngeal cancer was 63%, with the highest in the Netherlands and Malta (75%) and lowest in Portugal and Poland (around 47%). The question that arises here is, whether certain treatment approaches, such as that in the Netherlands, where T1–T3 tumours are primarily treated with radiotherapy using salvage surgery only in case of failure, are responsible for the high survival rates [14]. However, Pfister et al. [15] stated that the different treatment approaches (transoral laser surgery (TLS), open partial resection or total laryngectomy, primary or adjuvant radio- and/or chemotherapy) do not appear to affect the survival outcomes of patients. Moreover, while minimal invasive surgery improves the quality of life, toxic substances may also affect it [16, 17]. In addition, severe comorbidity (e.g. cardiovascular disease) seems to be a predictor for shorter survival times of laryngeal cancer patients [18–21].
Tumour site (glottic, supraglottic and subglottic) and staging determine the treatment modality and influence survival rates. For example, for patients with T1 or T2 laryngeal cancer, the American Society of Clinical Oncology (ASCO) recommends in its clinical practice guidelines an initial treatment that preserves the larynx [15]. For most patients with T3 or T4 disease without tumour invasion through the cartilage into soft tissues, a larynx preservation approach is regarded as an appropriate treatment option, and concurrent chemoradiation therapy is a useful approach. Newer publications reflect the increase of late toxicity after platin-based concurrent chemoradiation and discuss the use of induction therapy as part of sequential concepts conducted in clinical trials [22–26]. However, at advanced tumour stages, laryngectomy is often the only possible option. On the other hand, a recent article by Lefebvre et al. [25] concluded that it was impossible to give general therapy recommendations: the selected therapy approach should involve a combination of a treatment guideline and a careful patient management process.
The National Cancer Institute differentiates between localised cancer (no cancer spread, locally restricted), regional cancer (lymph node and tissue spread next to the primary tumour) and distant cancer (tumour spread to several organs and lymph node). In the year 1999, the 5- and 10-year survival rates for patients with laryngeal cancer in the US population were: 82 and 69% (localised cancer), 48 and 34% (regional cancer) and 28 and 18% (distant cancer), respectively. Tumour staging is expressed in the TNM-classification system in more detail, where T1–4 stands for the size of the tumour, N1–3 describes the involvement of the lymph nodes and M0 and M1 indicate the distant cancer spread. The resulting 24 TNM categories are grouped into four TNM stages, I–IV [27].
Recently, both tobacco and alcohol consumption have been reported to reduce the survival rates of head and neck cancer patients [28]. However, it is currently unknown to what extent other factors influence the survival times of laryngeal cancer patients.
Materials and methods
Relevant studies were identified by searching the PubMed database for articles published until June 2009. To consider only current treatment strategies, studies published before 1995 were not considered for this review. The following terms were used in various combinations: “laryngeal cancer” and “larynx survival”. Amongst the large number of studies identified, only those articles in which the title or the abstract provided hints about survival rates in humans were taken into detailed consideration. Articles considered as a result of the literature search for this review fulfilled the following criteria:
-
Publication language: English.
-
Only full-text articles were included, as abstracts did not provide sufficient information for more detailed evaluation.
-
Only studies with squamous cell carcinoma (SCC) were included.
The studies complying with the inclusion criteria were grouped by the following criteria: geographic area, comorbidities, quality of life, co-malignancies, laser surgery, conventional surgery, radiotherapy and combination of therapies.
Where available, details regarding the study population, study design and survival rates were extracted from the articles. The stage and location of neoplastic lesions were taken into account. Whenever patients in the individual studies had been excluded for the final analyses, only the numbers of relevant laryngeal cancer patients who had been used for the estimation of survival rates were reported in the “Results”.
Statistical methods
A formal meta-analysis on all published studies was not possible due to differences in study populations, therapies and definitions of staging. Thus only the 5-year survival rates published from cancer registries were used for data pooling using the method suggested by Sutton et al. [29]. If standard errors for the construction of 95% confidence intervals were not reported, these were calculated using the standard method for proportions as described by Cantor et al. [30].
Results
Our search identified 39 potentially relevant studies, containing information on laryngeal cancer and estimates of survival times. Seven articles were excluded because they considered survival for head and neck cancer in general, without any relevant details for laryngeal cancer. Another three studies were not taken into account. One article [31] analysed data on the effect of lifestyle habits on prognosis of the combined group of laryngeal and hypopharyngeal cancer. However, no detailed survival time was provided for laryngeal cancer. Fakhry et al. [32] reported on HPV infection in laryngeal and hypopharyngeal carcinoma patients. However, there was no patient with laryngeal cancer, so that the study was excluded. In another article, there was no description of statistical analysis [33]. Thus, a total of 29 studies were examined in detail.
Out of these, the main topic of 16 studies was therapy of head and neck cancer or laryngeal cancer, 8 studies focused mainly on survival rates, 1 on comorbidity, 2 on quality of life after surgical intervention and 1 on survival after tracheotomy. Twenty-four of the studies considered laryngeal cancer only, while 6 studies examined head and neck cancer in general, with a subgroup of laryngeal cancer patients. In those studies reporting on laryngeal cancer only, 11 reported in detail on supraglottic, glottic and subglottic cancer, 3 on glottic and supraglottic, 5 on supraglottic and 5 on glottic cancer only. Tables 1, 2, 3 present the details of each of the studies according to the above-mentioned categories.
Geographic areas
An overview of studies evaluating survival rates based on hospital record or national cancer databases in specific geographic areas is given in Table 1 [34–38]. Hoffman et al. [34] identified 158,426 larynx cases in the huge National Cancer Database of the USA over a time period of 15 years, a nearly identical time period compared to Rachet et al. [35], who analysed the survival of around 20,000 men in England and Wales [34, 35]. Where Hoffman et al. [34] found a decreasing relative 5-year survival for laryngeal cancer over 17 years (1985—68.1%, 1993—62.8%), no clear trend was observed by Rachet et al. [35] Socio-demographic differences were identified as a cause for the differences in survival rates, but seemed unlikely to account for the decreasing survival in laryngeal cancer in the absence of a similar negative impact on survival for other cancers. The other three studies from Finland (Raitiola et al.), Italy (La Rosa et al.) and Japan (Tamura et al.), based on hospital records and much smaller numbers of laryngeal cancer patients, did not present any time trends, although Raitiola et al. covered a period of 30 years [36–38]. Differences in survival rates have been attributed to T- and N-status [36] or tumour staging [38].
Co-malignancy/quality of life/comorbidity
Table 2 gives an overview of the studies evaluating co-malignancy, quality of life and comorbidity in the context of laryngeal cancer [18, 39–41]. One study reported on metachronous and synchronous second primary malignancies in head and neck cancer [39]. Laryngeal carcinoma was the most common index tumour with a 5-year survival rate of 68.9% [39]; however, no details of tumour staging were given. Survival rates were lower for patients with a metachronous second primary malignancy (26%) and for those with synchronous primary malignancies (11.9%). The two studies by Olthoff et al. and Fung et al. [40, 41] studied the impact of organ function and quality of life for locally advanced laryngeal cancer. Here, the voice-related quality of life was better in patients after chemoradiation compared with laryngectomy. Chen et al. [18] showed the importance of comorbidity for treatment and survival in advanced laryngeal carcinoma patients, finding that patients with either moderate or severe comorbidity had significantly worse overall and 5-year survival (but not disease-specific) survival compared to those with no or mild comorbidity. However, no significant difference between the two comorbidity groups was observed in terms of survival.
Laser surgery
Studies evaluating the effectiveness of different therapeutic approaches on survival of laryngeal cancer patients are presented in Table 3 [17, 42–60]. In the group involving laser surgery, three studies consisted of a mixture of different stages and tumour locations [42–44], of which two assessed early glottic cancer only [45, 46] and one assessed advanced laryngeal cancer cases only [47]. Thus, the results for overall survival varied between 55% for the advanced [47] versus 90 [46] and 95% [45] for the early cancer cases. The only study that compared transoral laser surgery (TLS) with the conventional supraglottic approach found differences in the 5-year disease-specific survival rate (80 vs. 72%), but was based on small numbers [43].
Conventional surgery
Three articles compared conventional supraglottic partial laryngectomy (i.e. standard laryngectomy) with other approaches [48–50]. Prades et al. [48] found higher 5-year survival rates for the standard approach (63%) compared with laterally extended laryngectomy (47%) or anteriorly extended laryngectomy (45%). The highest rates were found by Piazza et al. [50] for patients with open-neck partial laryngectomy (ONPL, 100%) or endoscopic resection (ER, 95%). However, the low disease-specific survival for total laryngectomy (TL, 48%) reflects the negative prognostic effect of the locally most advanced tumours that were not deemed candidates for conservation procedures. Santos et al. [51] compared the overall survival of surgery (58.5%) versus radiotherapy (16.3%). Several demographic, clinical and pathological variables were studied, but only initial treatment, and T- and N-stage had a significant prognostic value for survival. The aim of the study by Sevilla et al. [52] was to preserve a functioning larynx and avoid permanent tracheotomy. The results of a multivariate Cox proportional hazards model showed that cervical lymph node metastases of class pN3 and a primary tumour classified as pT4 were statistically significant and independent predictors of reduced disease-specific survival.
Radiotherapy
Four studies compared the results of radiotherapy, of which two focused on glottic cancer patients only [53, 54]. The latter studies showed similar rates for overall and disease-specific survival. Both studies analysed patient records over a time period of nearly 30 years, but without showing any time trends. The multivariate analysis by Mendenhall et al. [53] revealed that T-stage, histological differentiation and overall treatment time significantly influenced survival, whereas Reddy et al. [54] differentiated only between small and bulky tumours, the latter with clearly lower disease-specific survival.
The other two articles evaluated the outcome for head and neck cancer in general and not only for laryngeal cancer. Kao et al. [55] identified 5297 patients in the SEER database with node-positive head and neck squamous cell carcinoma (HNSCC), including 797 laryngeal cancer patients, and showed a relatively low overall 5-year survival for laryngeal cancer (40.2%). This study shows that adjuvant radiation offers a significantly better overall survival rate for patients with node-positive HNSCC in general, which also holds true for laryngeal cancer. Rusthoven et al. [56] also used the data from the SEER database, but only presented 3-year survival rates, which slightly decreased between the periods 1988–1997 and 1998–2004.
Combination of therapies
The final five studies presented in this review compared different combinations of therapies in their analyses. With a time period of 42 years, the biggest study group was analysed by Nguyen-Tan et al. [57]. The patients were treated by surgery, postoperative radiation or radiochemotherapy, preoperative radiotherapy, radiotherapy only or radiochemotherapy only, with an overall 5-year survival of 65 (stage III) and 34% (stage IV). The prognostic factors in a multivariate analysis for better overall survival were lower N-stage and a higher haemoglobin level during radiotherapy. The time period analysed by Spector et al. was the same; however, only the results for a final group of 42 patients were presented [58].
Unfortunately, no detailed survival rates were given for the different treatment arms in the study by MacKenzie et al. [59], who compared the treatment outcomes of primary radical radiotherapy and surgery in locally advanced laryngeal cancer.
Only the 3-year survival rates were given by Boscolo-Rizzo et al. and Herchenhorn et al. [17, 60]. In the former, the rates differed only marginally in the two treatment groups (total laryngectomy with voice prosthesis and postoperative radiotherapy compared with those receiving concurrent chemoradiation for laryngeal preservation); however, the quality of life score was better in patients treated by chemoradiation [17]. The latter showed that previous tracheotomy was a prognostic factor for a shorter survival time rate (6 vs. 61%); however, as tracheotomy is mandatory in patients with a very advanced tumour stage, the advanced tumour stage is responsible for the poor prognosis [60].
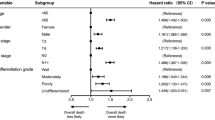
Figure 1 displays the results of all studies where the estimate for 5-year survival is given, together with the result of our meta-analysis using cancer registry studies only [34, 35], which yielded an overall rate for 5-year relative survival of 64.2% (95% confidence interval 63.7–64.7%).
Discussion
Our literature search identified 29 studies that evaluated survival of laryngeal cancer patients in general or focused on different subsites of the larynx. The sample size of these studies varied from only a few patients followed for a certain purpose or described by specific characteristics (n = 39 [40] up to tens of thousands of cases identified in cancer registries (n = 158,426 [34]). Clearly, the aims of the studies identified for this review were heterogeneous.
The decision on the treatment of laryngeal cancer is generally led by the goal of achieving a cure and preserving larynx function, and is based on many different factors: not only on tumour size, but also on other patient-related aspects such as comorbidities or a previous history of cancer. In addition, the treatment of laryngeal cancer has experienced much change in recent years, ranging from single therapies to combinations of different approaches. Several articles identified for this review focus on only one therapeutic method, that is, transoral laser surgery [44, 46], surgery [48, 49, 52] or radiotherapy [53, 54]. Other studies compare different therapeutic procedures, such as open hemi- or laryngectomy and transoral laser surgery [43, 50], surgery versus radiotherapy [51], total laryngectomy, neck dissection with radiotherapy versus any radiotherapy [58], surgery, chemo- and radiation therapy [17, 57] or radiotherapy and chemotherapy [60]. Studies showing the results for different therapies provide a descriptive picture of treatments of laryngeal cancer, but they cannot be directly compared to those that focus on other treatments.
Hoffman et al. [34] analysed the National Cancer Database of the USA, observing a trend toward decreasing survival amongst patients with laryngeal cancer from the mid-1980s to the mid-1990s, resulting in poor 5-year relative survival for those receiving either chemoradiation (59.2%) or irradiation alone (42.7%) when compared with that of surgery with irradiation (65.2%) and surgery alone (63.3%). A great advantage of that study was the possibility of comparing survival rates over time due to the rich database. On the other hand, this decreasing trend is described as an effect of the learning curve by Johnson [61], which reflects the fact that physicians experience several phases of accommodation to new therapies and diagnostics on their way from being beginners to experts, and that major changes have been introduced in the way patients with laryngeal cancer are treated in the last decade. Patterns of initial management across this same period indicate an increase in the use of chemoradiation and a decrease in the use of surgery despite an increase in the use of endoscopic resection [43]. For head and neck cancer in general, significantly higher progression-free and overall survival were observed by Bernier et al. [62], who showed that postoperative concurrent administration of high-dose cisplatin with radiotherapy was more efficacious than radiotherapy alone in patients with locally advanced head and neck cancer with special risk factors such as R1 resection or extracapsular spread, and does not cause an undue number of late complications. These results were partly confirmed by Cooper et al. [63], who also found longer disease-free survival rates for the combined treatment, but no significantly better overall survival and substantially more acute adverse effects of grade 3 or greater.
Since the two landmark phase-III studies from France and the USA [64, 65] demonstrated that there was a real alternative treatment for advanced laryngeal and hypopharyngeal cancer, the discussion on definitive non-surgical treatment for head and neck cancer started all over the world. The head and neck community also learnt that alternative multimodality treatment also had handicaps such as early and late toxicities, reduced functional outcome and treatment failure leading to high risk salvage surgery with several complications in many cases. To address this problem, Lefebvre and Ang [25] worked out a list of guidelines for better outcome specification after organ preservation therapy, which should be used in further clinical trials. The paper introduced a new end point: laryngoesophageal dysfunction-free survival. Also, considering better response, future trial populations should include patients with limited tumour size such as T2 or T3 laryngeal or hypopharyngeal squamous cell carcinoma. Until today, biomarkers have shown some correlation with better outcome after chemoradiation, but show strongly differing results and many technical peculiarities, so that the clinic impact is still limited. On the other hand, resurgence in specific genetic profiles associated with chemo- or radio response is a highly encouraging and promising field in many tumour entities [22].
However, today’s main guidelines for treatment of HNSCC are still based on phase-III trials and comprehensive meta-analysis [66], with excess of radiation or chemoradiation at the expense of surgical trials. As stated by Higgens and Wang [67], clinical recommendations for HNSCC treatment based on evidence are difficult due to the disproportion between surgical and non-surgical trials. This conflict is triggered by the fact that instruments for evaluating best surgical practice are different from methodological standards in non-surgical phase-II or -III trials [67]. Regarding current literature, induction chemotherapy before radiation treatment offers the possibility of chemoselection of good responders before therapy [26]. Furthermore, induction chemotherapy and sequential radiation lower the incidence of sever late toxicities and so improve functional outcome significantly [68]. Presently, the combination of docetaxel, platin and 5FU (TPF) is recommended as the best induction treatment in organ preservation trials [24] compared with PF alone. Since TPF is highly toxic, currently alternative induction combinations are advocated [26]. Worldwide, the only trial for organ preservation is the RTOG 91-11 trial, which compared induction (PF) with concurrent platin-based chemoradiation and radiation alone. After 5 years, disease-free survival in both the induction und concurrent group was 39%. Five-year laryngectomy-free survival was 45% in the induction and 47% in the concurrent group. Remarkably, there was a high rate of death unrelated to cancer in the concurrent group (36%) versus 18% in the induction group. Nevertheless, the study group did not sufficiently look for functional outcome and specific late toxicities [69]. To summarise, multimodality treatment in resectable laryngeal cancer is still a field of ongoing and future clinical trials and not to be recommended as standard treatment. In future, induction chemotherapy will seem to play a role in organ preservation in advanced laryngeal cancer. The main advantage of the induction approach is the possibility of early detection of responders to prevent unnecessary salvage and functional disasters in non-responders [26].
As the above-mentioned results are given for head and neck cancer patients in general, the same holds for patients with laryngeal cancer according to Sevilla et al. [52]. Here, severe and progressive late effects are seen in speech and swallowing in long-term survivors. Boscolo-Rizzo concluded that concurrent chemoradiation was associated with significant acute and late toxicity due to its radiosensitisation effects [17, 41]. However, concurrent chemoradiotherapy gave a significant benefit in the 5-year survival compared with radiotherapy alone, whereas adjuvant and induction chemotherapy did not improve survival. Consequently, concurrent chemoradiotherapy appears to be the most reasonable approach to preserving the larynx in patients with advanced laryngeal cancer. Holsinger et al. [16] claimed to have established risk-based criteria for treatment selection and functional outcome, rather than celebrating a single modality of treatment over any other, is this surgery, radiotherapy or chemotherapy. Selection of the treatment depends on patient factors, local expertise, and the availability of support and rehabilitative services [52].
This opens the discussion on the wide field of questions about quality of life (QOL) [17, 70]: the advantage of different treatments cannot be measured only in terms of overall or recurrence-free survival rates, but the quality of life after therapy has to be taken into account. Head and neck cancer and its associated treatment directly affect health-related QOL, as the most basic functions of speech and swallowing are frequently altered, while symptoms such as pain and psychosocial issues such as appearance and emotional functioning can also be problematic. The standard outcome measures of survival and disease status are essential and simple to record, but may be inadequate when there is a need to compare toxic therapies with similar disease control rates. More recently defined outcome measures such as larynx preservation rates after ‘organ preservation’ chemoradiation protocols epitomise the problem, as an in situ and disease-free larynx may be completely non-functional and leave a patient with a gastrostomy tube and tracheostomy after chemoradiation [71].
Promising results have been published for head and neck cancer and lifestyle factors or comorbidities, which might influence the survival of laryngeal cancer patients. Molina et al. [28] analysed the differences in head and neck cancer survival based on race, ethnicity and socioeconomic status in Florida/USA for the period 1998–2002 (N = 20,915). Significant differences in the median survival time for laryngeal cancer patients with regard to race (white, 49 months vs. African American, 25 months; p < 0.001), gender (men, 36 months vs. women, 41 months; p = 0.001) and area poverty level (lowest, 40 months, highest, 53 months; p < 0.0001) have been observed. In a multivariate analysis, race, poverty, age, gender, tumour site, stage, grade, treatment modality, history of smoking and alcohol consumption were reported as independent predictors for lower survival [31]. This means that there is additional scope for intervention, underlining not only the possibility of preventing laryngeal cancer by focusing on lifestyle factors such as smoking behaviour and alcohol consumption [2, 3], but also their influence on survivorship.
Directly related to the aspect of lifestyle factors is the field of comorbidities, as can be seen in a study by Di Martino et al. [39]. They found that heavy smokers and drinkers, who continued their habits after the completion of treatment for their index tumour, were at a particularly high risk for developing a second malignancy. Piccirillo et al. [19] analysed the records of 1,094 head and neck cancer patients in St. Louis, USA, for the years 1980–1991, and created a new head and neck-specific comorbidity index (WUHNCI). Seven comorbidity conditions (congestive heart disease, cardiac arrhythmia, peripheral vascular disease, pulmonary disease, renal disease, other controlled cancer, other uncontrolled cancer) were significantly related to survival (p = 0.001 to p = 0.07). The results pointed to the important influence of comorbidities and a previous and ongoing history of cancer (second primary cancer, recurrent malignancy) on therapy and survival outcome. Unfortunately, the study had to be excluded from this review because no details on 5-year survival rates were given. Thus, for future studies, clarification of the impact of lifestyle factors and comorbidities will be important; for example, some studies have shown a much lower survival for early stages compared to advanced stages [38, 52].
Some studies used the T categories to present their results, whereas others used the TNM stages I–IV. The two systems complement each other, because the staging combines three variables into one. The overall 5-year disease-specific survival, as presented by Sevilla et al. [52] showed significantly lower survival rates for stage II than for stage III (II: 71%/III: 80%). Here, the classification into stage III was caused by N1 (T1N1, T2N1–TNM classification) including a lower number of advanced tumours in stage III. Thus, bias caused by different classification systems for cases of different studies could not be excluded. The same might hold for the study by Tamura et al., in which unexpectedly high survival rates were presented for stage I–III cancer patients in Kyoto, Japan. On one hand, these glottis cancers seemed to be detected at the very early stages; however, on the other hand, the results were based on small numbers in some subgroups [38]. There have been several criticisms of that study, including the fact that many of the tumours were considered “advanced” because of their nodal status, and not because of their T category [38, 52]. Therefore, patients with mobile cords might have been candidates for conservative laryngeal surgery, rather than total laryngectomy. Given the excellent results documented for transoral laser microsurgery and supracricoid partial laryngectomy, many argue that these confounding factors may have favourably influenced the overall survival rates and the rate of laryngeal preservation, again indicating the difficulty of directly comparing survival rates based on therapy, an issue that also arose in a paper by the EUROCARE work group [14].
Due to the relatively low incidence of laryngeal cancer, many studies consider all head and neck cancer tumour sites together. In this way the study population increases, but on the other hand the evidence for each tumour site decreases, as laryngeal cancer has a better overall survival at 61.6% than for example hypopharyngeal cancer (29.2%) or oesophageal cancer (16.8%) (SEER) [13].
Human papillomavirus (HPV) has been linked to oropharyngeal carcinomas, but its current role in laryngeal squamous cell carcinoma is not clear. A significant influence of HPV on patient survival was observed by Hoffmann et al. [72], but only in combination with other prognostic factors, such as the lymph node status of the patient. The improved survival outcomes of HPV-positive versus HPV-negative patients with lymph node neck metastasis have been interpreted as being attributable to a better response of the HPV-positive group to therapy, i.e. induction chemotherapy and chemoradiation [32] or radiotherapy [72].
The advantage of analysing clinical data including therapy information is normally counterbalanced by the disadvantage that there may only be sparse data for analysing time trends over different years. The periods during which patients were included at first diagnosis ranged between 3.5 [60] and 44 years [58]. On the one hand, therapeutic methods may change over a large period of time, making it difficult to compare results, but on the other hand, having data from long periods provides a chance to consider trends over time. Unfortunately, survival rates for several years were not always reported, even when databases from cancer registries were used [36]. However, in general, these cancer registries do not provide therapy information. In this review, many studies had small sample sizes; the overall sample size was <100 in six studies and between 100 and 300 in eight studies, leading to rather imprecise estimates of survival rates when analysing subgroups of stages or therapies. The overall sample size was only above 16,000 subjects in four studies. Nevertheless, if in future the rich data of cancer registries could be analysed or presented in more detail, there might be the potential to study the trends and effects of therapies over time, which could ultimately enhance the survival and quality of life of laryngeal cancer patients.
The observed survival rates in different areas or countries depend on a number of factors including the availability of data, data collection and analysis methods, demographic and clinical characteristics of cases, time of diagnosis, therapeutic facilities and quality of care. In addition, information on most of these features (e.g. stage distribution of cases) is collected in different ways in each hospital or regional area. Some studies consider only overall survival rates; other studies provide disease- or cause-specific survival rates and only some studies consider both, while better estimates of the impact of tumour control on survival are provided by measuring cause-specific survival. However, the availability and access to cause-of-death statistics vary and are sometimes impossible to obtain in some countries.
In summary, the information provided in this review may be limited due to incomplete reporting of the data in the original articles. In addition, survival rates could not be extracted from some studies, since these details were not mentioned.
Conclusion
Direct comparison of different conservative and non-organ preservation surgical modalities in terms of survival is difficult. The different selection criteria of patients (especially regarding tumour extension and general conditions) prevent definite conclusions. However, this review provides a general picture of the complexity of factors influencing the survival of laryngeal cancer patients.
References
Ferlay J, Bray F, Pisani P, Parkin D (2001) GLOBOCAN 2000: cancer incidence, mortality and prevalence worldwide. IARC cancer base no. 5, IARC, Lyon, version 1.0
Ramroth H, Dietz A, Becher H (2004) Interaction effects and population-attributable risks for smoking and alcohol on laryngeal cancer and its subsites. A case–control study from Germany. Methods Inf Med 43:499–504. doi:10.1267/METH04050499
Shangina O, Brennan P, Szeszenia-Dabrowska N, Mates D, Fabiánová E, Fletcher T et al (2006) Occupational exposure and laryngeal and hypopharyngeal cancer risk in central and eastern Europe. Am J Epidemiol 164:367–375. doi:10.1093/aje/kwj208
Talamini R, Bosetti C, Vecchia CL, Maso LD, Levi F, Bidoli E et al (2002) Combined effect of tobacco and alcohol on laryngeal cancer risk: a case–control study. Cancer Causes Control 13:957–964
Hashibe M, Boffetta P, Zaridze D, Shangina O, Szeszenia-Dabrowska N, Mates D et al (2007) Contribution of tobacco and alcohol to the high rates of squamous cell carcinoma of the supraglottis and glottis in Central Europe. Am J Epidemiol 165:814–820. doi:10.1093/aje/kwk066
IARC (2003) Monographs on the evaluation of carcinogenic risks to humans tobacco smoke and involuntary smoking. IARC, Lyon, p 83
Ramroth H, Dietz A, Becher H (2008) Environmental tobacco smoke and laryngeal cancer: results from a population-based case–control study. Eur Arch Otorhinolaryngol 265:1367–1371. doi:10.1007/s00405-008-0651-7
Lee YCA, Boffetta P, Sturgis EM, Wei Q, Zhang ZF, Muscat J et al (2008) Involuntary smoking and head and neck cancer risk: pooled analysis in the international head and neck cancer epidemiology consortium. Cancer Epidemiol Biomarkers Prev 17:1974–1981. doi:10.1158/1055-9965.EPI-08-0047
Becher H, Ramroth H, Ahrens W, Risch A, Schmezer P, Dietz A (2005) Occupation, exposure to polycyclic aromatic hydrocarbons and laryngeal cancer risk. Int J Cancer 116:451–457. doi:10.1002/ijc.21049
Ramroth H, Dietz A, Ahrens W, Becher H (2008) Occupational wood dust exposure and the risk of laryngeal cancer: a population based case–control study in Germany. Am J Ind Med 51:648–655. doi:10.1002/ajim.20605
Boffetta P, Richiardi L, Berrino F, Estève J, Pisani P, Crosignani P et al (2003) Occupation and larynx and hypopharynx cancer: an international case–control study in France, Italy, Spain, and Switzerland. Cancer Causes Control 14:203–212
Dietz A, Ramroth H, Urban T, Ahrens W, Becher H (2004) Exposure to cement dust, related occupational groups and laryngeal cancer risk: results of a population based case–control study. Int J Cancer 108:907–911. doi:10.1002/ijc.11658
http://seer.cancer.gov/csr/1975_2006/results_merged/topic_survival.pdf
Sant M, Allemani C, Santaquilani M, Knijn A, Marchesi F, Capocaccia R et al (2009) EUROCARE-4. Survival of cancer patients diagnosed in 1995–1999. Results and commentary. Eur J Cancer 45:931–991. doi:10.1016/j.ejca.2008.11.018
Pfister DG, Laurie SA, Weinstein GS, Mendenhall WM, Adelstein DJ et al (2006) American society of clinical oncology clinical practice guideline for the use of larynx-preservation strategies in the treatment of laryngeal cancer. J Clin Oncol 24:3693–3704. doi:10.1200/JCO.2006.07.4559
Holsinger FC, Weber RS (2007) Swing of the surgical pendulum: a return to surgery for treatment of head and neck cancer in the 21st century? Int J Radiat Oncol Biol Phys 69:S129–S131. doi:10.1016/j.ijrobp.2007.05.044
Boscolo-Rizzo P, Maronato F, Marchiori C, Gava A, Mosto MCD (2008) Long-term quality of life after total laryngectomy and postoperative radiotherapy versus concurrent chemoradiotherapy for laryngeal preservation. Laryngoscope 118:300–306. doi:10.1097/MLG.0b013e31815a9ed3
Chen AY, Matson LK, Roberts D, Goepfert H (2001) The significance of comorbidity in advanced laryngeal cancer. Head Neck 23:566–572
Piccirillo JF, Lacy PD, Basu A, Spitznagel EL (2002) Development of a new head and neck cancer-specific comorbidity index. Arch Otolaryngol Head Neck Surg 128:1172–1179
Sabin SL, Rosenfeld RM, Sundaram K, Har-el G, Lucente FE (1999) The impact of comorbidity and age on survival with laryngeal cancer. Ear Nose Throat J 78:578, 581–578, 584
Castro MAF, Dedivitis RA, Ribeiro KCB (2007) Comorbidity measurement in patients with laryngeal squamous cell carcinoma. ORL J Otorhinolaryngol Relat Spec 69:146–152. doi:10.1159/000099223
Dietz A, Boehm A, Mozet C, Wichmann G, Giannis A (2008) Current aspects of targeted therapy in head and neck tumors. Eur Arch Otorhinolaryngol 265(Suppl 1):S3–S12. doi:10.1007/s00405-008-0697-6
Machtay M, Moughan J, Trotti A, Garden AS, Weber RS, Cooper JS et al (2008) Factors associated with severe late toxicity after concurrent chemoradiation for locally advanced head and neck cancer: an RTOG analysis. J Clin Oncol 26:3582–3589. doi:10.1200/JCO.2007.14.8841
Pointreau Y, Garaud P, Chapet S, Sire C, Tuchais C, Tortochaux J et al (2009) Randomized trial of induction chemotherapy with cisplatin and 5-fluorouracil with or without docetaxel for larynx preservation. J Natl Cancer Inst 101:498–506. doi:10.1093/jnci/djp007
Lefebvre JL, Ang KK, Panel LPC (2009) Larynx preservation clinical trial design: key issues and recommendations—a consensus panel summary. Int J Radiat Oncol Biol Phys 73:1293–1303
Dietz A, Boehm A, Horn IS, Kruber P, Bechmann I, Golusinski W et al (2010) Assay-based response evaluation in head and neck oncology: requirements for better decision making. Eur Arch Otorhinolaryngol 267:483–494. doi:10.1007/s00405-009-1191-5
Wittekind C, Sobin L (2002) TNM classification of malignant tumours. Wiley-Liss, New York
Molina MA, Cheung MC, Perez EA, Byrne MM, Franceschi D, Moffat FL et al (2008) African American and poor patients have a dramatically worse prognosis for head and neck cancer: an examination of 20,915 patients. Cancer 113:2797–2806. doi:10.1002/cncr.23889
Sutton A, Abrams K, Jones D, Sheldon T, Song F (2000) Methods for meta-analysis in medical research. Wiley, Chichester
Cantor AB (2001) Projecting the standard error of the Kaplan–Meier estimator. Stat Med 20:2091–2097. doi:10.1002/sim.856
Dikshit RP, Boffetta P, Bouchardy C, Merletti F, Crosignani P, Cuchi T et al (2005) Lifestyle habits as prognostic factors in survival of laryngeal and hypopharyngeal cancer: a multicentric European study. Int J Cancer 117:992–995. doi:10.1002/ijc.21244
Fakhry C, Westra WH, Li S, Cmelak A, Ridge JA, Pinto H et al (2008) Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. J Natl Cancer Inst 100:261–269. doi:10.1093/jnci/djn011
Adamopoulos G, Yotakis I, Apostolopoulos K, Manolopoulos L, Kandiloros D, Ferekidis E (1997) Supraglottic laryngectomy-series report and analysis of results. J Laryngol Otol 111:730–734
Hoffman HT, Porter K, Karnell LH, Cooper JS, Weber RS, Langer CJ et al (2006) Laryngeal cancer in the United States: changes in demographics, patterns of care, and survival. Laryngoscope 116:1–13. doi:10.1097/01.mlg.0000236095.97947.26
Rachet B, Quinn MJ, Cooper N, Coleman MP (2008) Survival from cancer of the larynx in England and Wales up to 2001. Br J Cancer 99(Suppl 1):S35–S37. doi:10.1038/sj.bjc.6604581
Raitiola H, Pukander J, Laippala P (1999) Glottic and supraglottic laryngeal carcinoma: differences in epidemiology, clinical characteristics and prognosis. Acta Otolaryngol 119:847–851
LaRosa F, Petrinelli AM, Stracci F, Ammetto C, Casucci P, Mastrandrea V (2000) Long term survival of upper aerodigestive tract cancer in male patients in the Umbria region (Italy). Eur J Epidemiol 16:489–494
Tamura Y, Tanaka S, Asato R, Hirano S, Yamashita M, Tamaki H, et al. (2007) Therapeutic outcomes of laryngeal cancer at Kyoto University Hospital for 10 years. Acta Otolaryngol Suppl, pp 62–65. doi:10.1080/00016480601067990
DiMartino E, Sellhaus B, Hausmann R, Minkenberg R, Lohmann M, Esthofen MW (2002) Survival in second primary malignancies of patients with head and neck cancer. J Laryngol Otol 116:831–838. doi:10.1258/00222150260293664
Olthoff A, Ewen A, Wolff H, Hermann R, Vorwerk H, Hille A et al (2009) Organ function and quality of life after transoral laser microsurgery and adjuvant radiotherapy for locally advanced laryngeal cancer. Strahlenther Onkol 185:303–309. doi:10.1007/s00066-009-1967-y
Fung K, Lyden TH, Lee J, Urba SG, Worden F, Eisbruch A et al (2005) Voice and swallowing outcomes of an organ-preservation trial for advanced laryngeal cancer. Int J Radiat Oncol Biol Phys 63:1395–1399. doi:10.1016/j.ijrobp.2005.05.004
Preuss SF, Cramer K, Klussmann JP, Eckel HE, Guntinas-Lichius O (2009) Transoral laser surgery for laryngeal cancer: outcome, complications and prognostic factors in 275 patients. Eur J Surg Oncol 35:235–240. doi:10.1016/j.ejso.2008.01.012
Cabanillas R, Rodrigo JP, Llorente JL, Suárez C (2008) Oncologic outcomes of transoral laser surgery of supraglottic carcinoma compared with a transcervical approach. Head Neck 30:750–755. doi:10.1002/hed.20778
Motta S, Moscillo L, Imperiali M, Motta G (2003) CO2 laser treatment of bilateral vocal cord paralysis in adduction. ORL J Otorhinolaryngol Relat Spec 65:359–365. doi:10.1159/000076055
Hartl DM, de Monès E, Hans S, Janot F, Brasnu D (2007) Treatment of early-stage glottic cancer by transoral laser resection. Ann Otol Rhinol Laryngol 116:832–836
Ansarin M, Santoro L, Cattaneo A, Massaro MA, Calabrese L, Giugliano G et al (2009) Laser surgery for early glottic cancer: impact of margin status on local control and organ preservation. Arch Otolaryngol Head Neck Surg 135:385–390. doi:10.1001/archoto.2009.10
Hinni ML, Salassa JR, Grant DG, Pearson BW, Hayden RE, Martin A et al (2007) Transoral laser microsurgery for advanced laryngeal cancer. Arch Otolaryngol Head Neck Surg 133:1198–1204. doi:10.1001/archotol.133.12.1198
Prades JM, Simon PG, Timoshenko AP, Dumollard JM, Schmitt T, Martin C (2005) Extended and standard supraglottic laryngectomies: a review of 110 patients. Eur Arch Otorhinolaryngol 262:947–952. doi:10.1007/s00405-004-0882-1
Pellini R, Pichi B, Ruscito P, Ceroni AR, Caliceti U, Rizzotto G et al (2008) Supracricoid partial laryngectomies after radiation failure: a multi-institutional series. Head Neck 30:372–379. doi:10.1002/hed.20709
Piazza C, Peretti G, Cattaneo A, Garrubba F, Zinis LORD, Nicolai P (2007) Salvage surgery after radiotherapy for laryngeal cancer: from endoscopic resections to open-neck partial and total laryngectomies. Arch Otolaryngol Head Neck Surg 133:1037–1043. doi:10.1001/archotol.133.10.1037
Santos CR, Kowalski LP, Magrin J, Fogaroli RC, Santos JC, Sabóia MV et al (1998) Prognostic factors in supraglottic carcinoma patients treated by surgery or radiotherapy. Ann Otol Rhinol Laryngol 107:697–702
Sevilla MA, Rodrigo JP, Llorente JL, Cabanillas R, López F, Suárez C (2008) Supraglottic laryngectomy: analysis of 267 cases. Eur Arch Otorhinolaryngol 265:11–16. doi:10.1007/s00405-007-0415-9
Mendenhall WM, Amdur RJ, Morris CG, Hinerman RW (2001) T1–T2N0 squamous cell carcinoma of the glottic larynx treated with radiation therapy. J Clin Oncol 19:4029–4036
Reddy SP, Hong RL, Nagda S, Emami B (2007) Effect of tumor bulk on local control and survival of patients with T1 glottic cancer: a 30-year experience. Int J Radiat Oncol Biol Phys 69:1389–1394. doi:10.1016/j.ijrobp.2007.05.077
Kao J, Lavaf A, Teng MS, Huang D, Genden EM (2008) Adjuvant radiotherapy and survival for patients with node-positive head and neck cancer: an analysis by primary site and nodal stage. Int J Radiat Oncol Biol Phys 71:362–370. doi:10.1016/j.ijrobp.2007.09.058
Rusthoven KE, Raben D, Chen C (2008) Improved survival in patients with stage III–IV head and neck cancer treated with radiotherapy as primary local treatment modality. Int J Radiat Oncol Biol Phys 72:343–350. doi:10.1016/j.ijrobp.2007.12.046
Nguyen-Tan PF, Le QT, Quivey JM, Singer M, Terris DJ, Goffinet DR et al (2001) Treatment results and prognostic factors of advanced T3–4 laryngeal carcinoma: the University of California, San Francisco (UCSF) and Stanford University Hospital (SUH) experience. Int J Radiat Oncol Biol Phys 50:1172–1180
Spector JG, Sessions DG, Lenox J, Simpson J (2006) Management of T3N1 glottic carcinoma: therapeutic outcomes. Laryngoscope 116:106–110. doi:10.1097/01.mlg.0000184767.62682.3d
MacKenzie RG, Franssen E, Balogh JM, Gilbert RW, Birt D, Davidson J (2000) Comparing treatment outcomes of radiotherapy and surgery in locally advanced carcinoma of the larynx: a comparison limited to patients eligible for surgery. Int J Radiat Oncol Biol Phys 47:65–71
Herchenhorn D, Dias FL, Ferreira CG, Araújo CM, Lima RA, Small IA et al (2008) Impact of previous tracheotomy as a prognostic factor in patients with locally advanced squamous cell carcinoma of the larynx submitted to concomitant chemotherapy and radiation. ORL J Otorhinolaryngol Relat Spec 70:381–388. doi:10.1159/000163034
Johnson J (2006) Outcomes in laryngeal cancer: a product of the learning curve? Laryngoscope 116:1529. doi:10.1097/01.mlg.0000236092.52123.a9
Bernier J, Domenge C, Ozsahin M, Matuszewska K, Lefèbvre JL, Greiner RH et al (2004) Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. N Engl J Med 350:1945–1952
Cooper JS, Pajak TF, Forastiere AA, Jacobs J, Campbell BH, Saxman SB et al (2004) Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck. N Engl J Med 350:1937–1944
Lefebvre JL, Chevalier D, Luboinski B, Kirkpatrick A, Collette L, Sahmoud T (1996) Larynx preservation in pyriform sinus cancer: preliminary results of a European organization for research and treatment of cancer phase III trial. EORTC head and neck cancer cooperative group. J Natl Cancer Inst 88:890–899
The Department of Veterans Affairs Laryngeal Cancer Study Group (1991) Induction chemotherapy plus radiation compared with surgery plus radiation in patients with advanced laryngeal cancer. N Engl J Med 324:1685–1690. doi:10.1056/NEJM199106133242402
Pignon JP, le Maître A, Maillard E, Bourhis J, MACHNCC Group (2009) Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): an update on 93 randomised trials and 17, 346 patients. Radiother Oncol 92:4–14. doi:10.1016/j.radonc.2009.04.014
Higgins KM, Wang JR (2008) State of head and neck surgical oncology research—a review and critical appraisal of landmark studies. Head Neck 30:1636–1642. doi:10.1002/hed.20863
Dietz A, Rudat V, Dreyhaupt J, Pritsch M, Hoppe F, Hagen R et al (2009) Induction chemotherapy with paclitaxel and cisplatin followed by radiotherapy for larynx organ preservation in advanced laryngeal and hypopharyngeal cancer offers moderate late toxicity outcome (DeLOS-I-trial). Eur Arch Otorhinolaryngol 266:1291–1300. doi:10.1007/s00405-008-0846-y
Forastiere AA, Trotti A, Pfister DG, Grandis JR (2006) Head and neck cancer: recent advances and new standards of care. J Clin Oncol 24:2603–2605. doi:10.1200/JCO.2006.07.1464
Hanna E, Sherman A, Cash D, Adams D, Vural E, Fan CY et al (2004) Quality of life for patients following total laryngectomy vs chemoradiation for laryngeal preservation. Arch Otolaryngol Head Neck Surg 130:875–879. doi:10.1001/archotol.130.7.875
Oates J, Clark JR, Read J, Reeves N, Gao K, O’Brien CJ (2008) Integration of prospective quality of life and nutritional assessment as routine components of multidisciplinary care of patients with head and neck cancer. ANZ J Surg 78:34–41. doi:10.1111/j.1445-2197.2007.04353.x
Hoffmann M, Görögh T, Gottschlich S, Lohrey C, Rittgen W, Ambrosch P et al (2005) Human papillomaviruses in head and neck cancer: 8 year-survival-analysis of 73 patients. Cancer Lett 218:199–206. doi:10.1016/j.canlet.2004.09.027
Acknowledgments
The work of Elisabeth Rudolph was supported in part by a DFG grant from the GRK 793 Graduate College: “Epidemiology of communicable and chronic, non-communicable diseases and their interrelationships” at the University Hospital at Heidelberg.
Conflict of interest
The authors declare no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rudolph, E., Dyckhoff, G., Becher, H. et al. Effects of tumour stage, comorbidity and therapy on survival of laryngeal cancer patients: a systematic review and a meta-analysis. Eur Arch Otorhinolaryngol 268, 165–179 (2011). https://doi.org/10.1007/s00405-010-1395-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-010-1395-8