Abstract
The purpose of this study was to investigate and compare the bacteriology of postradiotherapy chronic rhinosinusitis (postRT-CRS) and chronic rhinosinusitis (CRS) by evaluating the aspiration materials of the maxillary sinus of patients with postRT-CRS and patients with CRS. We collected the secretions of the maxillary sinus from 30 nasopharyngeal carcinoma patients with postRT-CRS and 30 patients with CRS for aerobe/facultative anaerobe bacteria culture. The most common isolates in the postRT-CRS group were Streptocuccus viridans, Staphylococcus aureus and Haemophilus influenzae, while those in the CRS group were Haemophilus influenzae, Pseudomonas aeruginosa and Staphylococcus aureus. Isolated Gram-positive coccus rate in postRT-CRS patients was significantly higher than in CRS patients (62.50% compared with 30.00%, respectively; P < 0.05), and isolated Gram-negative bacilli rate in postRT-CRS patients was significantly lower than in CRS patients (31.25% compared with 70.00%, respectively; P < 0.05). However, the incidence of positive cultures was not significantly different between the postRT-CRS group and the CRS group (P > 0.05). This study found that there were some differences in bacteriology between postRT-CRS and CRS. Gram-positive coccus was the predominant aerobic/facultative anaerobe pathogenic bacterium in patients with postRT-CRS, and Gram-negative bacilli was predominant in CRS patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nasopharyngeal carcinoma (NPC) is one of the most common head and neck malignancies in southern China, including Guangxi, Guangdong and Hong Kong. Radiotherapy (RT) is still the primary method of treating NPC. The radiation field ordinarily covers the nasopharyngeal cavity, skull base, posterior choana, oropharyngeal cavity, sphenoid sinus, ethmoid sinus, posterior one-third of the maxillary sinus and the upper neck [1]. Therefore, when the tumor cells are killed by irradiation, adjacent normal tissues and organs are unavoidably exposed and damaged, including the sinonasal mucosa, causing many sequelae. Postradiotherapy chronic rhinosinusitis (postRT-CRS) is one of these sequelae, and medical treatment with antibotics or nasal douche was advised to control the symptoms [2]. After aggressive medical treatment, rhinosinusitis symptoms in most of those patients could be improved [3]. Until now, there were few papers concerning the role of microbiology in such kind of rhinosinusitis. Some literature reported bacteriology of rhinosinusitis in NPC survivors, but their research only described the results in acute patients [4, 5].
Chronic rhinosinusitis (CRS) is a very common chronic disease with a substantial health-care impact. But the etiology of CRS is still the focus of much debate, and bacterial infection, allergy, fungi, superantigens and a crop of other factors have been implicated as causes of CRS. Especially in microbiology, there are many literature that study the bacteriology of chronic rhinosinusitis and attempt to explore its real role in this kind of chronic disease [6–9]. However, these literature could not give a coincident result.
The main aims of this study were twofold: first, to investigate the bacteriology of postRT-CRS in NPC patients and, second, to study the similarities and differences between postRT-CRS and CRS in bacteriology.
Materials and methods
Total of 30 NPC patients with postRT-CRS, who did not have any evidences of rhinosinusitis before RT, and 30 patients diagnosed with CRS at the Department of Otorhinolaryngology, Guangxi Medical University from November 2006 through December 2007 were included in this study. They were divided into the postRT-CRS group and the CRS group, respectively. The ages of the 30 patients in the postRT-CRS group (24 men and 6 women) ranged from 23 to 70 (mean age 42.7 ± 10.4), and they all had received a 7-week course of external beam radiotherapy to a median dose of 70.0 Gy (range, 66–74 Gy) for treatment of NPC. Of these patients, 11 had received adjuvant chemotherapy consisting of 5-fluorouracil and cisplatin. Their duration of sinus symptoms after RT, including mucopurulent rhinorrhea, nasal obstruction and postnasal drip, ranged from 6 months to 8.5 years (mean 2.92 ± 2.20 years). The CRS group comprised 23 men and 7 women (mean age 33.8 ± 12.4, between 21–59 years), whose duration of sinus symptoms ranged from 4 months to 15 years (mean 4.97 ± 4.38 years). Every patient in these two groups showed total haziness of maxillary sinus on sinus computed tomography. Additionally, all the patients had not taken treatment including antibiotics or intranasal corticosteroid for at least 1 week prior to aspirate sampling. None of the patients had a history of immunologic deficiency disease, cystic fibrosis, diabetes or had undergone endoscopic sinus surgery.
This study was approved by the ethical committee of Guangxi Medical University. All patients gave their informed consent before their inclusion in this study.
After sterilizing the external nose and vestibule with 1% povidone iodine solution, the specimens was obtained from the maxillary sinus by puncture antral through the inferior meatus. All samples were inoculated into a bacterial isolation media within 30 min to search for aerobic and facultative anaerobe bacteria. Aerobic/facultative anaerobe cultures were incubated at 35.8°C under 5% CO2 onto 5% sheep blood agar, chocolate agar and MacConkey agar for 48 h. The identity of each isolate was corroborated with the API 32ID (Biomerieux ATB, Expression, France). The bacteria was tested by the staffs of the Clinic Laboratory Centre of Guangxi Medical University.
The culture results of the maxillary sinus specimens were compared between the postRT-CRS group and the CRS group by Pearson χ2 tests. Results were considered significant when the P value was <0.05.
Results
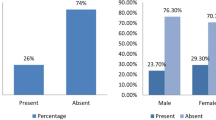
Of the 37 specimens collected from 37 maxillary sinuses of the 30 NPC patients with postRT-CRS, 27 cultures (72.97%) were positive. There were 32 isolates yielded, including 13 species of bacteria. The percentage of aerobic/facultative aerobic Gram-positive cocci and Gram-negative bacilli was 62.50 and 31.25%, respectively. The most common bacteria were the Streptococcus viridans (n = 6), Staphylococcus aureus (n = 5) and Haemophilus influenzae (n = 5). Streptococcus viridans were identified in 18.75% of the total isolates, 16.2% of the total cultures and 20% of the NPC patients.
Also, 37 specimens from 37 maxillary sinuses of the 30 patients with ordinary CRS were sent for culture, and 19 cultures (51.35%) were positive. However, there were only 20 isolates yielded, consisting of seven species of bacteria. Of the 20 isolates, 30% were Gram-positive cocci, and the others were all Gram-negative bacilli. The most common pathogenic bacteria were Haemophilus influenzae (n = 9), which were identified in 45% of the total isolates, followed by Pseudomonas aeruginosa (20%) and Streptococcus viridans (10%). Aerobic Gram-positive bacillus and Gram-negative coccus in patients of this group were not found.
Even though the number of isolates per culture ranged from 0 to 3, the majority only produced a single isolate in the two groups. Of 27 positive cultures in the postRT-CRS group, 23 cultures (85%) only produced a single isolate, 3 cultures produced two species of isolates, and 1 culture produced three species of isolates. Compared with the postRT-CRS group, the cultures producing a single isolate had a higher percentage in the CRS group. There were 18 of 19 positive cultures (94.7%) only yielding a single isolate, and 1 of 19 positive cultures (5.3%) yielding two species of isolates. Table 1 summarizes the overall data for the two groups. On comparing the incidence of positive cultures or the incidence of positive patients between the postRT-CRS group and the CRS group no significant difference could be found (P > 0.05; Table 2). By contrast, the rate of isolated Gram-positive cocci in the postRT-CRS group was significantly higher than in the CRS group (20 of 32 (62.50%) compared with 6 of 20 (30.00%), respectively; P < 0.05), while the rate of isolated Gram-negative bacilli in the CRS group was significantly higher than in the NPC group (10 of 32 (31.25%) compared with 14 of 20 (70.00%), respectively; P < 0.05; Table 3). The rate of isolated Haemophilus influenzae in the CRS group, which was the unique species of bacteria with significant difference between the two groups, was significantly higher than in the postRT-CRS group (P < 0.05; Table 3).
Discussion
RT for NPC is usually associated with mucosal side effects at the tumor site and surrounding structures, and rhinosinusitis is one of these sequelae [10]. Kamel et al. [11] found that the post-RT mucociliary clearance delay time in NPC patients gradually worsened with time for up to 6 months and then stabilized and persisted. Furthermore, according to the 2007 European Position Paper on Rhinosinusitis and Nasal Polyps (EP3OS), chronic rhinosinusitis (CRS) is defined as more than 12 weeks of symptoms without complete resolution [12]. Therefore, we thought that the bacteriology of postradiotherapy chronic rhinosinusitis (postRT-CRS) in NPC patients 6 months after RT, whose clinical symptoms persist for more than 12 weeks, was comparable to the bacteriology of ordinary CRS in patients without any underlying disease.
The bacteriology of acute rhinosinusitis (ARS) in NPC patients after RT has been investigated in some literature. In Hsin et al.’s study [4], frequently identified aerobes and facultative anaerobes included alpha-hemolytic streptococcus, Staphylococcus aureus and Pseudomonas aeruginosa. Huang et al. [5] collected 33 samples of ARS for aerobic culture from the middle meatus of 25 patients who underwent RT for NPC. Staphylococcus aureus comprised 42% of all aerobes. As much as 36% of the aerobic isolates were Gram-negative bacilli. However, persistent rhinosinusitis symptoms lasted for less than 3 months in all the patients in their studies.
In our study, the duration of symptoms of every postRT-CRS patient was more than 6 months. A total of 13 species of bacteria were isolated, and monoinfection existed in most of the specimens. The distribution of aerobic/facultative aerobic bacteria in maxillary sinuses of the postRT-CRS patients in this study was similar to that seen in Hsin CH et al.’s study [4]. The most common aerobic bacteria were Streptococcus viridans (18.75% of cultures) and Staphylococcus aureus (15.625% of cultures). In this study, however, Haemophilus influenzae was the most common Gram-negative aerobic bacilli, and we did not find Pseudomonas aeruginosa in the NPC patients.
Previous investigations on the bacteriology of chronic rhinosinusitis were made with different sampling methods. Consequently, the results of these studies were variable. The isolated aerobic bacteria rate was 60.8 ~ 90.4%, and the most common aerobic bacteria were Staphylococcus aureus, Staphylococcus epidermidis and Streptococcus viridans [6, 7, 13, 14].
In the present study, we found that the most common bacteria were Haemophilus influenzae (45% of isolates), followed by Pseudomonas aeruginosa, Streptococcus viridans and Staphylococcus aureus. Although there were some differences between our results and some of the previous studies, our results were in concordance with the findings of Kim et al. and Finegold et al. [8, 9]. Kim et al. gave two reasons to explain the high isolation rate of Haemophilus influenzae. One was that since most of the patients in their study previously used antibiotics, the isolation rate of the other pathogens may have decreased while that of Haemophilus influenzae, which was previously reported to show no difference in culture results before and after antibiotic treatment, were shown to be relatively high. Another reason was that the isolation rate of Gram-negative organisms such as Haemophilus influenzae increased as the severity of inflammation in the maxillary sinus increased [15].
To the best of our knowledge, this is the first study that compares the bacteriology of postRT-CRS and CRS. In this study, the predominant aerobic/facultative aerobic bacteria in patients with postRT-CRS and the patients with CRS were Gram-positive cocci and Gram-negative bacilli, respectively. In the CRS group, the isolated Haemophilus influenzae rate was significantly higher than in the postRT-CRS group (P < 0.05). The results of the comparison may be explained by two main points. First, although all the patients of the two groups did not use any antibiotics at least 1 week before sampling, most of the patients in the CRS group had already received drug treatment with the majority of antibiotics aimed toward Gram-positive bacteria, but only a few patients in the postRT-CRS group had used antibiotics after RT. Second, inflammation in the maxillary sinus was relatively severe in most of the patients with CRS in our study. However, the sample size was not large enough to make a statistical comparison of the overall distribution between these two groups.
It should be noted that a previous study had demonstrated delayed effects of radiation on nasal epithelium in patients with NPC, including epitheliul sloughing, cilia loss and ciliary dysmorphism, and this kind of long-term damage by radiation may be responsible for the prolonged sinusitis of irradiated NPC patients [10]. In our study, none of the postRT-CRS patients had rhinosinusitis before RT, and the signs and symptoms of rhinosinusitis appeared soon after RT and persisted for a long time. This also suggested that the presence of imflammation and bacteria was only a result secondary to sinus mucosa damaged by irradiation in the pathogenesis of postRT-CRS. Irreversible impairment of mucociliary function may result in the disorder of drainage of the sinuses, which allows bacteria to invade the sinus cavity more easily. Therefore, the presence of bacteria cannot be taken as an indication for antibiotic treatment unless acute exacerbation occurs.
Conclusion
Although anaerobic bacteria was not observed because of the difficulty of specimen transportation and the small sample size in our study, our findings demonstrated that there are some differences in bacteriology between postRT-CRS and CRS. The predominant aerobic/facultative anaerobic bacteria in NPC patients with postRT-CRS were Gram-positive cocci, whereas that in patients with CRS were Gram-negative bacilli. We hope that this study will be helpful in investigating the role of bacteria in postRT-CRS of NPC patients,and CRS, and in directing antibiotic therapy in these two kinds of sinus diseases.
References
Teo PM, Kwan WH, Leung SF et al (1996) Early tumour response and treatment toxicity after hyperfractionated radiotherapy in nasopharyngeal carcinoma. Br J Radiol 69:241–248
Hsuch CJ, Shu CH, Lin CZ (2000) Post-irradiation changes of the paranasal sinuses in patients with nasopharyngeal carcinoma. J Taiwan Otolaryngol Head Neck Surg 35:162–167
Su MC, Jiang RS, Chiang JL et al (2006) Endoscopic sinus surgery for the treatment of chronic rhinosinusitis in patients with post-irradiated nasopharyngeal carcinoma. Am J Otolaryngol 27:47–49. doi:10.1016/j.amjoto.2005.07.007
Hsin CH, Tsao CH, Su MC (2007) Bacteriology of acute rhinosinusitis in nasopharyngeal carcinoma survivors: a result of maxillary sinus punctures. Eur Arch Otorhinolaryngol 264:1157–1162. doi:10.1007/s00405-007-0334-9
Huang WH, Liu CM, Chao TK et al (2007) Middle meatus bacteriology of acute rhinosinusitis in patients after irradiation of nasopharynx. Am J Rhinol 21:286–288. doi:10.2500/ajr.2007.21.3016
Araujo E, Palombini BC, Cantarelli V et al (2003) Microbiology of middle meatus in chronic rhinosinusitis. Am J Rhinol 17:9–15
Aral M, Keles E, Kaygusuz I (2003) The microbiology of ethmoid and maxillary sinuses in patients with chronic sinusitis. Am J Otolaryngol 24:163–168. doi:10.1016/S0196-0709(02)32420-7
Finegold SM, Flynn MJ, Rose FV et al (2002) Bacteriologic findings associated with chronic bacterial maxillary sinusitis in adults. Clin Infect Dis 35:428–433. doi:10.1086/341899
Kim HJ, Lee K, Yoo JB et al (2006) Bacteriological findings and antimicrobial susceptibility in chronic sinusitis with nasal polyp. Acta Otolaryngol 126:489–497. doi:10.1080/00016480500437385
Lou PJ, Chen WP, Tai CC et al (1999) Delayed irradiation effects on nasal epithelium in patients with nasopharyngeal carcinoma. Ann Otol Rhinol Laryngol 108:474–480
Kamel R, Al-Badawy S, Khairy A et al (2004) Nasal and paranasal sinus changes after radiotherapy for nasopharyngeal carcinoma. Acta Otolaryngol 124:532–535. doi:10.1080/00016480410018106
Fokkens W, Lund V, Mullol J (2007) European position paper on rhinosinusitis and nasal polyps 2007: a summary for otorhinolaryngologists. Rhinology 45:97–101 on behalf of the European Position Paper on Rhinosinusitis, Nasal Polyps group (2007) EP3OS 2007
Merino LA, Ronconi MC, Hrenuk GE et al. (2003) Bacteriologic findings in patients with chronic sinusitis. Ear Nose Throat J 82:798–800, 803–794, 806
Biel MA, Brown CA, Levinson RM et al (1998) Evaluation of the microbiology of chronic maxillary sinusitis. Ann Otol Rhinol Laryngol 107:942–945
Jiang RS, Lin JF, Hsn CY (2002) Bacteriology of chronic maxillary sinusitis in relation to sinoscopic appearance. Am J Rhinol 16:249–253
Conflict of interest statement
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Deng, ZY., Tang, AZ. Bacteriology of postradiotherapy chronic rhinosinusitis in nasopharyngeal carcinoma patients and chronic rhinosinusitis. Eur Arch Otorhinolaryngol 266, 1403–1407 (2009). https://doi.org/10.1007/s00405-009-0915-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-009-0915-x