Abstract
Rhinosinusitis is a common complication in patients with nasopharyngeal carcinoma (NPC) who receive radiotherapy. An impaired mucociliary clearance due to this treatment may be the major cause of rhinosinusitis in these irradiated patients. The relative frequency with which various pathogens cause rhinosinusitis in these patients is unknown. This study investigates the bacteriology of acute rhinosinusitis in irradiated NPC patients by maxillary sinus puncture. From October 2001 through July 2006, 20 irradiated NPC patients with radiograph-proven acute maxillary sinusitis received maxillary sinus punctures. Aspirate contents of the sinuses were collected for aerobic and anaerobic cultivation. A total sampling of 26 sides was performed in the 20 patients. The culture rate was 85%. Frequently identified aerobes and facultative anaerobes included alpha-hemolytic streptococcus (n = 8), Staphylococcus aureus (n = 5) and Pseudomonas aeruginosa (n = 3). Streptococcus pneumoniae, Haemophilus influenzae and Moraxella catarrhalis, however, are far less common. This may provide important information about the antibiotic therapy in irradiated NPC patients with acute rhinosinusitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nasopharyngeal carcinoma (NPC) is a common cancer in Taiwan [1]. When diagnosed at stage I and II, more than 70 percent of these patients can survive after external beam radiotherapy [2], which is the current mainstay of therapy for the disease. The administration of radiation, however, inevitably causes damage to adjacent tissues from the base of the skull to the lower neck, and numerous complications may arise from this treatment. Rhinosinusitis is one of these complications. Failure to treat these patients with medical therapy, including standard antibiotics, is not uncommon, and becomes an enormous challenge to physicians.
It is well known that irradiation to the nasopharynx and nearby structures can cause irreversible damage to the sinonasal mucosa. An impaired mucociliary clearance of the nasal mucosa has been demonstrated in most irradiated NPC patients [3]. Different patterns of bacterial infections might occur in damaged sinonasal mucosa than in that of normal individuals. However, the microbiology of rhinosinusitis in irradiated NPC patients is not well established. This study investigates the organisms present in the maxillary sinus of irradiated NPC patients with radiograph-proven acute maxillary sinusitis by performing a maxillary sinus puncture.
Patients and methods
Subjects
The study was performed on irradiated NPC patients with acute maxillary sinusitis who presented to the otolaryngological department of Chung Shan Medical University Hospital from October 2001 to July 2006. External beam radiotherapy was delivered over a period of 7 weeks (5 days per week), with a median cumulative dose to the nasopharynx of 73 (range 70–76) Gy. Adjuvant chemotherapy consisting of cisplatin and 5-fluorouracil was given in 18 patients. All of the patients were regularly followed-up and did not show any evidence of residual or recurrent disease. Patients were considered for inclusion if they presented with typical symptoms of sinusitis (purulent nasal drainage, nasal congestion, and facial pain) for less than 4 weeks, as defined by Lanza and Kennedy [4]. All of these patients were confirmed to have maxillary sinusitis by radiographic abnormalities (sinus clouding or air-fluid level). Patients with a history of antibiotic administration in the previous 1 week or manifestations of recurrent chronic rhinosinusitis were excluded from the study. The patients were informed with treatment options including administration of empirical antibiotics and maxillary sinus puncture for bacterial culture and immediate drainage. There were 20 patients (12 men, 8 women) who were willing to undergo maxillary sinus puncture in the study. Informed consents were obtained from all patients with a detailed form that was in accordance with the standards of the ethics committee at Chung Shan Medical University.
Sample collection
Sterile gauze drenched in decongestant and anesthetic solution (1:100,000 epinephrine and 10% cocaine) was introduced to the common and inferior meatus for 20 min. Secretions were aspirated from the nasal cavities and nostrils were disinfected with povidone-iodine and 75% alcohol. Maxillary sinus was tapped by a sterile sinus trocar through the lateral wall of the inferior meatus, followed by aspiration of contents of the sinus into a 15 ml syringe. If no material could be aspirated, irrigation with saline was performed and the consequent aspiration was collected. Care was taken not to touch the vestibular epithelium by all instruments to minimize contamination. Samples from the sinus puncture were sent to the microbiological laboratory within 1 h.
Laboratory methods
In the microbiology laboratory, aerobic specimens were plated on blood agar plate, eosin methylene blue agar, and chocolate agar, cultured for 24 h at 35°C in an incubator containing 5% CO2. Anaerobic cultivation was performed using Brucella agar with Vitamin K1, hemin, PEA agar with phenylethyl alcohol agar and 5% Sheep’s Blood and incubated anaerobically (5% CO2 + 10% H2 + 85% N2). Plates were examined for growth of bacterial colonies at 24 and 48 h of incubation. Isolated organisms were identified using standard techniques. Potentially pathogenic organisms that grew on culture were reported semi-quantitatively with the following scale: <1+, rare; 1+, few; 2+, moderate; and 3+, many.
Results
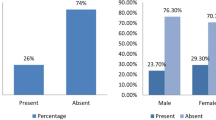
Twenty patients were enrolled in the study. The mean age of the 12 men and 8 women was 47.5 years (range 22–69 years). The time between completion of radiotherapy to maxillary sinus puncture ranged from 6 months to 21 years, with a mean of 4.9 years. Fourteen of the patients presented with unilateral maxillary sinusitis and six patients had bilateral maxillary sinusitis. Abnormalities revealed by sinus radiograph included air-fluid level in 10 maxillary sinuses and clouding in 16 maxillary sinuses, and thus a total sampling of 26 sides was performed in the 20 patients. The demographic, radiographic and culture results for each patient are shown in Table 1. There were no complications in any patient undergoing maxillary sinus puncture.
Of the 26 samples, 22 recovered one or more organisms. The culture rate was 85%. Aerobes and facultative anaerobes were recovered from 18 specimens, obligate anaerobes alone from 1 specimen, and mixed aerobes and anaerobes from 3 specimens. The most frequently identified aerobes and facultative anaerobes were alpha-hemolytic streptococcus (8/26, 31%) and Staphylococcus aureus (5/26, 19%). Other common aerobic bacteria recovered from these specimens included Pseudomonas aeruginosa (3/26, 12%) and Streptococcus constellatus (2/26, 8%). The cultured obligate anaerobes were peptostreptococcus and prevotella, both were identified at the same frequency (2/26, 8%). Among 6 patients who had bilateral diseases and received punctures of both maxillary sinuses, 3 patients had same pathogens recovered from both maxillary sinuses, including alpha-hemolytic streptococcus, P. aeruginosa and S. constellatus. One patient had alpha-hemolytic streptococcus recovered from left side and no bacteria recovered from right side. The other two patients had different bacteria recovered from bilateral maxillary sinuses (one side grew alpha-hemolytic streptococcus and the other grew S. aureus). Distribution of bacterial growth in the maxillary secretions is shown in Table 2.
Discussion
NPC is a prevalent malignancy in Southeast Asia, including China, Hong Kong and Taiwan. The current mainstay therapy for NPC is external beam irradiation to the nasopharynx and the neck. To deliver a curative dose of radiation to the tumor site, part of the nasal cavities, sphenoid, ethmoid and maxillary sinuses are included in the treatment field. Although recent advances in radiotherapy techniques have helped to reduce complications associated with treatment without jeopardizing the locoregional control rate, many patients still develop sinonasal complications after completion of radiation therapy. In a single-institutional study of irradiated NPC patients, chronic rhinosinusitis was found to be one of the most common untoward effects [5]. Although there is no literature on the incidence of acute rhinosinusitis in irradiated NPC patients, the entity is among the most common problems encountered by these patients and becomes one of the major reasons they search for medical counseling.
Although an obstructed ostiomeatal complex (OMC) is the major cause of rhinosinusitis in most individuals, there seem to be other pathophysiological causes responsible for the rhinosinusitis of irradiated NPC patients. Endoscopic examination of the nasal cavity in these patients revealed atrophic turbinates and wide sinus ostia, especially those of the maxillary and sphenoid sinuses [3]. Although atrophic change of the turbinates were not seen frequently in the patients of our study, endoscopic examinations did not demonstrate pathological mucosa, such as granulation tissue or polypoid mucosa, which obliterated the middle meatus. This indicates that obstruction of the OMC is not a common condition in irradiated NPC patients, and the cause underlying rhinosinusitis in these patients is most likely due to an impaired mucociliary clearance. In a series of studies comprising nine elderly patients irradiated for nasal carcinoma, impairment of nasal mucociliary clearance was found by using the saccharin transport test [6]. Similarly, a decreased mucociliary clearance and longer mucociliary transport times in the irradiated children with head and neck cancers were demonstrated by the saccharin/charcoal test [7]. The abnormal mucociliary clearance found in these irradiated patients is primarily related to radiation damage to the sinonasal epithelium, as demonstrated by a study involving electromicroscopic examination of the OMC mucosa in irradiated NPC patients. The study reported delayed irradiation effects on the nasal epithelium, including ciliary loss, dysmorphic cilia, and intercellular and intracellular vacuolation [8]. Electromicroscopic study of the mucosa of the middle meatus in one of our patients (patient number 1, 2 years after radiotherapy) also revealed a similar picture (Fig. 1). It is, however, unclear that different microbiologic agents may cause rhinosinusitis in irradiated NPC patients because of a damaged sinonasal mucosa in these patients.
Our study demonstrates the bacteriological features of acute maxillary sinusitis in irradiated NPC patients. The predominant aerobes and facultative anaerobes recovered from maxillary sinus secretions are alpha-hemolytic streptococcus and S. aureus. Alpha-hemolytic streptococcus and S. aureus are among the commensal flora in the nasal cavities and sinuses of healthy adults [9–11], suggesting that in the condition of impaired mucociliary clearance, these bacteria may become pathogenic and cause rhinosinusitis in NPC patients. The next common pathogen recovered from maxillary sinus secretions in our study is Pseudomonas aeruginos, a frequent microbiologic agent that causes infections in the situations of defective immunity. The impaired mucociliary function in the irradiated patients may provide such a milieu for the growth of P. aeruginos.
Contamination by non-pathogenic bacteria during the sampling process remains an important issue when alpha-hemolytic streptococcus were recovered and considered to be pathogenic for rhinosinusitis. In the eight maxillary sinus secretions with growth of alpha-hemolytic streptococcus, five samples were taken directly from the aspirate contents, while the other three from irrigation saline. This indicated that the cultivation of alpha-hemolytic streptococcus in our study stands for true analysis of maxillary contents rather than contamination during the process of maxillary sinus irrigations. Furthermore, our culture results should reflect limited, if any, contamination during sampling because of the zero recovery rate of coagulase-negative staphylococci, whose growth stands as a testimony for sampling contamination [12, 13].
As to members of the ‘infernal trio’ of community-acquired acute rhinosinusitis (S. pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis) [14], these are seldom recovered from maxillary secretions of these patients. Actually, there was only one S. pneumoniae, one H. influenzae, and one M. catarrhalis recovered from 26 specimens out of these 20 patients. Although the role of commensal flora as true pathogens in the pathogenesis of rhinosinusitis remains controversial, severe infections by these bacteria are not uncommon in many parts of the human body, especially in the status of an impaired immunity [15]. It is probable that the virulence of the organisms does not play a major role in the development of rhinosinusitis in these damaged sinonasal mucosa. Instead, commensal flora with lower virulence can readily cause inflammation and become pathogenic because of an impaired mucociliary function of the sinuses in these irradiated patients. Although our finding that S. pneumoniae, H. influenzae and M. catarrhalis do not predominate in the acute maxillary sinusitis of irradiated NPC patients might be the result of failure to exclude recurrent chronic maxillary sinusitis from the study population, all the patients denied typical symptoms of rhinosinusitis, such as purulent nasal drainage and nasal blockage, in the preceding months. Moreover, if part of the sample represented isolates from recurrent chronic maxillary sinusitis, there should be more anaerobic bacteria recovered in the study.
Like most other series performed on non-irradiated adults [16], our study also found a relatively low frequency of anaerobic bacteria isolated in acute maxillary sinusitis in irradiated NPC patients. This finding also suggests that poor drainage and increased intranasal pressure, a condition favoring the growth of anaerobes, are not marked in the maxillary sinus of these irradiated patients.
Among the sampling methods used to investigate the pathogens responsible for rhinosinusitis, maxillary sinus puncture is considered the gold standard for obtaining bacterial cultures [17]. Although the procedure is painful and more aggressive, and carries some risk of complications—such as bleeding, eyeball injury, and subcutaneous emphysema—it is rather safe when performed by an experienced otolaryngologist. In our series, all 20 patients tolerated the procedure well and none of them suffered any complications. Although there is increasing body of evidence that the culture results of endoscopic middle meatus sampling correlates well with those of maxillary sinus punctures [18, 19], the former sampling method may carry a higher risk of contamination, especially in some anatomic conditions of the nasal cavity. For instances, a deviated nasal septum and paradoxical middle turbinates may interfere with the sampling of sinus purulence from the middle meatus under endoscopic guidance. In addition, bacterial growth of the endoscopic sampling correlates well with that of maxillary sinus punctures only when a culture is made directly from the frank purulence [19]. In many instances, however, there were only scarce amounts of purulent discharge in the middle meatus to obtain even when radiographs of the sinus demonstrated definite pictures of rhinosinusitis. Therefore, the culture data from maxillary sinus punctures is more reliable and provides invaluable information in studying the bacteriology of rhinosinusitis. By the culture results of maxillary sinus punctures, we have been able to select appropriate treatment for each patient. In 2 patients who had P. aeruginos recovered and 2 patients who had penicillin-resistant S. aureus recovered, quinolones were prescribed according to the results of sensitivity test. As to 3 patients whose sinus secretions showed no bacterial growth, no antimicrobial agent was given. Also by performing maxillary sinus punctures, many patients reached prompt resolution of their sinonasal symptoms and some were still free of rhinosinusitis at their monthly follow-up. This is probably thanks to effective elimination of the accumulated pus and the immediate aeration of the maxillary sinus.
To prevent development of systemic metastases, 18 of these patients (except patient no. 4 and 5) received chemotherapy, which consisted of cisplatin and 5-fluorouracil. The inclusion of chemotherapy in the treatment of NPC might raise the concern of an altered microbiology of rhinosinusitis by these antineoplastic agents. However, both agents have plasma half-life less than an hour, and are excreted out of human body within days, and because the study was performed at least 6 months after completion of treatments, a time long enough for complete washout of antineoplastic agents and regeneration of sinonasal epithelial cells, the chemotherapy should have limited effect, if any, on the bacterial population of paranasal sinuses.
Because of the small patient number in the current study, these preliminary results must be confirmed by longer and more studies in order to establish the relative frequency with which bacteria causes acute rhinosinusitis in irradiated NPC patients.
Conclusion
In conclusion, we found that sinonasal commensal flora, such as alpha-hemolytic streptococcus and Staphylococcus aureus, are the major bacteria involved in acute rhinosinusitis of irradiated NPC patients, while S. pneumoniaea, Haemophilus influenza and Moraxella catarrhalis, which are the predominant pathogens of community-acquired sinusitis, are far less common. This may provide important information regarding antimicrobial therapy in irradiated NPC patients with acute maxillary sinusitis
References
Hsu MM, Tu SM (1983) Nasopharyngeal carcinoma in Taiwan. Clinical manifestations and results of therapy. Cancer 52:362–368
Heng DM, Wee J, Fong KW et al (1999) Prognostic factors in 677 patients in Singapore with nondisseminated nasopharyngeal carcinoma. Cancer 86:1912–1920
Kamel R, Al-Badawy S, Khairy A et al (2004) Nasal and paranasal sinus changes after radiotherapy for nasopharyngeal carcinoma. Acta Otolaryngol 124:532–535
Lanza DC, Kennedy DW (1997) Adult rhinosinusitis defined. Otolaryngol Head Neck Surg 117:S1–S7
Zubizarreta PA, D’Antonio G, Raslawski E et al (2000) Nasopharyngeal carcinoma in childhood and adolescence: a single-institution experience with combined therapy. Cancer 89:690–695
Stringer SP, Stiles W, Slattery WH 3rd et al (1995) Nasal mucociliary clearance after radiation therapy. Laryngoscope 105:380–382
Surico G, Muggeo P, Mappa L et al (2001) Impairment of nasal mucociliary clearance after radiotherapy for childhood head cancer. Head Neck 23:461–466
Lou PJ, Chen WP, Tai CC (1999) Delayed irradiation effects on nasal epithelium in patients with nasopharyngeal carcinoma. An ultrastructural study. Ann Otol Rhinol Laryngol 108:474–480
Brook I (1981) Aerobic and anaerobic bacterial flora of normal maxillary sinuses. Laryngoscope 91:372–376
Klossek JM, Dubreuil L, Richet H et al (1996) Bacteriology of the adult middle meatus. J Laryngol Otol 110:847–849
Jiang RS, Liang KL, Jang JW et al (1999) Bacteriology of endoscopically normal maxillary sinuses. J Laryngol Otol 113:825–828
Gordts F, Halewyck S, Pierard D et al (2000) Microbiology of the middle meatus: a comparison between normal adults and children. J Laryngol Otol 114:184–188
Rombaux P, Collet S, Hamoir M et al (2005) The role of nasal cavity disinfection in the bacteriology of chronic sinusitis. Rhinology 43:125–129
van Cauwenberge PB, Vander Mijnsbrugge AM, Ingels KJ (1993) The microbiology of acute and chronic sinusitis and otitis media:a review. Eur Arch Otorhinolaryngol 250:S3–S6
Su WY, Liu C, Hung SY, Tsai WF (1983) Bacteriological study in chronic maxillary sinusitis. Laryngoscope 93:931–934
Brook I (2004) Microbiology and antimicrobial management of sinusitis. Otolaryngol Clin North Am 37:253–266, v–vi
Carenfelt C, Lundberg C, Nord CE et al (1978) Bacteriology of maxillary sinusitis in relation to quality of the retained secretion. Acta Otolaryngol 86:298–302
Vaidya AM, Chow JM, Stankiewicz JA et al (1997) Correlation of middle meatal and maxillary sinus cultures in acute maxillary sinusitis. Am J Rhinol 11:139–143
Vogan JC, Bolger WE, Keyes AS (2000) Endoscopically guided sinonasal cultures: a direct comparison with maxillary sinus aspirate cultures. Otolaryngol Head Neck Surg 122:370–373
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hsin, CH., Tsao, CH., Su, MC. et al. Bacteriology of acute rhinosinusitis in nasopharyngeal carcinoma survivors: a result of maxillary sinus punctures. Eur Arch Otorhinolaryngol 264, 1157–1162 (2007). https://doi.org/10.1007/s00405-007-0334-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-007-0334-9