Abstract
This study aimed to evaluate the efficacy and safety of single-session radiofrequency tongue base reduction (RTBR) combined with uvulopalatopharyngoplasty (UPPP) for the treatment of obstructive sleep apnea syndrome (OSAS). Sixty-six patients with multilevel obstruction underwent single-session RTBR combined with UPPP. Snoring, Epworth sleepiness scale (ESS) and polysomnography were used to assess outcome before and 6 months after treatment. Sixty-six patients completed this study. Snoring level significantly decreased from 8.0 to 4.3. The mean ESS score significantly decreased from 11.4 to 7.5. The mean apnea–hypopnea index decreased significantly from 22.9 to 13.9. The overall success rate of the single-session RTBR combined with UPPP was 53.6%. Postoperative AHI in 50% of patients was normalized (AHI < 5). The success rates for patients with mild, moderate and severe OSAS were 62.5, 46.2 and 57.1%, respectively. There were two adverse effects, one ulceration of the tongue base and one transient taste change. Single-session RTBR combined with UPPP is an effective and safe treatment for OSAS patients with multilevel obstruction. It could be considered as first treatment for OSAS patients with multilevel obstruction, independent of the severity of OSAS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea syndrome (OSAS) is very frequent and is increasingly recognized as a major health problem [1]. OSAS results in significant morbidity, mortality, and cost to society as a result of a twofold to sevenfold increased risk of motor vehicle accidents [2]. OSAS may also result in cardiovascular disease, quality of life deficits and performance deficits from loss of alertness [3–5].
Nasal continuous positive airway pressure (CPAP) is considered the gold standard and the primary treatment for OSAS; however, the therapeutic use of nasal CPAP is seriously limited by low long-term compliance [6]. Although a variety of surgical techniques have been described to manage OSAS, multilevel pharyngeal surgery is required to overcome collapse at multiple levels of the pharyngeal airway.
Several surgical techniques such as uvulopalatopharyngoplasty (UPPP), uvulopalatal flap and radiofrequency-induced thermotherapy of the soft palate have been widely used for the treatment of velopharyngeal obstruction in OSAS. Available tongue base procedures that alleviate obstruction of the lower pharynx include mandibular osteotomy with genioglossus advancement, maxillomandibular advancement (MMA), partial midline tongue resection and hyoidthyroidpexia. These approaches, especially MMA, can be very effective in treating severe OSAS. However, these techniques require long hospitalization and appear to result in high postoperative morbidity and thus remain held in reserve for severe OSAS.
Radiofrequency tongue base reduction (RTBR) was first introduced in 1999 by Powell et al. [7] as a minimally invasive technique for OSAS. Several studies showed improvement in objective and subjective OSAS features [8–13]; however, these approaches have the limitation that they require several sessions. In this study, we present our results of single-session RTBR combined with UPPP for the treatment of OSAS with multilevel obstruction.
Methods
Sixty-six patients diagnosed with OSAS and both velopharyngeal and retrolingual collapses enrolled in the present study. No patient had previous velopharyngeal or lingual surgery. Patients were evaluated preoperatively and 6 months postoperatively by history taking, administering a questionnaire, physical examination, cephalometry, fiberoptic nasopharyngoscopy and polysomnography. Retropalatal and retrolingual obstructions were determined by physical examination, cephalometry and fiberoptic nasopharyngoscopy in all patients. Patients who had only a single-level retropalatal obstruction or only a retrolingual obstruction were not included in the present study. All patients with multilevel obstruction underwent RTBR combined with UPPP in one stage. This study was approved by our institutional review board.
Questionnaire
Snoring scores were subjectively evaluated with the help of the bed partners using a traditional 10 cm visual analogue scale (VAS) ranging from 0 (no snoring) to 10 (severe snoring/bed partner leaves the room). Daytime sleepiness was evaluated with the Epworth sleepiness scale (ESS).
Physical examination
All patients underwent a full head and neck examination. The body mass index (BMI), a rank for obesity and important criterion for OSAS, was calculated by dividing weight (kg) by the square of height (m2). Friedman [12] staging was applied. Tonsil size was graded 0–4. Friedman palate position was graded 1–4. Stage I was defined as those patients with palate position I or II, tonsil size 3 or 4 and BMI of less than 40. Stage II was defined as palate position I or II with tonsil size 0, 1 or 2 or palate position III and IV with tonsil size 3 or 4 and BMI of less than 40. Stage III was defined as palate position III or IV with tonsil size 0, 1 or 2 and BMI of less than 40. All patients with a BMI of greater than 40 were included in stage IV.
Cephalometry
Patients were seated with their heads oriented in the Frankfort horizontal plane and stabilized with a head holder. Patients were instructed to place their teeth in habitual occlusion, keeping the mouth closed and the tongue relaxed on the floor of the mouth. Exposures were taken at the end of expiration.
The following five parameters were obtained preoperatively: posterior airway space (PAS), the minimal distance between the tongue base and the posterior pharyngeal wall; PNS-P, the distance from the posterior nasal spine to the lowest point on the soft palate; mandibular plane to hyoid (MP-H), the distance from the mandibular plane to the most anterosuperior point of the hyoid bone; SNA, angle formed by intersection of lines drawn from sella to nasion and nasion to subspinale; and SNB, angle formed by intersection of lines drawn from sella to nasion and nasion to supramentale. Craniofacial abnormalities were defined as the SNA < 79° and/or SNB < 77°. RTBR was indicated as PAS < 11 mm and MP-H > 15 mm.
Fiberoptic nasopharyngoscopy
Nasopharyngoscopy was performed with the subjects in the supine position after being given topical nasal anaesthesia. A flexible nasopharyngoscope was inserted through the nasal cavity to the hypopharynx. Measurements were taken during a maximal inspiratory effort against a closed mouth and occluded nose [Mueller’s maneuver (MM)]. During examination, airway size was assessed separately in both the retropalatal (upper pharynx) and retroglossal (tongue base and supraglottic) segments. Collapse during MM was rated using the following classification: 1+, 0–25%; 2+, 26–50%; 3+, 51–75%; and 4+, >76%. RTBR was indicated as retrolingual collapse during MM > 50%.
Polysomnography
All patients underwent a one-night polysomnographic study at the hospital. The polysomnographic study included an electroencephalogram (C3/A1, C4/A2, O1/A1, O2/A2), electro-oculogram, chin and leg electromyogram and electrocardiogram. Respiration was measured by oronasal airflow, thoracic and abdominal movements by inductive plethysmography and oxyhaemoglobin saturation by pulse oximetry. Apnea was defined as the absence of airflow for more than 10 s, with hypopnea being a decrease of 50% or more in airflow associated with greater than 4% decline in oxygen saturation. The apnea–hypopnea index (AHI) denotes the total numbers of apneic plus hypopneic events divided by total sleep time in hours. Subjects were divided according to the AHI in simple snorers (AHI < 5) with mild sleep apnea being an AHI of 5–15; moderate sleep apnea, an AHI of 15–30; and severe sleep apnea, an AHI greater than 30. The patients whose AHI > 5 with daytime symptoms or AHI > 15 underwent surgical treatment.
Surgical procedure
Uvulopalatopharyngoplasty was carried out in a similar manner to Li’s technique [14]. Tonsillectomy was performed first. The oral soft palate mucosa and submucosa were debrided and the palatopharyngeus, palatoglossus and uvula muscles were preserved as much as possible. The uvular tip was trimmed. The palate was then reflected anteriorly and superiorly and the anterior and posterior tonsillar pillars were trimmed and reoriented to create a more retropalatal airway space.
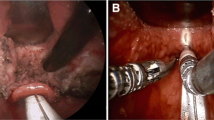
RTBR was performed using a CelonLab ENT (Celon AG Medical Instruments, Berlin, Germany) with a hand-held disposable bipolar electrode probe (CelonProSleep®). Because the RTBR was combined with the UPPP, general anaesthesia was required. The surface of the tongue was disinfected with 0.5% chlorhexadine. A mixture of normal saline and 1% lidocaine with 1:200,000 epinephrine was infiltrated around the middle of the circumvallate papillae to enhance the effect of radiofrequency. Nine application sites were selected. Three lesions were at the midline of the circumvallate papillae and 1 cm anterior and posterior to the middle of the circumvallate papillae. The next six lesions were 1 cm right and left of the first three lesions (Fig. 1). A power setting on the power control unit was 10 W. The probe at each application site was inserted perpendicularly at depth of 15 mm. The application time varied between 4 and 6 s per puncture and was terminated by acoustic ‘end-indication’ and an autostop facilitated by a thermister and tissue impedance measurement at the probe tip. The delivery energy at this power setting was about 60 J per punctum.
Postoperative care
All patients received antibiotics intravenously for 2 days postoperatively and then orally for 2 weeks. Oral painkillers and steroid were administered routinely. Patients were usually discharged 2 days postoperatively.
Statistics
All statistical analyses were performed using SPSS for Windows Version 11.5 (SPSS, Inc, Chicago, IL). Preoperative and postoperative parameters were compared using paired t tests. Success rates according to the severity of OSAS and Friedman stage were compared using the χ2 test. Statistical significance was accepted at P < 0.05.
Results
Sixty-six patients with OSAS who underwent RTBR combined with UPPP completed this study. There were 58 men and 8 women. The ages ranged from 23 to 64 years (mean age ± SD: 44.7 ± 10.6). The BMI of the patients was 27.6 ± 3.4 kg/m2. Thirty-one patients were classified as stage II and 35 patients as stage III according to the Friedman staging system. Patient characteristics are shown in Table 1.
Subjective assessment of the patients was carried out preoperatively and at 6 months postoperatively (Table 2). Postoperative values for ESS and snoring level were significantly reduced after the treatment for both stage II and III patients.
A total of 56 of 66 patients underwent postoperative PSG. There were 22 and 34 patients in stages II and III, respectively. Comparison of preoperative and postoperative polysomnographic data are presented in Table 3. The AHI for the total subjects decreased significantly from 22.9 ± 14.7 to 13.9 ± 18.7. The AHI in the supine position decreased significantly from 30.0 ± 17.3 to 19.0 ± 22.8. The apnea index (AI) also decreased significantly from 14.4 ± 11.5 to 4.4 ± 7.6. Mean oxygen saturation increased from 92.6 ± 4.2 to 94.1 ± 1.6% (P > 0.05). The lowest oxygen saturation increased from 79.1 ± 5.7% to 79.4 ± 16.5% (P > 0.05). The portion of slow wave sleep increased from 3.2 ± 3.1 to 4.5 ± 4.4% (P > 0.05). Total sleep time and sleep efficiency did not change substantially before and after treatment. The mean BMI (27.4 ± 3.2 kg/m2) at the time of the postoperative PSG did not significantly vary from its preoperative value.
A successful outcome was defined as a postoperative AHI < 20 with at least a 50% reduction from the preoperative level. In this study, 30 patients (53.6%) met the criteria for a successful outcome. And above all, postoperative AHI in 28 patients (50%) was normalized (AHI < 5). Dividing patients into groups according to Friedman stage, the success rate for stage II and III patients was 72.7 and 41.2%, respectively, and the differences between stage II and III patients were not statistically significant. When divided by the severity of OSAS, the success rates for patients with mild OSAS, moderate OSAS and severe OSAS were 62.5, 46.2 and 57.1%, respectively, and the differences among the groups were not statistically significant.
No postoperative complications such as infections, abscesses, haematomas or airway obstruction occurred. One patient had an ulceration of the tongue base that resolved within 1 week. One patient complained of a taste change that resolved within 3 months.
Discussion
After the first report by Powell et al. [7], there have been several studies addressing radiofrequency surgery of the tongue base. In most of these studies, several sessions with a small number of lesions per session were performed [7–12]. There is only one report that describes a higher number of lesions in a single-session [15]. However, it was a study of treatment of primary snoring. Our study is the first study to evaluate the effect of single-session RTBR combined with UPPP in the treatment of OSAS.
We used bipolar application technology. A standardized coagulation effect on the tongue base tissue is very important, as the hypoglossal nerve and neurovascular bundle may be damaged if the lesions are too large. The probe tip with the bipolar arrangement of electrodes in the needle eliminates these risks. The radiofrequency power is adapted to the current condition of the tissue during the coagulation process and overdosing or even carbonization can be avoided as the power input is best suited to the desired treatment result as a function of each moment in time [13]. This system reduced application times, averaging 6 s per puncture and had a lower energy (60 J per lesion), which reduced the damage to neighbouring tissue.
Sher et al. [16] reported previously that a patient population without tongue base obstruction demonstrated a 42% UPPP success rate. The success rate was 5% in patients with tongue base obstruction [16]. Woodson et al. [17] reported that 20% of OSAS patients responded to radiofrequency volumetric tissue reduction in a multi-institutional study. Fischer et al. [8] reported that 33% of patients were treated successfully by multilevel temperature-controlled radiofrequency therapy. Stuck et al. [9] and Steward [10] demonstrated success rates of multilevel radiofrequency surgery in 33 and 59% of patients, respectively. The mean numbers of treatment session per patient were 2.7 and 4.2, respectively [9, 10]. Nelson combined two subsequent temperature-controlled radiofrequency tongue reductions with UPPP in patients with multilevel obstruction and had an improved response rate (50% success rate) [11]. In our study, the success rate in all subjects was 53.6%. And above all, 28 of 30 patients was physiologically cured (postoperative AHI < 5). Li et al. [14] reported that the overall success rate of the modified UPPP for patients who were judged to have a narrowed retropalatal space was 82%. Friedman et al. [12] reported that UPPP demonstrated a success rate of 37.9% in Friedman stage II patients and 8.1% in stage III patients and in stages II and III patients treated with UPPP plus tongue base radiofrequency reduction, success rates were 74.0 and 43.8%, respectively. Among these patients 59.3% were operated upon with a one times tongue base radiofrequency reduction, with the others receiving a maximum of six procedures. In our study, the success rate was 72.7 and 41.2% in stage II and III patients, respectively. It is difficult to compare our results with other studies; however, our results, performed in a single-session, were similar to those in studies reported previously. Our surgical procedure was easier for the patients as it was a single-session procedure. In addition, our method has an advantage that is, the short time required because, we used the CelonLab system. Skeletal surgeries were performed on patients in whom success was not achieved; these results will be reported later.
Friedman et al. [18] reported that the success rates of UPPP for patients with mild, moderate and severe OSAS were 26.7, 42.5 and 26.5, respectively, and that patients with mild OSAS do not have a better chance of successful treatment than patients with severe OSAS. Li et al. [19] reported that the success rate for UPPP using a severity-based staging system was similar. When divided by the severity of OSAS, our success rates did not differ between the groups. We think that this technique can be applied to all patients independent of the severity of the OSAS.
Pazos and Mair reported on four patients with temporary tongue base neuralgia, two with tongue base abscesses formation and two with floor of mouth oedema with airway compromise in 25 cases of tongue base radiofrequency ablation [20]. Other authors have shown RTBR to be a safe procedure with reported adverse event rates between 0 and 8.8% [8–10, 17]. In studies using CelonLab, Herder et al. [13] reported that two patients had a mild and transient tongue deviation and one patient had a paresis of the hypoglossal nerve. Welt et al. [15] did not observe any postoperative complications. We observed two adverse effects (3.6%). These lesions healed without sequelae.
This study has several limitations. Various analysis to find obstruction level analysis were done under awakening conditions which were not ideal and Mueller maneuver is highly disputed, but definite method to find obstruction sites have not been known. In addition, 10 of 66 were missed for follow-up PSG for reason of expense or time. When they were compared to the others, their characteristics were not different and the results overall might not be affected by them.
Conclusion
Single-session RTBR combined with uvulopalatalpharyngoplasty is an effective treatment for reducing symptoms and AHI in OSAS patients with multilevel obstruction. It is also a safe treatment because of minimal postoperative morbidity and complication. Radiofrequency tongue base surgery has been described by others; however, the advantages of this procedure are a simple, short procedure time and the bipolar technique. It could be considered first treatment for OSAS patients with multilevel obstruction, independent of the severity of OSAS.
References
Flemons WW (2002) Clinical practice. Obstructive sleep apnea. N Engl J Med 347:498–504
Young T, Blustein J, Finn L, Palta M (1997) Sleep-disordered breathing and motor vehicle accidents in a population-based sample of employed adults. Sleep 20:608–613
Peker Y, Hedner J, Norum J, Kraiczi H, Carlson J (2002) Increased incidence of cardiovascular disease in middle-aged men with obstructive sleep apnea: a 7-year follow-up. Am J Respir Crit Care Med 166:159–165
Flemons WW, Tsai W (1997) Quality of life consequences of sleep disordered breathing. J Allergy Clin Immunol 99:S750–S756
Valencia-Flores M, Bliwise DL, Guilleminault C, Cilveti R, Clerk A (1996) Cognitive function in patients with sleep apnea after acute nocturnal nasal continuous positive airway pressure (CPAP) treatment: sleepiness and hypoxemia effects. J Clin Exp Neuropsychol 18:197–210
Meurice JC, Dore P, Paquereau J et al (1994) Predictive factors of long term compliance with nasal continuous positive airway pressure treatment in sleep apnea syndrome. Chest 105:429–433
Powell NB, Riley RW, Guilleminault C (1999) Radiofrequency tongue base reduction in sleep-disordered breathing: a pilot study. Otolaryngol Head Neck Surg 120:656–664
Fischer Y, Khan M, Mann W (2003) Multilevel temperature-controlled radiofrequency therapy of soft palate, base of tongue, and tonsils in adults with obstructive sleep apnea. Laryngoscope 113:1786–1791
Stuck BA, Starzak K, Verse T, Hormann K, Maurer JT (2003) Complications of temperature-controlled radiofrequency volumetric tissue reduction for sleep-disordered breathing. Acta Otolaryngol 123:532–535
Steward DL (2004) Effectiveness of multilevel (tongue and palate) radiofrequency tissue ablation for patients with obstructive sleep apnea syndrome. Laryngoscope 114:2073–2084
Nelson LM (2001) Combined temperature controlled radiofrequency tongue reduction and UPPP in apnea surgery. Ear Nose Throat J 80:640–644
Friedman M, Ibrahim H, Joshph NJ (2004) Staging of obstructive sleep apnea/hypopnea syndrome: a guide to appropriate treatment. Laryngoscope 114:454–459
den Herder C, Kox D, van Tinteren H, de Vries N (2006) Bipolar radiofrequency induced thermotherapy of the tongue base: its complication, acceptance and effectiveness under local anesthesia. Eur Arch Otorhinolaryngol 263:1031–1040
Li HY, Chen NH, Shu YH, Wang PC (2004) Changes in quality of life and respiratory disturbance after extended uvulopalatal flap surgery in patients with obstructive sleep apnea. Arch Otolaryngol Head Neck Surg 130:195–200
Welt S, Maurer JT, Hörmann K, Stuck BA (2007) Radiofrequency surgery of the tongue base in the treatment of snoring—a pilot study. Sleep Breath 11:39–43
Sher AE, Schechtman KB, Piccirillo JF (1996) The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 19:156–177
Woodson BT, Nelson L, Mickelson S, Huntley T, Sher A (2001) A multi-institutional study of radiofrequency volumetric tissue reduction for OSAS. Otolaryngol Head Neck Surg 125:303–311
Friedman M, Vidyasagar R, Bliznikas D, Joseph NJ (2005) Does severity of obstructive sleep apnea/hypopnea syndrome predict uvulopalatopharyngoplasty outcome? Laryngoscope 115:2109–2113
Li HY, Wang PC, Lee LA, Chen NH, Fang TJ (2006) Prediction of uvulopalatopharyngoplasty outcome: anatomy-based staging system versus severity based staging system. Sleep 29:1536–1541
Pazoa G, Mair EA (2001) Complications of radiofrequency ablation in the treatment of sleep-disordered breathing. Otolaryngol Head Neck Surg 125:462–467
Conflict of interest statement
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Eun, Y.G., Kim, S.W., Kwon, K.H. et al. Single-session radiofrequency tongue base reduction combined with uvulopalatopharyngoplasty for obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol 265, 1495–1500 (2008). https://doi.org/10.1007/s00405-008-0688-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-008-0688-7