Abstract
Ectopic meningiomas located within the external auditory canal without any intracranial connection are an extremely rare finding. A report is made of a 38-year-old woman presenting with a conductive hearing loss due to an aural polyp, which was subsequently diagnosed as a meningioma. Computer-aided tomography (CT) and magnetic resonance imaging (MRI) showed the tumour to be entirely extracranial. Complete tumour excision was achieved using a modified radical mastoidectomy approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ectopic meningiomas located within the external auditory canal without any intracranial connection are an extremely rare finding. A report is made of a 38-year-old woman presenting with a conductive hearing loss due to an aural polyp, which was subsequently diagnosed as a meningioma. Computer-aided tomography (CT) and magnetic resonance imaging (MRI) showed the tumour to be entirely extracranial. Complete tumour excision was achieved using a modified radical mastoidectomy approach.
Case report
A 38-year-old woman was referred to the Otolaryngology department complaining of an 8-month history of right-sided hearing loss, tinnitus and a sensation of fullness in the right ear. Her past medical history was unremarkable except for a superficial spreading melanoma excised from the scalp earlier in the year. Clinical examination confirmed a tender polypoid mass within the external auditory canal, the rest of the examination was normal. Pure tone audiometry revealed a conductive hearing loss of the order of 30–40 dB.
Examination under anaesthesia revealed a large, soft tissue mass extending from the posterior-superior meatal wall and obscuring the tympanic membrane; the mass appeared separate from the tympanic membrane. Several biopsies were taken.
Histopathological examination of the specimen showed syncitial nests of isomorphic epithelioid cells undermining keratinising squamous epithelium in a permeative fashion. They were arranged as focally confluent groups in a swirling pattern. Individual cells were plump with indistinct cytoplasmic borders. There was modest vascularity with no mitoses or necrosis. The appearance suggested a meningioma of transitional cell pattern (Fig. 1).
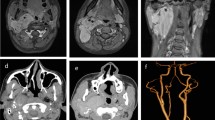
A CT scan (Fig. 2) confirmed the presence of a faintly calcified soft tissue mass within the external auditory canal. A secondary middle ear effusion and inflammatory changes involving the mastoid air cell system were noted. There was no evidence of bony erosion or of a defect in the floor of the middle cranial fossa. MRI scan (Fig. 3) demonstrated an enhancing lesion on post-contrast T1-weighted images within the external auditory canal; no intra-cranial connection could be demonstrated.
The patient eventually underwent an exploration of the right ear. The mass was found to originate from the post-superior meatal wall and extend into the attic region. It had passed medial to the incus and head of malleus and obstructed the additus. The ossicular chain, fallopian canal and otic capsule were intact, and no defect was detected in the tegmen. A modified radical mastoidectomy was performed to allow complete resection of the tumour. The incus and head of malleus were removed to facilitate tumour excision; the chorda tympani was embedded within the tumour and subsequently sacrificed. The incus was replaced in the mastoid cavity with a view to future ossiculoplasty. Histologic examination of the specimen confirmed the original diagnosis. The patient's postoperative recovery was unremarkable, and on subsequent follow-up the patient remained asymptomatic with no evidence of tumour recurrence.
Discussion
Meningiomas account for 13–18% of all primary intra-cranial neoplasms. Extension of these tumours into the external auditory canal from intracranial or skull based sites is recognised [6]. However, ectopic meningiomas without any intracranial connection located primarly within the external auditory canal are an extremely rare finding [1, 2, 3, 7, 10].
Two theories have postulated the origin of ectopic meningiomas. Majoros [5] suggested that they may originate from pinched off embryonal arachnoid cells outside the skull and vertebrae that lie along fusion lines of primitive bones and nerve sheaths. Shuanshoti and Panyathana [8] thought they may occur as a result of differential maturation of pluripotential mesenchymal cells. The finding of arachnoid granulations along nerve sheaths and the bony sulci of the temporal bone lends weight to the former theory.
Most cutaneous meningiomas arise in the scalp, face or paravertebral region in children and young adults [4]. Those reported to occur primarily in the external auditory canal have followed a generally benign course [6]. It is important to distinguish them from lesions that occur more frequently in the region. Schwannomas, paragangliomas, squamous cell carcinomas and adenexal tumours can all present in the region. The benign course of meningiomas compared to the potentially more aggressive course of some of the other tumours has important implications with regard to intervention. Fortunately, most meningiomas described at this site demonstrate a typical histologic picture [5].
Histologically, extracranial meningiomas do not differ greatly from their neuraxial counterparts. Like the majority of intracranial meningiomas they tend to show a female predominance and generally have a fairly benign clinical course. Four variants are recognised: (1) meningotheliomatous or syncytial, (2) transitional or psammomatous, (3) fibrous and (4) angioblastic [9]. The extracranial group are most often reported to be the transitional or meningotheliomatous type. In this particular case the transitional variant was diagnosed.
The mainstay of treatment is complete surgical excision, the type of operation employed is dependent on the extent of the tumour. Preoperative evaluation with high quality radio-imaging is imperative to delineate tumour extent and detect any intracranial extension. We opted for a modified radical mastoidectomy to ensure complete tumour clearance and to allow adequate access for future surveillance.
Because of the indolent growth of meningiomas, long-term follow-up is recommended to detect any local recurrence and to exclude any intracranial disease even after an apparently extracranial meningioma is removed. Rietz et al. recommend yearly follow-up with CT scans for at least 10 to 15 years; Tsunoda and Fukaya suggest MRI may provide more information for surveillance [7].
References
Chen KTK, Dehner LP (1978) Primary tumours of the external and middle ear. A clinicopathologic study of 14 paragangliomas and three meningiomas. Arch Otolaryngol 104: 253–259
DeWeese DD, Everts EC (1972) Primary intratympanic meningioma. Arch Otolaryngol 96: 62–66
El-Ghazali TMS (1981) Primary intra-tympanic meningioma. J Laryngol Otol 95: 849–852
Hu B, Pant M, Cornford M, Walot I, Peng SK (1998) Association of primary intracranial meningioma and cutaneous meningioma of external auditory canal. A case report and review of the literature. Arch Pathol Lab Med 122: 97–99
Majoros M (1970) Meningioma of the paranasal sinuses. Laryngoscope 80: 640–645
Prayson RA (2000) Middle ear meningiomas. Ann Diagn Pathol 4: 149–153
Rietz DR, Ford CN, Brandenberg JH, Kurtycz DF, Hafez GR (1983) Significance of apparent intratympanic meningiomas. Laryngoscope 93: 1397–1404
Shuanshoti S, Panyathana R (1973) Ectopic meningiomas. Arch Otolaryngol 98: 102–105
Tsunoda R, Fukaya T (1997) Extracranial meningioma presenting as a tumour of the external auditory meatus: a case report. J Laryngol Otol 111: 148–151
Zeitouni AG, Zagzag D, Cohen NL (1997) Meningioma of the internal auditory canal. Ann Otol Rhinol Laryngol 106: 657–661
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uppal, H.S., Kabbani, M., Reddy, V. et al. Ectopic extra-cranial meningioma presenting as an aural polyp. Eur Arch Otorhinolaryngol 260, 322–324 (2003). https://doi.org/10.1007/s00405-003-0582-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-003-0582-2