Abstract
Purpose
The aim was to follow-up two cohorts of women with GDM to investigate the incidence and time of diagnosis of manifest diabetes mellitus (DM) postpartum and identify the risk factors for diabetes in our population.
Methods
A follow-up study on two independent cohorts having oral glucose tolerance test (OGTT) in 1991/1992 and 2011–2016: Cohort 1 consisted of 406 women including 54 with GDM and 352 with a non-GDM OGTT-test and cohort 2 had 433 women diagnosed with GDM. The first cohort had nearly 25 years of follow-up and gave information on magnitude, conversion rate and type of diabetes manifestation. The second cohort was started recently to evaluate whether newer diagnostic criteria and baseline information on the old cohort are still valid for prediction of diabetes risk.
Results
The risk of manifest diabetes in cohort 1 at the end of follow-up was six times higher in women with previous GDM compared with non-GDM (RR = 6; 95% CI 4–11). We observed a 70% diabetes rate 25 years after pregnancy. Only family history of diabetes in cohort 2 was associated with conversion to manifest diabetes (p = 0.002), also after adjustment for age, BMI, non-Danish origin and smoking during pregnancy (p < 0.001)
Conclusion
The incidence of diabetes after GDM is higher than that previously reported in Scandinavian populations and the rate of manifest diabetes rises steeply 15 years after pregnancy and after 40 years of age. The women of cohort 2 with recent GDM are at risk of DM at a higher rate. On this background our results are useful in identifying the time where GDM women may benefit from the effective implementation of evidence-based treatment to postpone and advert manifest DM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gestational diabetes mellitus (GDM) has a prevalence ranging from 2 to 22% worldwide depending on the population and type of diagnostic test and the women with GDM are at risk of impaired glucose tolerance (IGT) and diabetes mellitus (DM) later in life [1,2,3,4]. Kjos et al. advocated use of early postpartum screening to rule out manifest diabetes found during pregnancy and found that any degree of glucose intolerance after pregnancy was as strong a predictor for future diabetes as GDM itself [5]. The global increase in the prevalence of diabetes emphasizes the need to reexamine and update the assessment of the risk of subsequent diabetes after GDM.
Major randomized trials in women with prior GDM support lifestyle intervention for prevention diabetes postpartum but implementation of these measures is challenging at best [6,7,8,9,10]. Metformin is effective in prevention of diabetes, though to a lesser degree. The participation is low in postpartum lifestyle intervention programs due to the lack of guidelines for modification and motivation for healthier lifestyle in public campaigns together with a paucity of knowledge on the risk of later onset of diabetes after GDM [10,11,12,13]. The participation rate was a mere 27% in the Tianjin GDM Prevention Program [14]. While most agree in the notion that women with prior GDM should be offered lifestyle intervention programs, it remains obscured when the time for enrollment for such intervention is optimal and whether a time window exists for prevention, beyond which the benefits of participation in lifestyle modification programs may be diminished [11].
Our department is involved in a feasibility study in women with previous GDM to identify the barriers for interventions with the purpose to improve compliance and setting the goals for what is practical and achievable [15, 16]. To balance the cost of such programs, the magnitude and timing of potential diabetes needs to be outlined and updated. With this background, the purpose of this study was to follow-up on two cohorts of women with GDM and to investigate the incidence of manifest DM postpartum and to identify the risk factors for conversion. The first cohort has nearly 25 years of follow-up and gives information on magnitude, speed and type of diabetes manifestation. The second cohort was started recently to evaluate whether newer criteria and baseline information on the old cohort are still valid for prediction of diabetes risk.
Methods
A follow-up was performed on two independent cohorts having oral glucose tolerance test (OGTT) in 1991/1992 and 2011–2016: Cohort 1 consisted of 406 women hereof were 54 with GDM and 352 with a non-GDM OGTT-test and cohort 2 had 433 women diagnosed with GDM. The Danish Data Protection Agency approved the project (nos. 1-16-02-824-17, 1-16-02-825-17, and 1-16-02-180-17), which was conducted in accordance with the Helsinki Declaration and the guidelines for Good Clinical Practice.
The screening indications were similar in the two cohorts except that in cohort 2 women with a diagnosis of polycystic ovary syndrome were included: Maternal pre-pregnancy body mass index (BMI) ≥ 27 kg/m2, family disposition of diabetes, previous GDM, multiple pregnancy, previous macrosomia (birth weight ≥ 4500 g), stillbirths and glucosuria. The diagnosis was made with a 2-h 75 g OGTT initial test at gestational week 10–20 and later at week 28 if the primary test was normal. In cohort 1 the criterion for GDM was at least two capillary plasma glucose values, measured at a seven point OGTT, exceeding the threshold values 6.4 mmol/l (fasting), 13.6 mmol/l (30 min), 13.7 mmol/l (60 min), 11 mmol/l (90 min), 10.2 mmol/l (120 min), 9.7 mmol/l (150 min), and 8.5 mmol/l (180 min). Cohort 2 was diagnosed based on threshold glucose values at 120 min of venous plasma or capillary whole blood ≥ 9 mmol/l or ≥ 10 mmol/l in capillary plasma.
Beside medical nutrition therapy, all women with GDM had ambulatory visits where a medical endocrinologist and a diabetes nurse assessed the glycemic regulation every second week from diagnosis.
The current recommendation for follow-up postpartum is an OGTT-test at their general practitioner (GP) three to four months after delivery and screening every third year. For diabetes diagnosis glycosylated hemoglobin (HbA1c) ≥ 48 mmol/mol (former level ≥ 6.5%), fasting plasma blood glucose levels of ≥ 7.0 mmol/l or 2-h glucose values ≥ 11.1 mmol/l at 75 g OGTT.
Hospital data were collected from the electronic hospital charts together with laboratory data, medications and prescriptions in current or previous use. We registered age, height, pre- and post-pregnancy weight, co-morbidity, and parity. Further on, screening indication, date of diagnosis of GDM, treatment received (none, diet and/or insulin), gestational age, birth weight, length, and head circumference. Blood samples were registered: HbA1c, mean glucose, 2-h glucose at 75 g OGTT and fasting blood glucose at the time of diagnosis during pregnancy and the last sample before giving birth. Postpartum the most recent glucose evaluation and the values at diabetes diagnosis were used. We excluded any duplicate, second pregnancies of women delivering more than once during 2011–2016 (n = 23).
The original cohorts were slightly reduced due to lack of follow-up data: Cohort 1 originally consisted of 406 women, but seven women had emigrated with no further trace at all, hereof were two women with former GDM, leaving 399 for evaluation for postpartum diabetes. Cohort 2 consisted of 433 GDM women, but six women emigrated with no trace in our records leaving 427 women.
We studied the total of glucose measurements available and the national prescription registry: Sixty-four women in cohort 2 had no follow-up glucose data, yet, and in cohort 1 further two had since delivery and sometime of follow-up emigrated and two women had died. The diabetes diagnosis of these women was ascertained and none of the 64 women of cohort 2 had any prescription on anti-diabetes drugs. The same applied for the four women from cohort 1 who either died or emigrated later. Their non-diabetic status was locked to the last known date; this was either the date of death or the last date when a note was made either in the laboratory results or prescription database. We categorized a woman with manifest diabetes if fasting glucose was above 7.0 mmol/l, 2-h OGTT value ≥ 11.1 mmol/l or a HbA1c ≥ 48 mmol/mol. Impaired glucose tolerance (IGT) was defined as fasting glucose of 6–7 mmol/, 2-h value at OGTT of 9–11 mmol/l or a HbA1c of 42–47 mmol/mol.
Statistical analysis
To test for difference between two variable means, the Student’s t test was applied if data followed a Gaussian distribution; otherwise Mann–Whitney’s U test was used. For three means ANOVA was used. If ANOVA was significant, Newman-Keul's post-hoc test was applied to identify the group that was significantly deviating from the mean. Proportions were tested in χ2 test and 95% confidence intervals (95% CI) were calculated using https://vassarstats.net/. The continuous variables age, glucose at OGTT (fasting and 2-h glucose), follow-up time were subjected to Kaplan–Meier analysis with the cohorts, GDM diagnosis during pregnancy and DM diagnosis after pregnancy as group variable. Log-rank test was applied for significance testing. Cox regression analysis was performed on the outcome of manifest diabetes with age, BMI, smoking and parity as continuous covariates and the categorical variables of screening indications and non-Danish origin. Follow-up times are given as median (range). When crude rates of diabetes incidence are reported the calculation uses the original, larger cohort in the denominator. Statistical analyses were conducted using the statistical software program IBM SPSS Statistics 20. Data are given as mean ± SD if they followed a Gaussian distribution; if not, median (range) are indicated. A two-sided p value of < 0.05 was chosen as the level of significance.
Results
The demographic characteristics were similar in women with GDM in both cohorts, whereas the non-GDM women turned out to be younger and weighing less (Table 1). The majority of women in both cohorts were overweight (cohort 1: non-GDM 70%; GDM: 72%; cohort 2: GDM 64%). Women with GDM in cohort 1 had higher BMI and age at delivery than women with non-GDM in cohort 1 (p < 0.05). Women had higher BMI when diagnosed with GDM in both cohort 1 and 2 than the non-GDM women of cohort 1 whereas those with GDM had similar BMI (Table 1).
The majority of the women were screened (in order of prevalence) due to obesity, family history and GDM in a previous pregnancy. Women screened due to glucosuria were absent in cohort 2 whereas the women with an age above 38 years at pregnancy were more prominent. Besides that, women in cohort 1 and 2 were similar according to weight, age at delivery, parity, and screening inclusion criteria at OGTT, except in the youngest cohort 2, non-Danish origin was more prominent and women smoked less. Furthermore, the prevalence of previous GDM tended to be higher among women in cohort 2 (Table 1).
Gestational week and child anthropometrics turned out similar in women with GDM in cohort 1 and 2 (Table 2). The non-GDM women delivered one week later than the GDM women (p < 0.001). In cohort 2, a total of 63 women (15%) were treated with insulin. We have no consistent information about insulin treatment during pregnancy of women cohort 1.
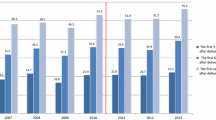
The cohorts were subjected to postpartum follow-up at different levels: In cohort 1, most of the women were followed-up at the obstetrical ward, in particular those with previous GDM, and in cohort 2 all follow-up was performed at their GP (data not shown). After more than 20 years of follow-up 85 women in cohort 1 were diagnosed with diabetes; hereof 79 with type 2 and six with type 1 diabetes mellitus (Table 3). Five years after pregnancy the diabetes rate was 8% and 7% in the women with GDM from cohort 1 and 2, respectively (Fig. 1). The risk of being diagnosed with diabetes was six times higher in women with previous GDM compared with non-GDM women in cohort 1 (RR = 6.1; 95% CI 3.5–10.6) adding up to an accumulated diabetes rate of almost 70% 25 years after pregnancy. The rate of manifest diabetes rises sharply after 40 years of age (Fig. 2). The median age of those diagnosed with diabetes was similar at the end of follow-up in the two subgroups of cohort 1 (48–51 years, Table 3).
Diabetes incidence in women with previous gestational diabetes (GDM) compared to women with normal oral glucose tolerance test during pregnancy (non-GDM). Non-GDM: women with normal oral glucose tolerance test during pregnancy in 1991/1992; GDM-cohort 1: gestational diabetes in 1991/92, GDM-cohort: gestational diabetes 2011–2016; GDM-cohort 1 and GDM-cohort 2 vs. non-GDM: both p < 0.001
Diabetes incidence by age in women with previous gestational diabetes (GDM) compared to women with normal oral glucose tolerance test during pregnancy (non-GDM). Non-GDM: women with normal oral glucose tolerance test during pregnancy in 1991/1992; GDM-cohort 1: gestational diabetes in 1991/1992, GDM-cohort: gestational diabetes 2011–2016; GDM-cohort 1 and GDM-cohort 2 vs. non-GDM: both p < 0.001
The women with previous GDM displayed 2.7% yearly average rate of diagnosis of manifest diabetes. The conversion rate was only 1% in cohort 2, which hereby mimicked the observed rate from the first 12 years postpartum in GDM women of cohort 1 (Fig. 1). After that time the incidence rate of diabetes rose dramatically above the non-GDM women. These only had a 0.5% rate of developing manifest diabetes over 25 years. By that time the rate picked up in speed and rose steeply 15 years after pregnancy. Concomitantly, the incidence of diabetes increased dramatically above that of the non-GDM women. Type 1 diabetes was diagnosed at a similar rate in all groups (Table 3).
None of the maternal screening criteria in both cohorts were associated with conversion to manifest diabetes except from family history of diabetes in cohort 2 (p = 0.002). Adding age, BMI, non-Danish origin and smoking during pregnancy to the analysis did not alter the association (Cox regression, p < 0.001).
Discussion
Our rate of manifest diabetes mellitus after GDM was much higher than expected and previous reported in Scandinavian populations [4, 17]. In other studies conversion rates varied between 2.6–70% depending on the population studied and the length of follow-up lasting from 6 weeks to 28 years after pregnancy [4]. The majority reported on GDM turning to manifest type 2 diabetes in populations with higher rates of type 2 diabetes than in Scandinavia. Lauenborg et al. found 40% DM after 10 years in a Danish population and, typical for Denmark, a high proportion being type 1 diabetes, namely 11% [17]. Follow-up attendance was a moderate 64% probably because the study focused on diagnosing the particular type of diabetes, the presence of IGT and autoantibodies. This may have biased the incidence of type 1 diabetes and with higher risk of DM than in the non-attending women. At 10 years follow-up in our cohort the cumulative incidence of diabetes was only 13% (Fig. 1); this low figure may be due to detection bias. The screening practices shifted from hospital-based to GP follow-up between the two cohorts and, thus, delayed the DM diagnosis differently. On the other hand, we only lost about 1% to follow-up from the original cohorts and, with similar relative incidence of type 1 diabetes to type 2 diabetes in all subgroups including the non-GDM, the DM diagnosis seems minimally biased by diagnostic criteria and setting of affirming the diagnosis. As our study reports the highest rate of DM reported in a Scandinavian follow-up we wonder if the diagnostic criteria included only the women with high risk of DM or that we have missed potential GDM women at screening with subsequent low risk. However, the similar median age at DM diagnosis in cohort 1 irrespective of GDM does not support that hypothesis, either (Fig. 2, Table 3). It seems unlikely that any ‘missing’ women with a risk would be amongst those with pre-pregnant risk factors and not screened with OGTT; if this were to be substantial, then a difference in cohort 1 between GDM and non-GDM would be expected,. The newest cohort 2 follows the exact footpath of the older cohort and tells what is in wait for the women involved, although we cannot be sure that it reaches similar levels due to the historic cohort design. Similarly, we found that the distribution of type 2 vs. type 1 diabetes was similar in both cohorts and with 30% lower prevalence of type 1 diabetes than Lauenborg et al. so we conclude that less selection bias was present.
A seven-fold risk of manifest diabetes after GDM was reported by Bellamy et al. reaching over a 25 year period, very similar to our study [18]. Populations of non-Scandinavian origin displayed many different and almost uniformly higher rates of type 2 diabetes compared to people of Scandinavian origin. We intended to adjust for a potential population bias by adding our non-GDM women with similar risk factors for diabetes. They, indeed, exhibited a similar background risk at screening except from slightly lower BMI. In line with this intended screening bias, our non-GDM women were prone to develop DM to a larger extent compared to the total national diabetes incidence, namely 14% vs 4.5%) [19] (Table 3, Fig. 1). Thus, even these women from cohort 1 comprise a group with a moderate risk of future DM on top of the high risk GDM women.
To postpone and advert manifest DM evidence-based treatment has been outlined and GDM women could potentially benefit. However, the timing and which intervention method would be most cost-effective remains unsettled [15, 16]. Our study may be useful in differentiating the timing as diet, exercise, and metformin need motivation and enough time to be implemented. The rate of manifest diabetes rose sharply after 40 years of age (Fig. 2). The median age of those diagnosed with diabetes was similar at the end of follow-up in the two subgroups of cohort 1 (48–51 years, Table 3). On this background our results are useful in identifying the time where GDM women may benefit from the effective implementation of evidence-based treatment to postpone and advert manifest DM. Moreover, the time frame to do so appears to be broad enough to differentiate and intensify at several time points.
Overweight and obesity is associated with development of diabetes later on. These risk factors were part of the screening criteria and, thus, were biased in that direction. Despite that the childbearing age and the population’s body weight had increased between the time of cohort 1 and 2, we found no difference in demographic characteristics between GDM women [4]. This may be due to the limited number of women or the change in the diagnostic test for GDM. Our prevalence of GDM has remained stable over the years, indicating no selection toward any difference in screening or metabolism between the cohorts. At further analysis, however, a family history of diabetes did turn out to be an independent predictive factor for the newest cohort, which included more GDM women but with a short observation time, pointing to the limits for analysis in cohort 1.
It seems that the conversion rate of cohort 2 follows the cohort 1 but we cannot preclude a more diabetes-prone background in the women of any cohort, yet. Any difference that may show up cannot easily be explained in screening and diagnostic test. We, therefore, conclude that the women of cohort 2 are at high risk of DM and should receive counseling and intervention on this aspect. Again, we lack data on physical activity, lipid profile, and alcohol consumption at baseline and further on, while smoking was accounted for during pregnancy, but not later on. Confounders like these are known to influence the rate of GDM and later DM [20].
At follow-up in the postpartum period no uniform data were available on glycemic control and treatment. Lack of follow-up postpartum was reported in several studies and seems to be a universal issue due to several causes [21,22,23]. The most common barrier reported was lack of time by patients [24]. Primary care providers have described that the main problems are lack of patients attendance, inconclusive guidelines, patient inconvenience [25] and poor communication with specialists [26, 27]. What factors influences the attendance to DM screening are somewhat inconclusive [27].
The diagnosis at 25 years may be biased by some misclassification as only the type and timing of medical treatment was available, which in most cases could be combined with glycemic measurements. For subtle diagnostic reasons hospital charts and GP’s notes should be scrutinized for verification of type of diabetes and further diagnosis. We had multiple blood glucose results available for women with manifest DM leaving no doubt on diagnosis. A number of women lacked glucose data postpartum and missing data impact the results in different ways. For one, the reasons for follow-up were unknown but we may hint at those with less follow-up and no medicine in the national prescription database are less likely to have any un-detected illness. Secondly, we acknowledge the potential risk of overlooking diabetes in our population as estimation of undiagnosed diabetes runs as high as 40%, corresponding to 200.000 people in Denmark at age 20–79 years [19]. The missing data would, however, confirm that our figures may be a conservative estimate of the risk in the GDM women, diet- and insulin treated alike, as diabetes is no rare outcome to be overlooked.
The severity of GDM seems to have an impact on postpartum screening. In accordance with other studies, insulin treatment and high glucose levels during pregnancy was associated with an increased glucose testing postpartum and higher diabetes detection rate [5, 17, 23].
The main limits of this study are its retrospective, follow-up design and the relatively modest sample size for detection of DM diagnosis. The registration of drug prescription and diagnostic data in the national registries and electronic data charts is lacking on a minimal scale and is surveyed systematically under the auspices of the National Health Authority [28]. The loss of follow-up may have resulted in a minimal higher incidence rate at the end of follow- up but this is mirrored in the increased variation of the Kaplan–Meier analysis.
Conclusion
The incidence of diabetes after GDM reaches considerable 70% after 25 years and the rate of manifest diabetes rises steeply 15 years after pregnancy and after 40 years of age. This may have been overlooked previously. The newly diagnosed GDM women may follow a similar path and should be targeted with evidence-based diabetes preventive interventions.
References
Cho GJ, An JJ, Choi SJ, Oh SY, Kwon HS, Hong SC, Kwon JY (2015) Postpartum glucose testing rates following gestational diabetes mellitus and factors affecting testing non-compliance from four tertiary centers in Korea. J Korean Med Sci. https://doi.org/10.3346/jkms.2015.30.12.1841
Jeppesen C, Maindal HT, Kristensen JK, Ovesen PG, Witte DR (2017) National study of the prevalence of gestational diabetes mellitus among Danish women from 2004 to 2012. Scand J Public Health. https://doi.org/10.1177/1403494817736943
Kim M, Park J, Kim SH, Kim YM, Yee C, Choi SJ, Oh SY, Roh CR (2018) The trends and risk factors to predict adverse outcomes in gestational diabetes mellitus: a 10-year experience from 2006 to 2015 in a single tertiary center. Obstet Gynecol Sci. https://doi.org/10.5468/ogs.2018.61.3.309
Kim C, Newton KM, Knopp RH (2002) Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care. https://doi.org/10.2337/diacare.25.10.1862
Kjos SL, Peters RK, Xiang A, Henry OA, Montoro M, Buchanan TA (1995) Predicting future diabetes in Latino women with gestational diabetes. Utility of early postpartum glucose tolerance testing. Diabetes. https://doi.org/10.2337/diab.44.5.586
Dabelea D, Snell-Bergeon JK, Hartsfield CL, Bischoff KJ, Hamman RF, McDuffie RS (2005) Increasing prevalence of gestational diabetes mellitus (GDM) over time and by birth cohort: Kaiser Permanente of Colorado GDM Screening Program. Diabetes Care. https://doi.org/10.2337/diacare.28.3.579
Pan XR, Li GW, Hu YH et al (1997) Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care 20:537–544. https://doi.org/10.2337/diacare.20.4.537
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM (2002) Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. https://doi.org/10.1056/NEJMoa012512
Tuomilehto J, Lindstrom J, Eriksson JG et al (2001) Finnish diabetes Prevention Study. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. https://doi.org/10.1056/NEJM200105033441801
Benhalima K, Jegers K, Devlieger R, Verhaeghe J, Mathieu C (2016) Glucose Intolerance after a recent history of gestational diabetes based on the 2013 WHO Criteria. PLoS ONE. https://doi.org/10.1371/journal.pone.0157272
Vääräsmäki M (2016) Is it worth treating gestational diabetes: if so, when and how? Diabetologia. https://doi.org/10.1007/s00125-016-3976-6
Ferrara A, Peng T, Kim C (2009) Trends in postpartum diabetes screening and subsequent diabetes and impaired fasting glucose among women with histories of gestational diabetes mellitus: a report from the Translating Research Into Action for Diabetes (TRIAD) Study. Diabetes Care. https://doi.org/10.2337/dc08-1184
Di Cianni G, Ghio A, Resi V, Volpe L (2010) Gestational diabetes mellitus: an opportunity to prevent type 2 diabetes and cardiovascular disease in young women. Womens Health (Lond). https://doi.org/10.2217/whe.09.76
Hu G, Tian H, Zhang F et al (2012) Tianjin Gestational Diabetes Mellitus Prevention Program: study design, methods, and 1-year interim report on the feasibility of lifestyle intervention program. Diabetes Res Clin Pract. https://doi.org/10.1016/j.diabres.2012.09.015
Nielsen KK, Grunnet LG, Maindal HT (2018) Prevention of Type 2 diabetes after gestational diabetes directed at the family context: a narrative review from the Danish Diabetes Academy symposium. Diabet Med. https://doi.org/10.1111/dme.13622
Timm A, Nielsen KK, Maindal HT (2018) Complex intervention research for families with prior gestational diabetes mellitus. Ugeskr Laeger 180(45) (pii: V03180168. PMID: 30404712)
Lauenborg J, Hansen T, Jensen DM et al (2004) Increasing incidence of diabetes after gestational diabetes: a long-term follow-up in a Danish population. Diabetes Care. https://doi.org/10.2337/diacare.27.5.1194
Bellamy L, Casas JP, Hingorani AD, Williams D (2009) Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. https://doi.org/10.1016/S0140-6736(09)60731-5
The National Diabetes Registry (Det Nationale diabetes register, in Danish). https://diabetes.dk/presse/diabetes-i-tal/diabetes-i-danmark.aspx. Accessed Oct 2019
Risk Factors for Type 2 Diabetes National Institute of Diabetes and Digestive and Kidney Disease: U.S Department of Health and Human Services; 2016. https://www.niddk.nih.gov/health-information/diabetes/overview/risk-factors-type-2-diabetes. Accessed Oct 2019
Butalia S, Donovan L, Savu A, Johnson J, Edwards A, Kaul P (2017) Postpartum diabetes testing rates after gestational diabetes mellitus in Canadian women: a population-based study. Can J Diabetes. https://doi.org/10.1016/j.jcjd.2016.12.013
Nouhjah S, Shahbazian H, Amoori N, Jahanfar S, Shahbazian N, Jahanshahi A, Cheraghian B (2017) Postpartum screening practices, progression to abnormal glucose tolerance and its related risk factors in Asian women with a known history of gestational diabetes: a systematic review and meta-analysis. Diabetes Metab Syndr. https://doi.org/10.1016/j.dsx.2017.05.002
Hunt KJ, Logan SL, Conway DL, Korte JE (2010) Postpartum screening following GDM: how well are we doing? Curr Diab Rep. https://doi.org/10.1007/s11892-010-0110-x
Keely E, Clark H, Karovitch A, Graham I (2010) Screening for type 2 diabetes following gestational diabetes: family physician and patient perspectives. Can Fam Physician 56(6):558–63. https://www.cfp.ca/content/56/6/558.long(PMID: 20547525)
Aroda VR, Christophi CA, Edelstein SL et al (2015) Diabetes Prevention Program Research Group. The effect of lifestyle intervention and metformin on preventing or delaying diabetes among women with and without gestational diabetes: the Diabetes Prevention Program outcomes study 10-year follow-up. J Clin Endocrinol Metab. https://doi.org/10.1210/jc.2014-3761
Tovar A, Chasan-Taber L, Eggleston E, Oken E (2011) Postpartum screening for diabetes among women with a history of gestational diabetes mellitus. Prev Chronic Dis 8(6):A124. https://www.cdc.gov/pcd/issues/2011/nov/11_0031.htm(PMID:22005617 PMCID: PMC3221566)
Nielsen KK, Kapur A, Damm P, de Courten M, Bygbjerg IC (2014) From screening to postpartum follow-up - the determinants and barriers for gestational diabetes mellitus (GDM) services, a systematic review. BMC Pregnancy Childbirth. https://doi.org/10.1186/1471-2393-14-41
Lynge E, Sandegaard JL, Rebolj M (2011) The Danish national patient register. Scand J Public Health. https://doi.org/10.1177/1403494811401482
Funding
This study was not funded by any grants.
Author information
Authors and Affiliations
Contributions
KAA data verification and qualification, manuscript writing. HMA data collection and verification, manuscript editing. UP data collection and manuscript editing. RAK protocol development and manuscript editing. FFL project idea and implementation, registration and legal applications, data analysis and manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Ethical approval
The Danish Data Protection Agency approved the project (Nos. 1-16-02-824-17, 1-16-02-825-17 and 1-16-02-180-17) and the ethical standards were in line with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The original approvals are enclosed together with permission to internals addition of data from one cohort study to the other which is covered by the running permission no 621549 and belongs to the approval no 1-16-02-824-17. The regions umbrella permission further covers retrospective follow-up studies as long as no single person is identifiable and thus anonymous. The handling of data and expression by the Gynecology Dept, Herning of conforming with personal data law is further expressed by the Data handling agreement no. 509 with the National Health Authority. All above correspondences are added in originals to the submission. This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aagaard, K.A., Al-Far, H.M., Piscator, U. et al. Manifest diabetes after gestational diabetes: a double-cohort, long-term follow-up in a Danish population. Arch Gynecol Obstet 302, 1271–1278 (2020). https://doi.org/10.1007/s00404-020-05669-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05669-1