Abstract
Background and objectives
To compare effectiveness and safety of dinoprostone, misoprostol and Cook’s balloon as labour-inducing agents in women with intrauterine growth restriction (IUGR) at term.
Methods
Retrospective cohort chart review of women diagnosed with foetal growth restriction at term in Reina Sofia Hospital, Cordoba, Spain from January 2014 to December 2015. Registration of baseline characteristics and method of induction was made. The main outcome was time from induction to delivery. Obstetric and perinatal outcomes were also collected.
Results
A total of 99 women were diagnosed with IUGR in the mentioned period. Of them, 21 women were induced with dinoprostone [dinoprostone group (DG)], 20 with misoprostol (MG) and in 58 with Cook’s balloon (CG). Groups were homogeneous regarding pre-induction Bishop score and parity. The CG required more time (24.36 vs. 19.23 h; p = 0.02) and more oxytocin dose for conduction of labour from induction to delivery (6.75 vs. 1.24 mUI; p < 0.01) than DG. Moreover, the CG also needed more oxytocin than MG, 6.75 vs. 2.37 mUI (p < 0.001). Caesarean rate was 5, 14.9 and 17.3% in MG, DG and CG, respectively. No differences were observed in rates of uterine tachysystole, non-reassuring foetal status and neonatal adverse events.
Interpretation and conclusions
Prostaglandins were more effective than Cook’s balloon to induce labour and achieve vaginal birth in this sample of women with IUGR at term, with a similar safety profile.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Labour induction involves a complex set of interventions applied to artificial initiation of labour before its spontaneous onset with the purpose of achieving vaginal delivery [1]. Labour induction has shown benefits in selected cases including post-term pregnancies, premature rupture of membranes, maternal disease and intrauterine growth restriction (IUGR) [2].
Traditionally, induction of labour has been associated with an increased risk in operative delivery rates. Specifically, induction of labour for foetal indications significantly increases the risk of caesarean delivery in nulliparous women [3].
Amniotomy and stimulation with oxytocin are widely accepted methods for inducing labour. However, known risk factors as Bishop’s score ≤5 have been significantly associated with an increased rate of caesarean delivery [4]. Thus, pre-induction cervical ripening is required. Prostaglandins improve cervical maturation and increases successful vaginal delivery rates [5]. Nevertheless, it remains a concern on the safety profile of its use in conditions such as IUGR and in these cases, mechanical methods may play an important role [6].
Compared to prostaglandins, mechanical methods such as Cook’s balloon have lower risk of hyper stimulation with similar caesarean section rates [7]. For this reason, mechanical methods are particularly recommended in cases of high risk of impaired foetal well-being, such as IUGR. Therefore, the present study was designed to compare the effectiveness and safety of prostaglandin E1 and E2, misoprostol and dinoprostone, respectively, with Cook’s intracervical double balloon as labour-inducing agent in women with IUGR at term.
Methods
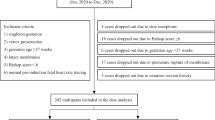
This retrospective cohort study was designed with the aim to compare dinoprostone 10 mg (Propess®, Ferring Pharmaceutical, Saint-Prex, Switzerland), misoprostol 25 mcg (Misofar®, Laboratorios Bial S.A) and the Cook’s intracervical balloon (Cook Cervical Ripening Balloon®, Cook Incorporated, IN, USA) for induction of labour in pregnancies with IUGR at term. Pregnant women diagnosed with IUGR at Reina Sofia Hospital, Cordoba, Spain during a period comprised from January 2014 to December 2015, were recruited. Approval for the study was obtained from the local research ethics committee. Study was conducted retrospectively, according to local protocols.
Women were eligible for inclusion if they met the following criteria: IUGR type I (≤3th percentile with normal foetal Doppler) and Bishop’s score <7. The exclusion criteria included history of previous caesarean section or major uterine surgery, non-reassuring foetal status (NRFS), low amniotic fluid index, chorioamnionitis, active infection in birth canal, premature rupture of membranes, third trimester metrorrhagia, multiple pregnancy and non-cephalic presentation. Complete and understandable information about the induction of labour was given to all women according to the usual protocol of this hospital, and each of them chose the induction method to be used.
Sample size was calculated using Granmo (sample size and power calculator. Version 7.12 April 2015). According to previous studies and accepting an alpha risk of 0.05 and a beta risk of 0.05, at least 16 subjects in the smaller group and 49 in the largest group are necessary to recognize as statically significant difference in time to delivery. A total of 99 women were consecutively selected in the period mentioned above. Twenty patients were induced with misoprostol (MG), 21 with dinoprostone (DG), and 58 with the Cook’s balloon (CG). According to local institution’s protocol, in the MG, a 25 mcg tablet was administered vaginally every 4 h, up to a maximum of 4 tablets within 24 h. In the DG, a 10 mg vaginal insert was placed in the posterior vaginal fornix for 24 h. The Cook’s balloon was introduced into the vagina, and both the intrauterine and intravaginal balloons were filled with 50 mL of saline solution. A cardiotocography monitoring was performed for 30 min during the administration of each method, and was repeated every 6 h in DG y CG. Oxytocin infusion was added if the active phase of labour (3 cm dilatation and 3–4 contractions every 10 min) was not achieved within 24 h of induction.
According to previous studies, the main variables included for analysis were time to induction, time to active labour, time to delivery and use of oxytocin. Intrapartum complications such as tachysystole, non-reassuring foetal status (NRFS), fever, and meconium were included. Episiotomy also was recorded. Type of delivery, reason for caesarean section, birth weight and neonatal status, including APGAR score at 1 and 5 min and postpartum pH, were also considered.
Statistical analysis
Data were collected retrospectively from the hospital electronic medical records and analysed using the G-Stat 2.0 free statistical software (Glaxo Smith Kline, Tres Cantos. Madrid). The ANOVA test was used for comparisons between quantitative variables and Chi-squared test was used for qualitative variables. A value of p < 0.05 was considered statistically significant.
Results
Among the 99 pregnant women diagnosed with type I IUGR at term included in the MG, DG, and CG groups, no differences were observed in the baseline characteristics at the time of the inclusion. Table 1.
The time elapsed between induction to delivery was 24.33 (±1.18) h for CG, 19.23 (±1.60) h for DG and 22.35 (±2.31) h for MG (p = 0.08). Thirty women in CG, eight women in MG and three women in DG required oxytocin infusion. A higher dose of oxytocin was required in the CG than in the prostaglandin groups (Table 2).
Only one case of caesarean section was recorded in the MG (5%), vs. 14.3% (n = 3) and 17.3% (n = 10) in DG and CG groups, respectively. Type of delivery, episiotomy and reasons for caesarean section are shown in Table 2.
Regarding perinatal outcomes, no differences were observed between the three groups including tachysystole, NRFS, meconium, intrapartum fever, postpartum haemorrhage, pH, Apgar scores or the rate of neonatal admissions.
Discussion
Labour induction is recommended when the risks of continuing pregnancy either for the mother or foetus, outweighs the advantages of an expectant management. Pevner emphasize the importance of selecting appropriate candidates to improve the success of labour induction [8]. When induction of labour involves IUGR foetuses a strict assessment of foetal well-being should be performed. Doppler assessment of the placental and foetal circulation and foetal biophysical profile to detect foetal hypoxia [9] are of crucial importance for decision-making. The Spanish guidelines, recommended induction of labour in type I IUGR foetuses after the 37th week of gestation. According to Rhinehart-Ventura, the use of a standardized induction protocol allows to reduce the rate of failed inductions and a minor length of labour [10]. Additionally, the Bishop score is also relevant in the prediction of induction success [11]. This variable, evaluated by the same team of gynaecologists, was homogeneous in our sample and may explain the lack of differences between the three groups.
Among the multiple alternatives for the induction of labour, misoprostol appears to be the most efficient compared with mechanical methods and even with other prostaglandins; however, the evidence of higher incidence of uterine hyper stimulation and tachysystole with prostaglandins [12, 13] arise concerns about foetal well-being, which is particularly relevant in IUGR foetuses [7, 14].
In a recent study, Chavakula et al. compared misoprostol and Foley catheter for labour induction in IUGR pregnancies. Misoprostol did not increase the incidence of tachysystole or abnormal foetal heart rate. Moreover, in this study misoprostol was found to be more effective in terms of time to delivery [15]. Our results are consistent with these studies, but not with the results of Hofmeyr study, where vaginal misoprostol was associated with increased uterine hyperstimulation [16]. Misoprostol has also been associated with an increased incidence of meconium-stained amniotic fluid comparing to dinoprostone [17]; but in our study, no differences were detected between the three methods analysed.
The incidence of intrapartum complications, neonatal outcomes and maternal morbidity were similar in all the groups. These data are consistent with the results of Culver, suggesting that misoprostol has a similar safety profile than mechanical methods [18]. Moreover, in the present study, the rate of neonatal admissions was lower in DG and MG although this may be explained by the small sample size, gestational age and greater birth weight at time of induction.
Time elapsed from induction to delivery, the rate of caesarean section and the incidence of chorioamnionitis were similar in the three groups. These data are consistent to Fox’s study [19, 20]. Although He considered the intracervical double balloon particularly recommendable for the labour induction in IUGR foetuses, this method did not reduce the rate of caesarean sections [21]. In our study, the rate of caesarean deliveries trended to be higher when the double balloon was used. Noteworthy in the He study, the double balloon increased the rate of infection; however, in our study the rate of intrapartum fever was comparable in all groups.
Women who had previously uterine surgery were not included in this study. Lydon-Rochelle’s and De Bonrostro’s studies found that double balloon may be an alternative safe and effective for the induction of women who have had prior caesarean deliveries, given the higher risk of uterine rupture [22, 23]. And in a recent paper, Kehl concludes that the sequential application of double-balloon catheter and vaginal PGE2 is as effective as the sole use of vaginal PGE2 with less applications and total amount of PGE2 [24]. In addition, the World Health Organization considered mechanical methods as a method of choice for labour induction in woman with previous caesarean section [25].
Cost associated to induction of labour must be another aspect to consider. In this direction, according to previous studies, misoprostol is postulated as the most cost-effective. As we observed in this study, this could be due to greater speed and safety with prostaglandins [26].
Like the most of available studies on this topic, the present one has several major limitations including the retrospective design of the study that difficult to stablish definitive conclusions and the lack of a large sample to establish which induction method is the most effective and safe for IURG pregnancies. It is clear that randomized and prospective studies are necessary. However, in spite of the retrospective data, the present study along with others may be useful for further meta-analysis.
Finally, in this study, prostaglandins were more effective regarding time to delivery and at least as safe as the Cook´s balloon, given the lack of differences in caesarean rates for NRFS [3 (14.29%) in DG, 0 (0%) in MG and 5 (8.62%) in CG, p = 0.23] and perinatal outcomes (no differences were observed between the three groups including pH, Apgar scores or the rate of neonatal admissions) for the induction of labour in foetuses with IUGR at term.
References
Lawani OL, Onyebuchi AK, Iyoke CA, Okafo CN, Ajah LO (2014) Obstetric outcome and significance of labour induction in a health resource poor setting. Obstet Gynecol Int 2014:419621
Mozurkewich E, Chilimigras J, Koepke E, Keeton K, King VJ (2009) Indications for induction of labour: a best-evidence review. BJOG 116(5):626–636
Parkes I, Kabiri D, Hants Y, Ezra Y (2016) The indication for induction of labor impacts the risk of cesarean delivery. J Matern Foetal Neonatal Med 29(2):224–228
Rijal P (2014) Identification of risk factors for cesarean delivery following induction of labour. J Nepal Health Res Counc 12(27):73–77
Kelly AJ, Malik S, Smith L, Kavanagh J, Thomas J (2009) Vaginal prostaglandin (PGE2 and PGF2a) for induction of labour at term. Cochrane Database Syst Rev 4:CD003101
Keirse MJ (2006) Natural prostaglandins for induction of labor and preinduction cervical ripening. Clin Obstet Gynecol 49(3):609–626
Jozwiak M, Bloemenkamp KW, Kelly AJ, Mol BW, Irion O, Boulvain M (2012) Mechanical methods for induction of labour. Cochrane Database Syst Rev 3:CD001233
Pevzner L, Rayburn WF, Rummey P, Wing DA (2009) Factors predicting successful labor induction with dinoprostone and misoprostol vaginal inserts. Obstet Gynecol 114(2 Pt 1):261–267
Resnik R (2002) Intrauterine growth restriction. Obstet Gynecol 99(3):490–496
Rhinehart-Ventura J, Eppes C, Sangi-Haghpeykar H, Davidson C (2014) Evaluation of outcomes after implementation of an induction-of-labor protocol. Am J Obstet Gynecol 211(3):301.e1–301.e7
Crane JM (2006) Factors predicting labor induction success: a critical analysis. Clin Obstet Gynecol 49(3):573–584
Liu A, Lv J, Hu Y, Lang J, Ma L, Chen W (2014) Efficacy and safety of intravaginal misoprostol versus intracervical dinoprostone for labor induction at term: a systematic review and meta-analysis. J Obstet Gynaecol Res 40(4):897–906
Du C, Liu Y, Ding H, Zhang R, Tan J (2015) Double-balloon catheter vs. dinoprostone vaginal insert for induction of labor with an unfavorable cervix. Arch Gynecol Obstet 291(6):1221–1227
Bishop EH (1964) Pelvic scoring for elective induction. Obstet Gynecol 24:266–268
Chavakula PR, Benjamin SJ, Abraham A, Londhe V, Jeyaseelan V, Mathews JE (2015) Misoprostol versus Foley catheter insertion for induction of labor in pregnancies affected by foetal growth restriction. Int J Gynaecol Obstet 129(2):152–155
Hofmeyr GJ, Gulmezoglu AM, Alfirevic Z (1999) Misoprostol for induction of labour: a systematic review. Br J Obstet Gynaecol 106(8):798–803
Goldberg AB, Greenberg MB, Darney PD (2001) Misoprostol and pregnancy. N Engl J Med 344(1):38–47
Culver J, Strauss RA, Brody S, Dorman K, Timlin S, McMahon MJ (2004) Randomized trial comparing vaginal misoprostol versus Foley catheter with concurrent oxytocin for labor induction in nulliparous women. Am J Perinatol 21(3):139–146
Ben-Haroush A, Yogev Y, Glickman H, Kaplan B, Hod M, Bar J (2004) Mode of delivery in pregnancies with suspected foetal growth restriction following induction of labor with vaginal prostaglandin E2. Acta Obstet Gynecol Scand 83(1):52–57
Fox NS, Saltzman DH, Roman AS, Klauser CK, Moshier E, Rebarber A (2011) Intravaginal misoprostol versus Foley catheter for labour induction: a meta-analysis. BJOG 118(6):647–654
He Y, Hu J, Zhang X, Huang H, Chen Q (2014) Clinical analysis of double-balloon catheter for cervical ripening in 66 cases. Zhonghua Fu Chan Ke Za Zhi 49(10):741–745
Lydon-Rochelle M, Holt VL, Easterling TR, Martin DP (2001) Risk of uterine rupture during labor among women with a prior cesarean delivery. N Engl J Med 345(1):3–8
De Bonrostro Torralba C, Tejero Cabrejas EL, Marti Gamboa S, Lapresta Moros M, Campillos Maz JM, Castán Mateo S (2017) Double-balloon catheter for induction of labour in women with a previous cesarean section could it be the best choice? Arch Gynecol Obstet 295(5):1135–1143
Kehl S, Weiss C, Wamsler M et al (2016) Double-balloon catheter and sequential vaginal prostaglandin E2 versus vaginal prostaglandin E2 alone for induction of labor after previous cesarean section. Arch Gynecol Obstet 293(4):757–765
WHO (2011) WHO Recommendations for induction of labour. World Health Organization, Geneva. Available from: http://www.ncbi.nlm.nih.gov/books/NBK131963/. Accessed 31 July 2017
Duro-Gómez J, Garrido-Oyarzún MF, Rodríguez-Marín AB, de la Torre González AJ, Arjona-Berral JE, Castelo-Branco C (2017) What can we do to reduce the associated cost in induction of labour of intrauterine growth restriction foetuses at term? A cost-analysis study. Arch Gynecol Obstet. doi:10.1007/s00404-017-4458-x
Author information
Authors and Affiliations
Contributions
JDG: project development, data collection and analysis, and manuscript writing. MFGO: data analysis and manuscript editing. ABRM: data collection and management. AJTG: data collection and management. JEAB: data management and analysis, and manuscript editing. CC-B: data analysis, manuscript writing and editing
Corresponding author
Ethics declarations
Conflict of interest
We, the authors, declare that we have no conflict of interest.
Informed consent
This survey was conducted as an open prospective quasi-experimental cohort study and was approved by the institutional review board of the Reina Sofia Hospital (Córdoba, Spain. Reference 246-26/11/2015). All of the procedures were in accordance with the Helsinki Declaration of 1975.
Rights and permissions
About this article
Cite this article
Duro-Gómez, J., Garrido-Oyarzún, M.F., Rodríguez-Marín, A.B. et al. Efficacy and safety of misoprostol, dinoprostone and Cook’s balloon for labour induction in women with foetal growth restriction at term. Arch Gynecol Obstet 296, 777–781 (2017). https://doi.org/10.1007/s00404-017-4492-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-017-4492-8