Abstract
Background
Objectives of the current study were to find the most effective method of induction of labour in case of intrauterine foetal death (IUFD), with efficacy described as least induction-to-delivery time, and the agent with the best safety profile, i.e. least maternal complications.
Methods
This was a prospective observational descriptive study carried out between January and November 2015 in a tertiary care centre. Hundred consecutive cases of IUFD after 20 weeks of gestation requiring induction of labour and fulfilling inclusion criteria were selected. The method of induction decided by each consultant was noted, and results were analysed. As this was a purely observational study, all agents used for induction of labour (misoprostol, dinoprostone gel, intracervical Foley catheter) and all dose variations were included.
Results
The induction-to-delivery interval was shortest with dinoprostone (12.52 h) followed by Foley catheter (13.28 h) and misoprostol (15.82 h). However, the p value (0.301) was not statistically significant. Misoprostol was used more often in second trimester, while dinoprostone gel was most commonly used in third trimester. Failure occurred in 3 cases; all required lower segment caesarean section (LSCS). No significant complications were associated with any of the methods.
Conclusions
Dinoprostone gel, misoprostol and Foley catheter are safe for induction of labour in all cases of IUFD, even for those with previous LSCS with IUFD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Foetal death is defined by WHO as “death prior to complete expulsion or extraction from its mother of products of conception, irrespective of duration of pregnancy” [1]. IUFD is a tragic event for the parents and a cause of great stress for the caregiver. Spontaneous labour usually ensues after IUFD in majority of women within 2 weeks. However, induction of labour is performed in many cases due to psychological and social pressures, and these women need a method which can reduce the duration of labour. Currently, there are no standard protocols for induction of labour in IUFD. Prostaglandins (misoprostol, dinoprostone gel), oxytocin and intracervical Foley catheter have all been tried. Misoprostol in different doses and routes has been tried but not been standardized. There are very few studies which compare all methods of induction together. Within our institute, different methods are used in various combinations by different consultants.
Purpose of the Study
The primary endpoint of the study was to find the most effective method of induction of labour in IUFD, with efficacy described as least induction-to-delivery time; need for additional methods or augmentation with oxytocin was also studied. Secondary endpoints included analysis of safety of various methods, complications and need for LSCS in IUFD.
Methodology
This was a prospective observational descriptive study carried out in the Department of Obstetrics and Gynecology, Seth G.S. Medical College and K.E.M. Hospital, Mumbai, India, between January and November 2015. Hundred consecutive cases of IUFD after 20 weeks of gestation requiring induction of labour and fulfilling inclusion criteria were selected. The study was initiated after approval by the institutional ethics committee.
Inclusion Criteria
-
1.
All diagnosed cases of IUFD more than 20 weeks of gestation but not in labour
-
2.
Singleton pregnancy
Exclusion Criteria
-
1.
Refusal of consent for inclusion in study
All patients presenting to the outpatient or emergency department with IUFD were enrolled in the study after taking informed valid consent. Details of history, general physical and systemic examination, ultrasonography, basic laboratory investigations like haemoglobin level, and DIC profile were recorded. The method of induction decided by each consultant was noted, and results were analysed. As this was a purely observational study, all agents and all dose variations used were included.
Results
Of 100 cases included in the study, 85 were referred to our centre with IUFD; the commonest reason for referral was lack of availability of blood and blood products. Almost half of the cases had poor antenatal care, with < 3 visits. Majority of women were in the age group 21–30 years; 47% were primipara, 2% were grand multipara, and 51% had parity between 2 and 4. The commonest documented aetiology for IUFD was hypertensive disorders (25), IUGR (11) and diabetes mellitus (3); aetiology was unexplained in 26 cases, and major congenital malformations were seen in 9 cases. Thirty-two patients presented in second trimester between 20 and 28 weeks, and 68 patients presented after 28 weeks.
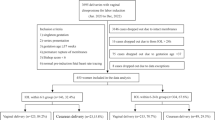
Induction of labour was done with dinoprostone gel in 64 cases (9 in second and 55 in third trimester); misoprostol in 28 cases (20 in second and 8 in third trimester); and intracervical Foley in 8 cases (3 in second and 5 in third trimester). Figure 1 shows the primary method of induction at various gestational ages.
Misoprostol was more commonly used in second trimester, while dinoprostone was used in third trimester. Of the 64 cases where dinoprostone was used as the primary method, 15/64 cases delivered with dinoprostone alone, an additional 6/64 cases delivered with second insertion of dinoprostone gel after 6 h, whereas majority of cases (43/64) needed a secondary method of induction, either oxytocin or Foley catheter. A small proportion (10/64) required 2 insertions of dinoprostone gel, followed by Foley catheter and oxytocin. There were no failures in this group. Figure 2 shows distribution of cases of dinoprostone.
Misoprostol was used more often in second trimester and early weeks of third trimester. All consultants used the vaginal route; however, there was no uniformity in dose schedule. Higher doses were used in second as compared to third trimester; 400 µg four hourly (maximum 5 doses) was used most frequently in second trimester, while 200 µg of single dose followed by 50 µg four hourly (maximum 5 doses) was used most frequently in third trimester, as shown in Fig. 3. Two of 28 cases required oxytocin as secondary method; 7/28 cases experienced minor side effects like fever, diarrhoea. Major complications like uterine rupture or post-partum haemorrhage were not encountered in any of the cases; however, there were 2 failures in this group.
Intracervical Foley catheter as primary method of induction was used in 8 cases, all in third trimester, and was the preferred method in patients with previous LSCS. In 5 cases, Foley was expelled spontaneously, while in 3 cases, it was removed after 6 h. Oxytocin was required in 7/8 cases for augmentation of labour. There was 1 failed induction but no major side effects or complications in this group.
Oxytocin was needed in 52% of cases as a secondary method or to augment labour, most often in the dinoprostone (43/64) and Foley groups (7/8), as shown in Fig. 4.
Management of cases of previous LSCS with IUFD is shown in Table 1: There were 10 cases of previous one LSCS and 1 case of previous 3 LSCS. In second trimester, most common method used was misoprostol (4/5 cases), while in third trimester, Foley and dinoprostone gel were used equally. There were 2 failures in this group.
Overall, 97 out of 100 patients delivered successfully. Failed induction of labour occurred in 3 cases all of whom required LSCS. Details of 2 of these cases are outlined in Table 1. One case of previous 1 LSCS underwent LSCS 17 h 15 min after induction with Foley catheter followed by oxytocin in view of non-progress of labour. The second case was previous three LSCS with IUFD at 34 weeks who was induced with misoprostol 400 µg followed by 200 µg 4 hourly for 5 doses (total 1400 µg). LSCS was done at 56 h in view of failed induction. The third case was a primigravida with IUFD at 30 weeks, induced with misoprostol 400 µg followed by 200 µg 4 hourly for 7 doses (total 1800 µg); LSCS was done in view of failed induction at 7 doses 4 h apart of misoprost amounts to 28 h.
The mean induction-to-delivery time was used to determine efficacy; the time for three primary methods of induction was calculated and compared using ANOVA test, as shown in Table 2. Irrespective of method used, the average time to delivery was 13.50 h. The delivery time in majority of the patients (95% confidence interval) was between 11.63 and 15.36 h. It was least for dinoprostone group [12.52 h (751 min)] followed by Foley group [13.28 h (786 min)] and highest with misoprostol group [15.82 h (949 min)]. Though dinoprostone gel had the least induction-to-delivery time, the individual variation in duration (range) was high with gel. However, the p value was 0.301 which was not statistically significant. Hence, we can conclude that the three methods were equally effective with respect to the induction-to-delivery time. Table 2 also shows the delivery times with various doses of misoprostol, the difference between which was statistically significant. We can conclude that 200 µg stat followed by 4 hourly 50 µg dose appears to be the most effective dosage.
No significant side effects were associated with dinoprostone gel and Foley; 7/28 misoprostol cases had minor side effects like fever and diarrhoea. Ten patients had severe anaemia and received blood transfusion. Post-partum haemorrhage was seen in single case of dinoprostone group; she received two units of whole blood. Two patients had disseminated intravascular coagulation (DIC) due to underlying pathology (preeclampsia), which was corrected with fresh-frozen plasma and cryoprecipitate.
Discussion
Death of a viable foetus is a stressful situation for the family and the obstetrician. Despite advances in medical science, diagnostic and therapeutic modalities, pregnancy wastage still occurs at an unacceptably high rate. Although perinatal mortality has reduced over last few decades, foetal deaths still remain high [2]. Our facility is a tertiary referral centre, and many women are referred for further management after IUFD has already been diagnosed.
In our prospective study, we analysed different methods for induction of labour in IUFD, namely misoprostol, dinoprostone gel and Foley catheter, and variations in dosage used by different consultants. Ethacridine lactate which was previously available could have been an excellent option in the second trimester; however, there are no recent references in the literature of its use in IUFD. The only recent publication is a study from China which compared efficacy of mifepristone and ethacridine lactate with ethacridine lactate alone for pregnancy termination among 276 women between 16 and 27 weeks of gestation; however, unlike our study, these were not cases of IUFD. Mei [3] found that induction-to-abortion interval, blood loss, rate of retained placental tissue and uterine evacuation were significantly less in the misoprostol and ethacridine lactate group v. the ethacridine group.
Singh [4] identified risk factors and aimed to streamline preventive and management protocols for IUFD. However, no aetiological causes were identified in 33.44% of their 296 cases; this was similar to our study in which aetiology was unexplained in 26% of cases.
A prospective study of 40 women with IUFD after 28 weeks of gestation by Biswas [5] compared the efficacy, safety and tolerance of misoprostol versus dinoprostone gel in induction of labour. They concluded that both misoprostol and dinoprostone gel are safe; misoprostol is more effective in terms of reducing induction-to-delivery interval, with requirement of lesser dose. This was in contrast to our study, where induction-to-delivery time was shorter for dinoprostone group (12.52 h) as compared to misoprostol group (15.82 h), which may be explained by the fact that we included both second and third trimester cases of IUFD and there was a great variation in the doses of misoprostol used in our study.
Nascimento [6] analysed the use of vaginal misoprostol and/or induction/augmentation with intravenous oxytocin in 171 women with IUFD in second and third trimesters in a teaching hospital in Brazil. Patients were divided to group A (misoprostol alone), B (misoprostol and oxytocin) and C (oxytocin alone) in 9.3, 19.9 and 70.8% of the cases, respectively. The mean induction-to-delivery interval was 15.4 h. The majority (71%) of cases required a single administration of misoprostol, and the mean dosage was only 98.4 μg in group A. They concluded that misoprostol effectively contributed to delivery of IUFD by vaginal route and recommended its availability in the public health service.
Gawron [7] described the management of third trimester stillbirths in 74 women using chart reviews. The mean gestation age was 35.5 weeks; induction methods included misoprostol, oxytocin and amniotomy; transcervical Foley catheter; and mifepristone. Similar to our study, the median time to delivery was 11 h 20 min; 98% of women including those with previous LSCS had a successful vaginal delivery. They concluded that misoprostol might confer the shortest induction intervals; however, further prospective trials are needed to identify the optimal misoprostol regimen in third trimester stillbirths.
In a randomized controlled study by Rab et al. [8] in Egypt, 200 women with stillbirth, unfavourable cervix and scarred uterus underwent cervical ripening with either Foley catheter or Cook cervical ripening balloon. Time from balloon insertion to expulsion and from insertion to delivery was significantly shorter in Foley group. However, the difference between the two groups with respect to other parameters like time to active labour, balloon expulsion to delivery, incidence of CS, pain score, hospital stay and maternal satisfaction was not statistically significant. The authors concluded that both methods are comparable in cases with scarred uteri; however, Foley has a shorter induction delivery interval and is cheaper.
Conclusions
Management of IUFD has immense significance in today’s obstetric practice. To summarize, dinoprostone gel, misoprostol and Foley can be used for induction of labour in second and third trimester IUFD. Of these, misoprostol is probably the most cost-effective method as it is cheap and easily available, compared to dinoprostone which is more expensive and requires refrigeration. All three methods can be used safely in cases of previous LSCS. However, because of heterogeneity in methods used as well as dosage, it is difficult to suggest a standardized protocol for induction of labour in cases of IUFD or make recommendations based on our study, especially with regard to dosage of misoprostol. Also, second and third trimester cases were studied together, yet the two may be quite different clinical entities and the optimal dose and regimen may differ between different gestational periods. The subjective preference and comfort of individual consultants still play a major role in selecting the agent for induction of labour and will continue to do so till larger and long-term comprehensive, prospective comparative data are available.
References
MacDorman MF, Kirmeyer SE, Wilson EC. Fetal and perinatal mortality, United States, 2006. Natl Vital Stat Rep. 2012;60(8):1–22.
Clinical Practice Guideline: Investigation and management of late fetal intrauterine death and stillbirth. Institute of Obstetrician and Gynaecologists, Royal College of Physicians Ireland, and Directorate of Strategies and Clinical Programmes, Health Service Executive. October 2011, revised 2013. Version 1.0, guideline no. 4.
Mei Q, Li X, Liu H, et al. Effectiveness of mifepristone in combination with ethacridine lactate for second trimester pregnancy termination. Eur J Obstet Gynecol Reprod Biol. 2014;178:12–5.
Singh N, Pandey K, Gupta N, et al. A retrospective study of 296 cases of intrauterine fetal deaths at a tertiary care centre. Int J Reprod Contracept Obstet Gynecol. 2013;2:141–6.
Biswas T. Misoprostol (PGE1) versus dinoprostone gel (PGE2) in induction of labour in late intra uterine fetal death with unfavourable cervix: a prospective comparative study. Int J Reprod Contracept Obstet Gynecol. 2015;4:35–7.
Nascimento MI, Cunha AA, Oliveira SR, et al. Misoprostol use under routine conditions for termination of pregnancies with intrauterine fetal death. Rev Assoc Med Bras. 2013;59(4):354–9.
Gawron LM, Kiley JW. Labor induction outcomes in third-trimester stillbirths. Int J Gynaecol Obstet. 2013;123(3):203–6. https://doi.org/10.1016/j.ijgo.2013.06.023 (Epub 2013 Sep 4).
Rab MT, Mohammed AB, Zahran KA, et al. Transcervical Foley’s catheter versus Cook balloon for cervical ripening in stillbirth with a scarred uterus: a randomized controlled trial. J Matern Fetal Neonatal Med. 2015;28(10):1181–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr Kinnari Amin, Dr Anahita Chauhan and Dr Anchal Goel declare that they have no conflict of interest.
Ethical Approval
All procedures followed were in accordance with the ethical standards of the institutional ethics committee and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Kinnari V. Amin is an Ex-Registrar, Department of Obstetrics and Gynecology, Seth G. S. Medical College and K.E.M. Hospital, Mumbai, Maharashtra, India. Anahita R. Chauhan is a Former Professor and Head of Unit, Department of Obstetrics and Gynecology, Seth G.S. Medical College and K.E.M. Hospital, Mumbai, Maharashtra, India. Anchal Goel is an Ex-Registrar, Department of Obstetrics and Gynecology, Seth G.S. Medical College and K.E.M. Hospital, Mumbai, Maharashtra, India.
Rights and permissions
About this article
Cite this article
Amin, K.V., Chauhan, A.R. & Goel, A. Current Practices of Cervical Ripening and Induction of Labour in Intrauterine Foetal Demise: An Observational Study. J Obstet Gynecol India 69, 37–42 (2019). https://doi.org/10.1007/s13224-017-1085-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-017-1085-1