Abstract
Objective
To evaluate the feasibility and effectiveness of intraoperative nerve staining by modified leucomethylene blue (MLB).
Methods
Animal experiment was performed to assure whether the tissues dyed blue by MLB were nerves with microscopic examination. Ten patients with cervical cancer were performed by nerve-sparing radical hysterectomy (NSRH) and nerve staining intraoperatively by MLB. The status of staining was recorded. The post-void residual urine volume after removing was measured by ultrasound. The time to post-void residual urine volume of less than 100 ml and the first defecation were recorded.
Results
In animal experiment, the tissues dyed blue obviously showed abundant nerve fibers by microscopic examination. The minor nerves were dyed blue clearly in NSRH. The time to post-void residual urine volume of less than 100 ml after removal of the urethral catheter was 10.3 (7–13) days by records. The time to the first defecation was 67.7 (60–82) h.
Conclusion
Intraoperative nerve staining by MLB provided a new method for nerve location in NSRH. It was safe, effective and convenient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Previous papers suggested that the careful identification and preservation of the hypogastric nerves (HN) and pelvic splanchnic nerves (PSN) is significant to minimize bladder function injury during the past years [1, 2]. The total meometrial resection (TMMR), as a kind of NSRH with excellent oncological outcomes, was performed by M. Hockel in open technique [3] and recently translated in robotic and laparoscopic surgery by other authors [4, 5]. However, the origin and distribution of the pelvic nerve plexus have not been fully described and it was a difficult technique to discriminate the nerve and other tissues in operation. If anatomical details of the pelvic nerve plexus and the vesical branches could be clarificated, various types of nerve-sparing laparoscopic radical hysterectomies would be achieved more successfully. Moreover, no standardized technique for NSRH has been confirmed and controversies still exist about its oncological safety when NSRH performed [6, 7].
We consider whether nerve staining intraoperatively provides a precise nerve location in NSRH. Selective nerve staining by leucomethylene blue (LB) as an intraoperative aid has been shown to achieve complete vagotomy [8–10]. In this pilot study, we performed nerve staining intraoperatively by modified leucomethylene blue (MLB) in NSRH and observed the effectiveness of nerve staining.
Materials and methods
Animal experiment
MLB consists of 800 mg Na2S2O3·5H2O, 10 ml 0.1% leucomethylene blue, and four drops of dilute hydrochloric acid (proportion 1.17, hydrochloric acid/water 1/3). The final solution was colorless and pH was 4.0.
Intraperitoneal 1% pentobarbital sodium (30 mg/kg) was used for anesthesia. The SD rats breathed spontaneously throughout the whole experiment. The abdomen of rat was opened through a midline incision after anesthetizing. Esophagus and stomach were exposed and the serous was removed. The esophagus and stomach was covered by MLB quickly, followed by physiological saline douched the stained area. The process was repeated three times and the vagus nerve was dyed blue (Fig. 1). After that, the tissue stained obviously was selected for microscopic examination.
Nerve staining in NSRH
Ten patients with cervical cancer, stage IB1 (tumor size ≤2 cm), requiring radical hysterectomy, were performed by NSRH and nerve staining intraoperatively during the period from September 2015 to December 2015 in the Obstetrics and Gynecology Hospital of Fudan University, Shanghai, P. R. China. The study design and protocol were approved by the Institutional Review Board, and all patients were given written informed consent after the procedure was explained fully. Clinical data obtained, including age, stage, histology, operating time, blood loss, intra- and postoperative complications, length of stay, time to recovery of bladder and rectal function.
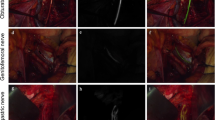
Nerve-sparing surgery was performed as follows: pelvic lymphadenectomy was performed in all patients. HN, located in the pararectal space, was near the rectum and it ran parallel to the utero-sacral ligament (USL) [11]. Followed by the lateral peritoneum beside the USL and the posterior leaf of the broad ligament dissected longitudinally along the USL, the Okabayashi pararectal spaces were covered by MLB quickly, followed by saline flushed stained area. The process was repeated three times. Then the hypogastric nerve plexus was exposed under the peritoneum. The HN and branches were dissected and preserved laterally to the pelvic wall (Fig. 2).
The prerectal space was developed by blunt dissection when isolation of the USL and rectal pillars and after dissection of the peritoneum of the Douglas pouch. The prerectal and the pararectal spaces were distinguished and the Okabayashi space was identified. MLB was used again and the ablation of impalpable nerves dominating rectum was avoided (Fig. 3).
The HN was traced towards the cardinal ligament and the posterior-lateral wall of the uterus, forming the inferior hypogastric plexus combined with the PSN. Then the MLB was used to locate the nerve bundles running parallel to the posterior leaf of the vesicocervical ligament from the cardinal ligament to the bladder (Fig. 4).
The paravaginal space was distinguished by dissecting the loose connective tissue among the side of the vagina and the posterior leaf of the vesicouterine ligament. The MLB was used to locate the nerve fibers, including the bladder branches and other minor ones from the inferior hypogastric plexus (Fig. 5).
Assessment of bladder and rectal function
All patients were placed a Foley catheter for 7 days postoperatively. Bladder function was assessed from day 7 after surgery. Postoperative post-void residual urine volume of less than 100 ml was indication for success after removing the Foley catheter. The post-void residual urine volume after removing was measured by ultrasound. The bladder was catheterized again in case of the post-void residual urine volume exceeded 100 ml. And the urine volume was measured every 3 days until the post-void residual urine volume was less than 100 ml. The time to post-void residual urine volume of less than 100 ml and the first defecation were recorded.
Results
Animal experiment
The tissue selected showed abundant nerve fibers by microscopic examination (Fig. 6).
Nerve staining in NSRH
The nerve staining in NSRH was performed successfully? for all the patients in this study. The minor nerves were dyed blue clearly in the operation. The mean operating time was 187 (range 170–210) min. The mean blood loss was 266 (range 200–380) ml. The average length of stay was 12.9 (range 10–15) days. No intraoperative and postoperative complications were reported. No lymph node, parametrium metastasis and lymph vascular space invasion were revealed by pathologic evaluation.
The time to post-void residual urine volume of less than 100 ml after removal of the urethral catheter was 10.3 (7–13) days by records. The time to the first defecation was 67.7 (60–82) h (Table 1).
Discussion
The technique for systematic preservation of the pelvic autonomic nerve system, which contains the HN, the PSN, the pelvic plexus and the bladder branches of the pelvic plexus, was further improved and described. However, until now, the minor nerves, even some main ones were illegible intraoperatively.
It was reported that several methods were applied in the NSRH to localize the nerve. Intraoperative electrical stimulation (IES) while monitoring intravesical pressure during radical hysterectomy represents a technically simple and useful procedure for the prediction of postoperative bladder function. However, it has an element of invasiveness; the appropriate nerve was not actually in the location where the IES probe was applied or that the nerve was temporarily damaged during the course of the operation [11–13]. A cavitron ultrasonic surgical aspirator (CUSA, Excel) was applied to remove parametrial tissue to preserve the autonomic hypogastric nerve in NSRH [14]. Nevertheless, the procedure needs special equipment and is expensive for many patients in developing countries. In a word, the procedures above can only be performed by experienced surgeons.
In this pilot study, we introduced a new technique of intraoperative nerve staining with MLB for NSRH. It was proved to be safe, effective and convenient.
Oded reported that methylene blue staining as an aid to facial nerve identification in parotid gland surgery. However, the specificity of the pure methylene blue was not distinguished in nerve staining. Furthermore, it was performed by injection into the gland and it was a potential hazard for tissue damage [15]. LB consists of 0.4% methylene blue, 7.02% ascorbic acid, and 1.68% sodium bicarbonate solution. It is a colorless or very faintly blue solution. If exposed to the air, it rapidly changes to deep blue, oxidized by the atmosphere. It was initially applied to vagotomy for the patients with stomach ulcer [8–10, 16].
However, Peer et al. indicated that the coloring of the distal esophagus with LB is of no clinical value in achieving completeness of vagotomy because nerve tissue was confirmed in only 33% of nerve tissue removed [10]. Because ascorbic acid cannot completely oxidized methylene blue, LB is also susceptible to oxidation in the dyeing process, this oxidized methylene blue can only remain extracellular, resulting in non-specific staining, affects the staining results. However, the MLB is maintained in the reduced state in this procedure, which can enter nervous tissue. The strong oxidizing ability of nervous tissue oxidated the reduced MLB. Nerve showed blue, so the MLB had better specificity than LB in nerve staining. Other cells lack this oxidation, and therefore cannot be dyed blue. It suggested that nervous tissue either stores or has access to considerably more oxygen than other tissues did. Recently, it has been criticized that there is no standardized technique for NSRH, and controversies still exists about its oncological safety [5–7]. So the nerve staining provides a chance to make a balance between reasonable oncological outcomes and function-preserving. In the opposite, in performing a truncal vagotomy, the dye should be applied to make absolutely sure no vagal fibers, even small, were left lying on the esophagus.
On the other hand, it was absolute that the pelvic nerve plexus appears as a mesh, not one or two fibers. In the operation, the nerves spared were always visible by naked eye. And the minor nerves, producing a marked effect, were always neglected. Moreover, there were variant nerves sometimes, just like the vessels. Proper staining of the nerve solved the thorny problems. Our study suggested small nerve fibers oxidize the MLB more readily than muscle or connective tissue and it was proved selective. Large nerve fibers or trunks are not stainable. The reason for this may be that the thick sheath of the larger nerves impedes MLB to penetrate. However, in the process of NSRH, most nerves injuried or excised were hard to be detected by naked eye, and therefore difficult to be isolated and divided.
In our hospital, the patients always discharged from hospital when the postoperative pathology reports were received. So the average length of stay was more than the duration recorded in the literature [17, 18].
There were some limitations of our study. First, it was only a pilot study, increased number of procedures with longer-term follow-up should be performed. Second, the abdominal cavity was filled with carbon dioxide and lack of oxygen under laparoscopy so the oxidation of MLB was incomplete. Furthermore, the penetration of MLB is not powerful enough and the tissues covered the target nerve fibers should be isolated when staining. Last but not least, the specificity of MLB needs to be improved.
References
Liang Z, Chen Y, Xu H et al (2010) Laparoscopic nerve-sparing radical hysterectomy with fascia space dissection technique for cervical cancer: description of technique and outcomes. Gynecol Oncol 119:202–207
Sakuragi N (2015) Nerve-sparing radical hysterectomy: time for a new standard of care for cervical cancer? J Gynecol Oncol 26:81–82
Höckel M, Horn LC, Hentschel B et al (2003) Total mesometrial resection: high resolution nerve-sparing radical hysterectomy based on developmentally defined surgical anatomy. Int J Gynecol Cancer 13:791–803
Chiantera V, Vizzielli G, Lucidi A et al (2015) Laparoscopic radical hysterectomy in cervical cancer as total mesometrial resection (L-TMMR): a multicentric experience. Gynecol Oncol 139:47–51
Vizzielli G, Lucidi A, Gallotta V et al (2016) Robotic total mesometrial resection versus laparoscopic total mesometrial resection in early cervical cancer: a case-control study. J Minim Invasive Gynecol 23:804–809
Long Y, Yao D, Pan X et al (2014) Clinical efficacy and safety of nerve-sparing radical hysterectomy for cervical cancer: a systematic review and meta-analysis. PloS One 9:e94116
Roh JW, Lee DO, Suh DH et al (2015) Efficacy and oncologic safety of nerve-sparing radical hysterectomy for cervical cancer: a randomized controlled trial. J Gynecol Oncol 26:90–99
Frimer ML, Cohen MM, Harrison RC et al (1970) The selective nerve stain leucomethylene blue as an intraoperative aid to achieving complete vagotomy. Gut 11:881–882
Cooke WM, Welbourn RB, Talbot IC et al (1970) Leucomethylene-blue as aid to complete vagotomy. Lancet 1:864–865
Wille-Jørgensen P, Jensen HE (1981) Leucomethylene blue staining during vagotomy. Br J Surg 68:81–82
Nagai T, Niikura H, Kurosawa H et al (2012) Individualized radical hysterectomy procedure using intraoperative electrical stimulation for patients with cervical cancer. Int J Gynecol Cancer 22:1591–1596
Chen CL, Guo HX, Yu YH et al (2010) The measurement of vesical detrusor electromyographic activity during nerve-sparing radical hysterectomy. Reprod Sci 17:1144–1152
Katahira A, Niikura H, Kaiho Y et al (2005) Intraoperative electrical stimulation of the pelvic splanchnic nerves during nerve-sparing radicalhysterectomy. Gynecol Oncol 98:462–466
Raspagliesi F, Ditto A, Fontanelli R et al (2004) Nerve-sparing radical hysterectomy: a surgical technique for preserving the autonomic hypogastric nerve. Gynecol Oncol 93:307–314
Nahlieli O, Levy Y (2001) Intravital staining with methylene blue as an aid to facial nerve identification in parotid gland surgery. J Oral Maxillofac Surg 59:355–356
Kurihara K, Cohen M, Schultz RC (1984) Nerve staining with leucomethylene blue: an experimental study. Plast Reconstr Surg 73:960–964
Lanowska M, Brink-Spalink V, Mangler M, Grittner U et al (2014) Vaginal-assisted laparoscopic radical hysterectomy (VALRH) versus laparoscopic-assisted radical vaginal hysterectomy (LARVH) in the treatment of cervical cancer: surgical results and oncologic outcome. Arch Gynecol Obstet 289:1293–1300
Kimmig R, Iannaccone A, Aktas B et al (2016) Embryologically based radical hysterectomy as peritoneal mesometrial resection (PMMR) with pelvic and para-aortic lymphadenectomy for loco-regional tumor control in endometrial cancer: first evidence for efficacy. Arch Gynecol Obstet 294:153–160
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Dr Xuyin Zhang had no disclosure of potential conflicts of interest. Dr Luoqi Jia had no disclosure of potential conflicts of interest. Dr Xiang Tao had no disclosure of potential conflicts of interest. Dr Jingxin Ding had no disclosure of potential conflicts of interest. Dr Keqin Hua had no disclosure of potential conflicts of interest.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
X. Zhang and L. Jia contributed equally to this article.
Rights and permissions
About this article
Cite this article
Zhang, X., Jia, L., Tao, X. et al. Intraoperative nerve staining in nerve-sparing radical hysterectomy: a pilot study. Arch Gynecol Obstet 295, 737–741 (2017). https://doi.org/10.1007/s00404-016-4284-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4284-6