Abstract
Purpose
The aim of this study is to present long-term results including patients’ satisfaction, pelvic floor symptoms, regret and change in body image in a long-term follow-up after colpocleisis.
Methods
All women who underwent colpocleisis between September 2001 and February 2014 were identified from the hospital operating lists. These women were contacted for a telephone survey up to 13 years after surgery and asked to complete a structured questionnaire to assess patients’ satisfaction, Quality of Life (QoL) and pelvic floor symptoms.
Results
A total of 44 women underwent colpocleisis during the period from September 2001 to February 2014. Mean age was 78 years (range 65–91) years. Mean follow-up time was 41 months (range 10–120). Twenty women could be reached for the survey and were included in the analysis. 15 (75 %) reported a positive impact on QoL, 2 (10 %) a negative because of urinary problems, 2 (10 %) could not report any change in the QoL and 1 (5 %) could not answer this question. There was no recurrence of prolapse. The majority of patients (90 %) would undergo the same surgery again and no patient regretted the loss of her vaginal sexual function.
Conclusions
Colpocleisis seems to be an effective treatment for pelvic organ prolapse. In the long term, impact on quality of life is positive, whilst urinary tract symptoms seem to be the most bothersome factor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical procedures for pelvic organ prolapse (POP) can be categorized by reconstructive and obliterative techniques [1]. Colpocleisis is the most common term used internationally to describe various obliterative procedures which can include partial or total vaginal extirpation or removal of the vaginal epithelium, approximation of the perineal and pelvic floor muscles, aggressive perineorrhaphy and suture of the labia minora and can be combined with concomitant hysterectomy and incontinence surgical procedures [2]. Colpocleisis is considered to be a highly effective technique for correcting POP in women who do not wish to preserve the option of vaginal intercourse. As a matter of fact, due to the irreversibility of the procedure, but also due to its low morbidity, it is reserved for the frail and elderly who are sexual inactive [3]. Data suggest that in some centres up to 30 % of women of age >70 with POP are eligible to and receive colpocleisis as primary treatment [4]. Post-interventional satisfaction after careful patient selection and counselling is high, achieving cure rates of up to 100 % [5].
However, the literature about long-term results after colpocleisis is still sparse, since most published studies report a follow-up of up to 2–3 years. The aim of this study is to present long-term results including patients’ satisfaction, pelvic floor symptoms, regret and change in body image after colpocleisis.
Materials and methods
All women who underwent colpocleisis were identified from the hospital operating lists of the Clinic for Gynecology and Gynecological Oncology in the University Hospital of Basel between September 2001 and February 2014. In our institution, the decision to offer colpocleisis is made after at least two consultations. For women to be considered for the intervention, they have to declare that they are sexual inactive and do not seek to sexual intercourse in the future. All women are thoroughly counselled and all treatment options are discussed prior to surgery, with written information provided. Routine fitness for surgery assessment is performed in conjunction with the anaesthesiology department according to our in-house protocols, including EKG, chest X-ray and blood tests.
Our approach for colpocleisis comprised of partial vaginal extirpation, de-epithelialisation and approximation of the levator ani and perineorrhaphy. We included all patients which according to the surgery report were left with less than 6 cm of total vaginal length and 1 cm introitus width which according to the surgeon would not allow sexual intercourse. All women received prophylactic antibiotics intraoperatively and thromboprophylaxis postoperatively. According to our protocols, all patients received a Foley catheter 24–48 h. After removing the catheter, residual urine was measured and all patients received the standard postoperative care and were released according to the judgement of the responsible doctor. The postoperative control took place 4–6 weeks after surgery.
The women were contacted by telephone up to 13 years after surgery, informed about the reason for the telephone contact and asked if they would be willing to participate. Once verbal consent was obtained, our pre-designed structured questionnaire was completed over the telephone. Patients were asked to answer specific questions concerning surgery satisfaction, quality of life and pelvic floor symptoms. Patients were also given the opportunity to discuss their symptoms as well as whether they were the same or had deteriorated or improved following colpocleisis. Regret and recommendation of the surgery were assessed by two additional questions.
Results
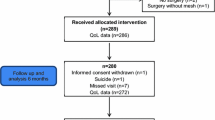
A total of 44 women underwent colpocleisis during the period from September 2001 to February 2014. All women met the criteria for inclusion in the study (total vaginal length <6 cm and narrowed introitus). Fourteen women had died by the time of the telephone call, six with dementia were unable to answer the questions, one patient refused to answer the questionnaire because of a non-specified reason, another one was in coma and two patients could not be traced. Thus, 20 women could be reached for the survey and were included in the analysis. Mean age was 82.7 (range 75–90) years and the mean follow-up time was 41 months (range 10–120).
All patients underwent colpocleisis according to our protocols as described in the materials and methods section. Six patients had a concomitant vaginal hysterectomy, three have had prior hysterectomy for reasons other than POP, seven had recurrence of prolapse after hysterectomy for prolapse and four were diagnosed with recurrence of prolapse after previous prolapse operation (Table 1).
Of the 20 patients who answered the questions, 15 (75 %) reported a positive impact on QoL and 2 (10 %) a negative impact. Two patients (10 %) could not report any change in the QoL and one (5 %) could not answer this question (Table 2). The two patients who reported a negative impact on their QoL also regretted having had surgery altogether because of persistence of urinary symptoms but none of them reported a change of body image or recurrence of prolapse. Two patients thought their body image had changed, one of them because she did not feel correctly informed and the other patient could not define the reason; however, these two patients reported a positive impact on their QoL and would still recommend the surgery.
Thirteen patients (65 %) described persistent urinary problems (Fig. 1). Two patients reported bowel problems, both of whom also had bowel symptoms before surgery. One patient with stool-outlet obstruction before surgery reported a complete resolution of the symptoms after colpocleisis. The majority of patients (90 %) would undergo the same surgery again and no patient regretted the loss of her vaginal sexual function.
Within the 44 interventions, five (11.4 %) major complications were recorded, namely four bladder injuries and one bowel perforation, which could be resolved during surgery. Mean estimated blood loss was 360 ml with an average operating time of 150 min. Two women, one of whom underwent concomitant vaginal hysterectomy, had a blood loss of 1200 ml and required blood transfusion. Fifteen patients received general anaesthesia and the remaining five interventions were performed under spinal anaesthesia.
Discussion
Surgical intervention for POP can have multiple approaches. Patients may undergo extensive pelvic reconstructive surgery, with native tissue or use of grafts or obliterative procedures such as colpocleisis. The goal of reconstructive surgery is to restore the normal anatomy and function, while obliterative surgery aims primarily to the correction of prolapse and relief of the symptoms by closing off a portion of the vaginal canal.
In our study, we present longitudinal data of up to 13 years after colpocleisis, with a mean follow-up time of 41 months, which is, to our knowledge, the longest follow-up reported. Within this time, none of our patients reported recurrence of pelvic organ prolapse. Fifteen out of 20 women (75 %) reported improvement in QoL. The worsening of QoL in two patients was due to persistence of urinary symptoms, specifically urge incontinence. In fact, the majority (65 %) of women after colpocleisis reported persistent urinary symptoms (Fig. 1). This is a common finding after surgery for POP [6]. Also our practice does not include performing incontinence surgery simultaneously with POP surgery. Instead, we prefer a two-stage management. Unfortunately, our data cannot be conclusive on the impact of colpocleisis on urinary incontinence, mainly because of two reasons: first, the assessment of urinary incontinence before surgery has been performed in a specialized urogynaecology department and differs from the telephone assessment performed in our follow-up. Second, some of our patients have been referred after surgery to other institutions and/or have received incontinence therapies which could not be tracked, partially because of the difficulty of history taking in many of the elderly patients included in our study. This was also the reason we decided not to use an extent pelvic floor questionnaire at follow-up but a simple and concise structured one.
The largest report regarding colpocleisis is from Zebede et al. including 310 women with a follow-up of 45 weeks [7]. They report a satisfaction rate of 92.9 % and an anatomical success rate of 98.1 %. Reisenauer et al. conducted a prospective longitudinal study and at a 14-month follow-up report a subjective cure rate of 94 %. They also report no recurrence of prolapse and no regret after surgery [8]. Vij et al. in a retrospective chart review report a median follow-up of 36 months after colpocleisis (range 24–60 months) [9]. They report on 23 cases, one of which (4 %) regretted having had the colpocleisis because of recurrence of prolapse. Interestingly, although Vij et al. report no major changes in bowel symptoms, which is similar to our observation, they report a 25 % improvement in urinary incontinence. In our study, we observed seven new cases of urinary incontinence postoperatively (six urgency, one stress urinary incontinence), which was the main contributing factor for reporting a worsening of QoL after colpocleisis. This finding is similar to the report of Koski et al., who found that urgency and frequency are the most common complaints (33.3 %) at a follow-up of 9.3 months after colpocleisis [10].
Colpocleisis seems not to be preferred by surgeons for the treatment of pelvic organ prolapse [11]. This is possibly due to the irreversible nature of the procedure, fear of regret and loss of sexual vaginal function but also due to the lack of long-term data following colpocleisis. However, the management of pelvic organ prolapse in the elderly represents a unique situation. Given that large cohort studies report that only 16.2 % of women between 75 and 85 years old are sexually active [12], discussing the primary goals of surgery in this patients’ group is essential. As a matter of fact, Crisp et al. report that the vast majority of women over 75 who receive colpocleisis have following goals: 55 % expect management or correction of prolapse, 27.5 % improvement in urinary or bladder symptoms and 11.25 % increase the ability to perform daily activities [13]. Regret in the study of Crisp et al. was mostly connected with urinary symptoms, whereas only one out of 87 women who reported ‘missing sex’ denied being sexually active preoperatively. These findings are also similar to our results.
There are some limitations to our study, the first being the small study population. However, most previously published studies report on similar numbers, possibly because colpocleisis is not a commonly performed operation. Also the retrospective nature of our analysis is prone to bias: the assessment of quality of life and pelvic floor symptoms was not performed using validated questionnaires and we could only reach 20 out of 44 patients, since many of them have deceased at the time of follow-up. However, we believe that our results reflect with accuracy the symptoms of the patients after colpocleisis, something that can be confirmed by the compliance of these results with previously published studies. The complications rate found in our cohort as well as the mean estimated blood loss and the operating time are higher than that reported from other authors; Reisenauer et al. report no intraoperative complications during colpocleisis [8].This is probably explained through the fact that we perform colpocleisis mostly in patients with recurrence or re-recurrence of prolapse (this was the case in the two women who needed blood transfusion) and almost every surgical procedure performed in our institution has also an educational purpose, which inevitably increases operating time and consequently blood loss.
Conclusion
Due to the increasingly ageing population, pelvic organ prolapse is expected to become a more common clinical challenge [14]. Colpocleisis seems to be an option in women who do not wish preservation of the vaginal sexual function, offering improvement in quality of life, while regret rates remain low. It seems that the most common complaint after colpocleisis is persistent urinary symptoms, which is also the major contributing factor affecting negatively the quality of life. Proper counselling of elderly women with pelvic organ prolapse, mostly regarding urinary symptoms and surgery’s goals, are very important in selecting patients who could benefit from colpocleisis.
References
Jelovsek JE, Maher C, Barber MD (2007) Pelvic organ prolapse. Lancet 369(9566):1027–1038
FitzGerald MP, Richter HE, Siddique S, Thompson P, Zyczynski H, Weber A (2006) Colpocleisis: a review. Int Urogynecol J 17:261–271
Abbasy S, Kenton K (2010) Obliterative procedures for pelvic organ prolapse. Clin Obstet Gynecol 53:86–98
Skoczylas LC, Turner LC, Wang L, Winger DG, Shepherd JP (2014) Changes in prolapse surgery trends relative to FDA notifications regarding vaginal mesh Int Urogynecol J 25:471–477
Misrai V, Gosseine PN, Costa P, Haab F, Delmas V (2009) Colpocleisis: indications, technique and results. Prog Urol 19(13):1031–1036
Wei JT, Nygaard I, Richter HE, Nager CW, Barber MD, Kenton K et al (2012) A midurethral sling to reduce incontinence after vaginal prolapse repair. N Engl J Med 366(25):2358–2367
Zebede S, Smith A, Plowright L, Hegde A, Aguilar V, Davila W (2013) Obliterative LeFort colpocleisis in a large group of elderly women. Obstet Gynecol 121:279–284
Reisenauer C, Oberlechner E, Schoenfisch B, Wallwiener D, Huebner M (2013) Modified LeFort colpocleisis: clinical outcome and patient satisfaction. Arch Gynecol Obstet 288:1349–1353
Vij M, Bombieri A, Dua A, Freeman R (2014) Long-term follow-up after colpocleisis: regret, bowel and bladder function. Int Urogynecol J 25(6):811–815. doi:10.1007/s00192-013-2296-3
Koski M, Chow D, Bedestani A, Togami J, Chesson R, Winters C (2012) Colpocleisis for advanced pelvic organ prolapse. Urology 80:542–546
Boyles S, Weber A, Meyer A, Meyn L (2003) Procedures for pelvic organ prolapse in the United States 1979–1999. Am J Obstet Gynecol 188:108–115
Lindau ST, Schumm LP, Laumann EO et al (2007) A study of sexuality and health among older adults in United States. N Engl J Med 357:762–774
Crisp C, Book N, Smith A, Cunkelman J, Mishan V, Treszezamsky A, Adams S, Apostolis C, Lowenstein L, Pauls R (2013) Body image, regret and satisfaction following colpocleisis. Am J Obstet Gynecol 209:473 (e1–7)
Mothes AR, Radosa MP, Altendorf-Hofmann A (2016) Runnebaum IB Risk index for pelvic organ prolapse based on established individual risk factor. Arch Obstet Gynecol 293:617–624
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding.
Conflict of interest
None.
Ethical approval
All procedures performed in the study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study
Rights and permissions
About this article
Cite this article
Katsara, A., Wight, E., Heinzelmann-Schwarz, V. et al. Long-term quality of life, satisfaction, pelvic floor symptoms and regret after colpocleisis. Arch Gynecol Obstet 294, 999–1003 (2016). https://doi.org/10.1007/s00404-016-4158-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4158-y