Abstract
Purpose
To investigate whether postoperative GnRH agonist (GnRH-a) treatment can prevent endometriosis recurrence.
Methods
This meta-analysis searched PubMed, Embase and Cochrane Library for relevant studies published online before June 2015. Seven randomized controlled trials including 328 patients with postoperative GnRH-a treatment and 394 patients in control group were included in the meta-analysis. In the meta-analysis, the recurrence rate of GnRH-a group compared with control group was evaluated with odds ratio (OR) and its 95 % confidence interval (CI). Heterogeneity, small study effect and publication bias were, respectively, assessed using Higgins I 2, sensitivity analysis and funnel plot.
Results
Postoperative GnRH-a treatment for endometriosis (pooled OR = 0.71; 95 % CI 0.52–0.96) was superior to expectant or placebo treatment in prevention of the recurrence. The recurrence rate decreased significantly in patients who received 6 months GnRH-a treatment (pooled OR = 0.59, 95 % CI 0.38–0.90), whereas no significant difference of recurrence rate existed between patients with 3 months post-surgical GnRH-a therapy and the control group (pooled OR = 0.87, 95 % CI 0.56–1.34). No significant heterogeneity and small study effect were found in the meta-analysis. However, publication bias did existed in the present meta-analysis.
Conclusions
Longer-term (6 months) postoperative administration of GnRH-a can decrease the recurrence risk of endometriosis, whereas 3 months duration of GnRH-a therapy makes no significant difference in preventing the recurrence of endometriosis. Therefore, instead of a 3 month therapy, the duration of the postoperative administration should be longer enough (6 months) to prevent the recurrence of endometriosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endometriosis is defined as the presence of functional endometrial epithelium and stroma outside the uterus. It affects 2–10 % of women of reproductive age and can result in dysmenorrhea and infertility [1]. Though endometriosis is a benign disease, it can behave malignantly by penetrating and developing elsewhere like cancer metastasis. Due to the lack of curable medicine treatment, laparoscopic surgery is recommended for the management of endometriosis, especially for those with endometriosis-associated pain or infertility [2]. However, the recurrence rate is reported to range from 18.9 to 40 % at 5 years after surgery and is directly correlated with the duration of follow-up [3–5]. Hospital readmission for additional surgical treatment was about 27 % in endometriosis patients within 4 years after surgery [6], and some patients require three or more re-operations [7]. To prevent the recurrence of endometriosis, hormonal treatment following surgery is often used to increase the efficacy of treatment by down-regulating the estrogen level.
Danazol, medroxyprogesterone acetate, combined hormonal contraceptives, as well as GnRH agonist (GnRH-a) have been usually used after conservative surgery. It is believed that postoperative medical treatment can eradicate microscopic lesions which are not identified and removed surgically. Nevertheless, the effect of the postoperative medical treatment is not well studied yet. GnRH-a is frequently used in endometriosis patients following conservative surgery (28 days interval for 3–6 months) to prevent recurrence. ESHRE guideline recommended that postoperative treatment with GnRH-a for 6 months reduces endometriosis-associated pain and delays recurrence at 12 and 24 months [8]. Postoperative GnRH-a treatment for 6 months was reported to reduce the recurrence rate and endometriosis-associated pain when compared with placebo or expectant management [9–11]. On the contrary, several studies reported that a 3- to 6-month course of GnRH-a treatment following surgery had no impact on the recurrence rate or pelvic pain in women with endometriosis [12–15]. Thus, the real value of post-surgical GnRH-a treatment in preventing recurrence of endometriosis is unproven.
The aim of the present meta-analysis was to evaluate the efficacy of postoperative GnRH-a treatment. Our primary objective was to determine whether postoperative GnRH-a treatment can reduce the recurrence rate of endometriosis. Our secondary objective was to evaluate the relationship between the duration of GnRH-a treatment and the recurrence rate of endometriosis.
Materials and methods
Search strategy and selection criteria
For this meta-analysis, we carefully and systematically searched PubMed, Embase and Cochrane Library for relevant studies published online before June 2015. The search terms “endometriosis”, “GnRH agonist or gonadotrophin-releasing hormone agonist or GnRH-a” and “postoperative or laparoscopy or conservative surgery”were used as keywords, respectively (search strategy for PubMed was shown in Supplementary Fig. 1). The searches were independently conducted in duplicate by two authors (QM Zheng and HL Mao). Studies were included if they met all of the following criteria: (1) endometriosis was diagnosed by surgery or pathology, (2) the study group only consisted patients who used GnRH-a as postoperative medical treatment, (3) the selection of control group was clearly described (no patients in the control group received hormonal therapy after the surgery), (4) be human studies, (5) published in English. Patients with previous hormone therapy were exclusion criteria. Case reports, review articles or studies published as abstracts only were also excluded. The previous two authors independently scanned article titles and abstracts and evaluated the eligibility of all studies according to the inclusion and exclusion criteria. Any disagreement in the process was resolved by discussion. Reference lists of selected articles and reviews were also checked for relevant studies. In case of duplicate publications, only those published most recently were included.
Data extraction
Data extraction was also independently performed by the two authors using a standardized data-collection form. The data were extracted from eligible studies: author’ name, country, year of publication, study design, numbers of patients in study and control groups, diagnosis of the recurrence of endometriosis, numbers of recurrent patients in study and control groups, duration of the postoperative GnRH-a treatment. The quality of each study was independently assessed by the two authors using the Jadad scale for randomized controlled trials [17].
Statistical analysis
The meta-analysis was performed with STATA software (version 12.0; Stata Corporation, College Station, TX, USA). All the results for binary outcomes were shown as OR with its 95 % CI (confidence interval). The impact of heterogeneity was assessed using Higgins I 2 [17]. I 2 values of 25, 50, and 75 % correspond to low, moderate and high heterogeneity. When P > 0.1 or I 2 ≤ 50 %, the fixed effect model using the Mantel–Haenszel method was used because it indicated acceptable heterogeneity. On the contrary, the random effects model was used when P < 0.1 or I 2 > 50 %. Sensitivity analysis was performed by recalculating the pooled OR after deleting studies one at a time to establish the robustness of our results. Funnel plot was produced using logOR of each study on the X axis and the standard error of logOR of each study on the Y axis to identify the presence of publication bias. Furthermore, Harbord’s test was used to test the symmetry of the funnel plot. P > 0.1 suggested that the funnel plot was symmetry and no significant publication bias existed.
Results
Selection of studies
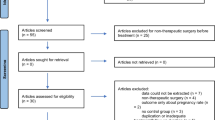
As shown in Fig. 1, 914 articles were selected from the three databases while 3 articles were identified from references. After deleting the duplicates and screening titles and abstracts, 42 articles were left assessed for eligibility, of which only 7 studies met the inclusion criteria after carefully evaluation [10, 13–15, 20, 22, 24]. Therefore, 7 randomized controlled trials including 382 patients with postoperative GnRH-a treatment and 394 patients in control group were included in the meta-analysis (Table 1). The studies were, respectively, conducted in Italy (n = 4), Iran (n = 1), Germany (n = 1) and Spain (n = 1). The Jadad score ranged from 2 to 5 for randomized controlled trials (Supplementary Table). Of the 7 studies, 2 studies considered dysmenorrhea relapse as recurrence, 1 studies considered transvaginal ultrasonographic endometrioma relapse as recurrence, while the other 4 studies considered either dysmenorrhea or endometrioma relapse as recurrence. As for the duration of GnRH-a treatment, 3 studies lasted 6 months, 4 studies lasted 3 months.
Main outcomes
Fixed effect model using the Mantel–Haenszel method was used because no obvious heterogeneity was found (P = 0.960, I 2 = 0.0 %, Fig. 2). As shown in Fig. 2, the result (pooled OR = 0.71; 95 % CI 0.52–0.96) revealed that postoperative GnRH-a treatment significantly decreased the endometriosis recurrence rate. Then, we analyzed the rate of endometriosis recurrence in patients with different durations of GnRH-a treatment by subgroup analysis. The results of heterogeneity tests were P = 0. 970, I 2 = 0.0 % for articles reporting the duration of 3 months, while P = 0. 887, I 2 = 0.0 % for articles reporting the duration of 6 months (Fig. 3). Therefore, the fixed effect model using the Mantel–Haenszel method was used to calculate the pooled OR. As shown in Fig. 3, no significant difference of endometriosis recurrence rate existed between patients with 3 months postoperative GnRH-a treatment and the control group (pooled OR = 0.87, 95 % CI 0.56–1.34), whereas the rate of recurrence decreased in patients who received 6 months postoperative GnRH-a treatment (pooled OR = 0.59, 95 % CI 0.38–0.90).
Publication bias and sensitivity analysis
As depicted in Fig. 4, though the funnel plot was visually symmetry, the Harbord’s test indicated that the funnel plot was asymmetry for Harbord’s test indicated significant difference (P = 0.026, Supplementary Fig. 2). So, publication bias existed in the present meta-analysis. Sensitivity analysis was performed to evaluate whether any small study effect influenced the pooled effect size. No significant changes were observed in the leave-one-out sensitivity analysis (Supplementary Fig. 3). Thus, the outcome of the current meta-analysis can be considered steady.
Discussion
In the present meta-analysis, we observed no statistical difference in recurrence rate between patients with and without postoperative GnRH-a treatment. However, when taken the duration of GnRH-a treatment into account, the recurrence rate significantly decreased in patients who received 6 months postoperative GnRH-a injection, while no significant decrease of recurrence rate was seen in patients with 3 months postoperative GnRH-a treatment.
Owing to the high relapse rate of endometriosis, a GnRH-a is frequently prescribed as a postoperative adjuvant therapy to reduce the symptoms and disease recurrence. Post-surgical administration of GnRH-a, an estrogen-lowing therapy, can eradicate microscopic lesions that could not be removed surgically and prevent iatrogenic dissemination of endometriotic cells [13]. However, data from randomized or cohort studies on the efficacy of GnRH-a are more controversial. Our meta-analysis pooled the OR (pooled OR = 0.71; 95 % CI 0.52–0.96) of the recurrence rate in patients with post-surgical GnRH-a therapy compared to the control patients, which revealed significant reduce in the symptoms and disease recurrence. The result was in accordance with previous reports that patients treated with GnRH-a had fewer symptoms recurrence and significantly smaller peritoneal implants at a second look laparoscopy [21–23]. Nevertheless, results from other reports documented that post-surgical administration of GnRH-a did not increase the pain relief or decrease the recurrence rate of disease [12, 15, 24, 25]. Though some results revealed no advantage of GnRH-a in preventing the recurrence of endometriosis, there are some benefits of the postoperative GnRH-a treatment. Administration of a GnRH agonist delayed the median time to recurrence by 2–5 months when compared with the expectant management group [9]. Postoperative treatment with GnRH-a was effective in the treatment of dyspareunia and improved the quality of sex life [26].
Jee et al. reported that longer-term treatment of GnRH-a could be beneficial to reducing the ovarian endometriomas or pain recurrence [9]. However, Hornstein et al. compared 3 months versus 6 months of nafarelin therapy and reported no significant difference in pain or clinical symptoms recurrence [27]. Thus, we analyzed whether longer duration of GnRH-a administration could decrease the symptoms or disease recurrence. Our results revealed that the recurrence rate decreased in patients who received 6 months GnRH-a treatment (pooled OR = 0.59, 95 % CI 0.38–0.90), whereas no significant decrease of recurrence rate existed in patients with 3 months post-surgical GnRH-a therapy (pooled OR = 0.87, 95 % CI 0.56–1.34). The difference can be explained by that short duration of GnRH-a therapy was not efficacy enough to eradicate microscopic lesions or prevent iatrogenic dissemination of endometriotic cells. Longer-term (6 months) administration of GnRH-a can decrease the recurrence rate by about 40 %. To test the reliability of the result, we calculated the sample size according to our result. The randomized clinical study should include 404 patients, 202 patients receiving GnRH-a treatment for 6 months and 202 patients receiving placebo for 6 months. In the present meta-analysis, 270 patients receiving GnRH-a treatment for 6 months and 263 receiving placebo were included. Thus, 6 months administration of GnRH-a indeed can decrease the recurrence rate of endometriosis. However, a limit of 6 months duration of GnRH-a is generally recommended because of its side effects and cost [28]. Even within a duration of 6 months, a 4–7 % reversible bone mineral loss can be expected [29]. To prevent the side effects, the addition of add-back therapy would improve the hypoestrogenic state while maintaining the efficacy of treatment [30]. Apart from the side effects, the high cost of GnRH-a therapy limits the course of the GnRH-a therapy. Usually, 3–6 months duration of GnRH-a treatment is recommended clinically. Taken that 3 months duration of GnRH-a therapy can not decrease the recurrence rate of endometriosis, we recommend 6 months postoperative GnRH-a treatment to prevent the recurrence.
Although 6-month, other than 3-month, duration of GnRH-a therapy is proved to decrease the recurrence rate of endometriosis, it should be carefully comprehended for the following reasons. Firstly, the stages of endometriosis can influence the results for recurrence rate is high in advanced stages [31]. But the stages of endometriosis for patients in each group were not reported in most included studies. Secondly, only one randomized trials included was double-blinded for it is difficult to keep the study double-blinded due to the side effects of GnRH-a. Thirdly, only studies published in English were included in the meta-analysis, which might miss studies published in other languages. Besides that, publication bias existed in the present meta-analysis. As a consequence, the meta-analysis should be updated if more large scale randomized controlled studies were published.
In conclusion, though this meta-analysis revealed no significant decrease in symptoms and disease recurrence in patients who received postoperative GnRH-a therapy, results differed in different durations of GnRH-a therapy. Longer-term (6 months) postoperative administration of GnRH-a can decrease the recurrence risk of endometriosis, whereas 3 months duration of GnRH-a therapy makes no significant difference in preventing the recurrence of endometriosis. The result suggests that it is reasonable to prevent recurrence of endometriosis with GnRH-a for patients who received conservative surgery. However, the duration of the postoperative administration should be long enough to prevent the recurrence of endometriosis. The meta-analysis should be updated if more large scale randomized controlled studies were published, especially those comparing the efficacy of different duration of GnRH-a treatment.
References
Eskenazi B, Warner ML (1997) Epidemiology of endometriosis. Obstet Gynecol Clin North Am 24(2):235–258
Dunselman GAJ, Vermeulen N, Becker C, Calhaz-Jorge C, D’Hooghe T, De Bie B, Heikinheimo O, Horne AW, Kiesel L, Nap A, Prentice A, Saridogan E, Soriano D, Nelen W (2014) ESHRE guideline: management of women with endometriosis. Hum Reprod 29(3):400–412. doi:10.1093/humrep/det457
Fedele L, Bianchi S, Zanconato G, Berlanda N, Raffaelli R, Fontana E (2006) Laparoscopic excision of recurrent endometriomas: long-term outcome and comparison with primary surgery. Fertil Steril 85(3):694–699. doi:10.1016/j.fertnstert.2005.08.028
Wheeler JM, Malinak LR (1983) Recurrent endometriosis: incidence, management, and prognosis. Am J Obstet Gynecol 146(3):247–253
Fedele L, Bianchi S, Di Nola G, Candiani M, Busacca M, Vignali M (1994) The recurrence of endometriosis. Ann N Y Acad Sci 734:358–364
Weir E, Mustard C, Cohen M, Kung R (2005) Endometriosis: what is the risk of hospital admission, readmission, and major surgical intervention? J Minim Invasive Gynecol 12(6):486–493. doi:10.1016/j.jmig.2005.09.001
Cheong Y, Tay P, Luk F, Gan HC, Li TC, Cooke I (2008) Laparoscopic surgery for endometriosis: How often do we need to re-operate? J Obstet Gynaecol 28(1):82–85. doi:10.1080/01443610701811761
Kennedy S (2005) ESHRE guideline for the diagnosis and treatment of endometriosis. Hum Reprod 20(10):2698–2704. doi:10.1093/humrep/dei135
Jee BC, Lee JY, Suh CS, Kim SH, Choi YM, Moon SY (2009) Impact of GnRH agonist treatment on recurrence of ovarian endometriomas after conservative laparoscopic surgery. Fertil Steril 91(1):40–45
Vercellini P, Crosignani PG, Fadini R, Radici E, Belloni C, Sismondi P (1999) A gonadotrophin-releasing hormone agonist compared with expectant management after conservative surgery for symptomatic endometriosis. Br J Obstet Gynaecol 106(7):672–677
Hornstein MD, Hemmings R, Yuzpe AA, Heinrichs WL (1997) Use of nafarelin versus placebo after reductive laparoscopic surgery for endometriosis. Fertil Steril 5:860–864
Parazzini F, Fedele L, Busacca M, Falsetti L, Pellegrini S, Venturini PL, Stella M (1994) Postsurgical medical treatment of advanced endometriosis: results of a randomized clinical trial. Am J Obstet Gynecol 171(5):1205–1207
Busacca M, Somigliana E, Bianchi S, De Marinis S, Calia C, Candiani M, Vignali M (2001) Post-operative GnRH analogue treatment after conservative surgery for symptomatic endometriosis stage III-IV: a randomized controlled trial. Hum Reprod 16(11):2399–2402
Loverro G, Carriero C, Rossi AC, Putignano G, Nicolardi V, Selvaggi L (2008) A randomized study comparing triptorelin or expectant management following conservative laparoscopic surgery for symptomatic stage III-IV endometriosis. Eur J Obstet Gynecol Reprod Biol 136(2):194–198
Alborzi S, Hamedi B, Omidvar A, Dehbashi S, Alborzi M (2011) A comparison of the effect of short-term aromatase inhibitor (letrozole) and GnRH agonist (triptorelin) versus case control on pregnancy rate and symptom and sign recurrence after laparoscopic treatment of endometriosis. Arch Gynecol Obstet 284(1):105–110
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17(1):1–12
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. Bmj 327(7414):557–560. doi:10.1136/bmj.327.7414.557
Sesti F, Capozzolo T, Pietropolli A, Marziali M, Bollea MR, Piccione E (2009) Recurrence rate of endometrioma after laparoscopic cystectomy: a comparative randomized trial between post-operative hormonal suppression treatment or dietary therapy vs. placebo. Eur J Obstet Gynecol Reprod Biol 147(1):72–77
Acién P, Quereda F, Campos A, Gomez-Torres MJ, Velasco I, Gutierrez M (2002) Use of intraperitoneal interferon alpha-2b therapy after conservative surgery for endometriosis and postoperative medical treatment with depot gonadotropin-releasing hormone analog: a randomized clinical trial. Fertil Steril 4:705–711
Liu X, Yuan L, Shen F, Zhu Z, Jiang H, Guo SW (2007) Patterns of and risk factors for recurrence in women with ovarian endometriomas. Obstet Gynecol 109(6):1411–1420. doi:10.1097/01.AOG.0000265215.87717.8b
Regidor PA, Regidor M, Kato K, Bier UW, Buhler K, Schindler AE (1997) Long-term follow-up on the treatment of endometriosis with the GnRH- agonist buserelinacetate. Long-term follow-up data (up to 98 months) of 42 patients with endometriosis who were treated with GnRH-agonist buserelinacetate (Suprecur(registered trademark)), were evaluated in respect of recurrence of pain symptoms and pregnancy outcome. Eur J Obstet Gynecol Reprod Biol 73(2):153–160
Sesti F, Pietropolli A, Capozzolo T, Broccoli P, Pierangeli S, Bollea MR, Piccione E (2007) Hormonal suppression treatment or dietary therapy versus placebo in the control of painful symptoms after conservative surgery for endometriosis stage III-IV. A randomized comparative trial. Fertil Steril 88(6):1541–1547
Mettler L, Ruprai R, Alkatout I (2014) Impact of medical and surgical treatment of endometriosis on the cure of endometriosis and pain. Biomed Res Int 2014:264653. doi:10.1155/2014/264653
Yap C, Furness S, Farquhar C (2004) Pre and post operative medical therapy for endometriosis surgery. Cochrane Database Syst Rev (3):CD003678. doi:10.1002/14651858.CD003678.pub2
Vercellini P, Frontino G, De Giorgi O, Pietropaolo G, Pasin R, Crosignani PG (2003) Endometriosis: preoperative and postoperative medical treatment. Obstet Gynecol Clin North Am 30(1):163–180
Ferrero S, Abbamonte LH, Parisi M, Ragni N, Remorgida V (2007) Dyspareunia and quality of sex life after laparoscopic excision of endometriosis and postoperative administration of triptorelin. Fertil Steril 87(1):227–229. doi:10.1016/j.fertnstert.2006.06.018
Hornstein MD, Yuzpe AA, Burry KA, Heinrichs LR, Buttram VL Jr, Orwoll ES (1995) Prospective randomized double-blind trial of 3 versus 6 months of nafarelin therapy for endometriosis associated pelvic pain. Fertil Steril 63(5):955–962
Olive DL (2004) Optimizing gonadotropin-releasing hormone agonist therapy in women with endometriosis. Treat Endocrinol 3(2):83–89
Sagsveen M, Farmer JE, Prentice A, Breeze A (2003) Gonadotrophin-releasing hormone analogues for endometriosis: bone mineral density. Cochrane Database Syst Rev (4):CD001297. doi:10.1002/14651858.cd001297
Howell R, Edmonds DK, Dowsett M, Crook D, Lees B, Stevenson JC (1995) Gonadotropin-releasing hormone analogue (goserelin) plus hormone replacement therapy for the treatment of endometriosis: a randomized controlled trial. Fertil Steril 64(3):474–481
Kikuchi I, Takeuchi H, Kitade M, Shimanuki H, Kumakiri J, Kinoshita K (2006) Recurrence rate of endometriomas following a laparoscopic cystectomy. Acta Obstet Gynecol Scand 85(9):1120–1124. doi:10.1080/00016340600627154
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This article does not contain any studies with human participants or animals performed by any of the authors.
Funding
This study was supported by grants from the National Natural Science Foundation of China (81370696) as well as the Science and Technology Development planning of Shandong (2013GGE27031).
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Q. Zheng and H. Mao contributed equally.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zheng, Q., Mao, H., Xu, Y. et al. Can postoperative GnRH agonist treatment prevent endometriosis recurrence? A meta-analysis. Arch Gynecol Obstet 294, 201–207 (2016). https://doi.org/10.1007/s00404-016-4085-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4085-y