Abstract
Purpose
To compare the role of an aromatase inhibitor (letrozole) with a GnRH agonist (triptorelin) versus case control on the pregnancy rate and recurrence of symptoms and signs in patients with endometriosis.
Methods
In a prospective randomized clinical trial, after treatment of 144 infertile women in their reproductive age by laparoscopy (whose endometriosis was confirmed by prior laparoscopy), they were divided into 3 groups: group 1 (47 cases) who received letrozole for 2 months, group 2 (40 patients) who were prescribed triptorelin for 2 months and group 3 who were 57 patients in the control group and did not receive any medication. We followed up each group at least for 12 months after their restoration of regular cycle.
Results
Pregnancy rate was 23.4% in group 1, 27.5% in group 2, and 28.1% in group 3. The results did not show significant differences among the 3 groups. Recurrence rate of endometriosis was 6.4% in group 1, 5% group 2 and 5.3% in group 3, which was not statistically significantly different as well.
Conclusion
Pregnancy rate and endometriosis recurrence rate are comparable among the 3 groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endometriosis, characterized by dysmenorrhea, infertility and dyspareunia, is a common disease among women in the reproductive age. The mechanisms which are mentioned as the causes of subfertility are ovulatory dysfunction, luteal insufficiency, luteinized unruptured follicle syndrome, recurrent abortion, altered immunity and intraperitoneal inflammation [1]. The recurrence of endometriosis after surgical therapy is still an unsolved problem for clinicians [2]. Although conservative surgery in laparoscopy is still known to be the best alternative for treatment of symptomatic endometriosis, it cannot prevent the recurrence of the disease. About 40% of patients have recurrences after 5 years following complete excision of endometriotic lesions [2].
The main goal of postoperative medical therapy is to accomplish complete removal of lesions which: cannot be surgically removed, to treat microscopic foci and to prevent iatrogenic metastatic endometriotic cells. However, considering harmful side effects and the cost of medical therapies we should have enough definitive evidence to conduct a combined surgical/medical study. At present, the postoperative effects of these medical therapies and results are not known clearly and conclusions from the few randomized controlled trials are contradictory [3–6].
In most of the studies postoperative medical treatment has been used for 6 months but as shown in some other studies, short courses of medical treatment after laparoscopic resection of endometriotic lesions is effective in reduction of implants’ volume and signs and symptoms of the patients [7–9].
In our study, a short period use of estrogen-lowering medical therapy after surgery has been suggested in order to increase the efficacy of treatment. We decided to evaluate the post-laparoscopic medical therapy in a randomized clinical trial. This was done by dividing the patients into three groups: the first group was given aromatase inhibitor (letrozole), the second group received GnRH analogue (triptorelin), and the third group did not take any medication. Postoperative medication was continued for 2 months after laparoscopic surgery, and then the patients were followed up for 12 months after their menstruation became regular. This study is the first research in the literature which compares the effect of postoperative letrozole with GnRH (triptorelin) versus case control on the pregnancy rate. The primary goal was to estimate whether this surgical/medical combined approach can produce a significant improvement in pregnancy rate and relief of pain symptoms.
Materials and methods
In a prospective randomized study, 144 infertile patients with laparoscopical and histological diagnosis of endometriosis were studied from June 2004 through January 2007. The patients were selected from those referred to private and university infertility clinics. Method of randomization was by computerized numbering. The Institutional Review Board of Shiraz University of Medical Sciences (Shiraz, Iran) approved this study. All the patients have signed the consent form and everyone was allowed to withdraw their cooperation at any time if they wished. All the patients were infertile at least for 12 months and some of them had symptoms such as dysmenorrhea, dyspareunia and pelvic pain.
For investigation of infertility, in addition to taking history and physical exam, two times semen analysis, transvaginal sonography (TVS), hysterosalpingography (HSG) and hormonal profile were performed. There were no statistical differences in the infertility evaluations of the groups (such as FSH levels, antral follicle counts or other parameters). Laparoscopy with histological confirmation of endometriosis was done afterwards. All the laparoscopies were performed by the first author. The patients were classified according to revised American Society for Reproduction Medicine (ASRM) [10].
Under general anesthesia, laparoscopy was performed, using a subumbilical incision and two or three lower part incisions. After evaluation of the abdomino-pelvic structures and peritoneal surface, adhesionolysis by sharp dissection was done to fully mobilize the ovaries and other pelvic structures. All the peritoneal lesions were excised, cystectomy was performed for all endometriomas and the tissues were sent for pathologic examination [11]. The patients entered into our study only if endometriosis was shown histologically. Those with severe male factor infertility requiring intra-cytoplasmic sperm injection (ICSI) or those who had preoperative medication were excluded from the study. However, due to exclusion criteria 144 cases were finally selected. Then they were divided into three groups by random computer-generated lists. Group 1: those who were prescribed an aromatase inhibitor, letrozole (Femara, Novartis Pharma AG, Basel, Switzerland), one tablet 2.5 mg/day in a period of 2 months, group 2: patients who were administered GnRH analogue, triptorelin (Diepherelin, Beaufour Ipsen Pharma Paris, France) Amp 3.75 mg (IM) in an interval of 4 weeks, for 2 months and group 3: the case–control group, those who did not receive any medication (Fig. 1).
They were followed up at 3-month intervals for 1 year, after restoration of their menstruation cycles. Only those patients who completed their follow-up periods were included. At each visit, the patients were asked about their symptoms and transvaginal sonography was performed for them (Fig. 1).
Before and after surgery each patient was asked to record the presence and severity of pelvic pain on a 10-cm linear analog scale. A score of 1–4 was considered mild pain and was not included in this study because of similarities between pain caused by endometriosis and non-endometriotic pain in this score. A score of 5–7 showed moderate pain and 8–10 severe pain. Recurrence of symptoms and signs was defined when dysmenorrhea, dyspareunia and pelvic pain were returned as per mentioned scoring [12]. In our study ultrasonography characteristics of simple cyst (vs. endometrioma) were: uniocular cysts with regular contour and smooth wall without internal echogenecity which disappears in follow-up [13]. Pregnancy was confirmed by ultrasonography and cardiac activity.
Results
After final exclusions, 144 patients entered our study with different stages and were divided into three groups. The patients’ demography data are shown in Table 1; there were no statistically significant differences regarding the mean age, type of infertility, duration of infertility, prevalence of different stages of endometriosis, score of the disease and preoperative prevalence of the symptoms such as pelvic pain, dysmenorrhea, and dyspareunia among three groups (Table 1).
Considering disease recurrence, there were no statistically differences among the three groups (Table 2) and also there were no correlation between the stages of endometriosis and pregnancy rate (Table 3).
There was a direct correlation between symptom and sign recurrence and stages of the disease (P = 0.008). Also, cyst formation occurred in the letrozole group as follows: functional cyst developed 24.3% in the letrozole group but only 2.5% in triptorelin group and none of the case–control group (P = <0.001). Regarding the functional cyst formation, there were statistically significant differences between patients who took letrozole and those who did not.
Comments
Surgery is usually the fundamental step in the management of advanced stages of endometriosis to reduce symptoms and treatment of subfertility, especially when there is mechanical distortion of the pelvis and reconstruction of normal pelvic anatomy is obligatory. Furthermore, many studies suggest that laparoscopic surgery of endometriosis is superior to laparotomy in many aspects due to low morbidity, decreased cost, and possibility of adhesion recurrence. In addition, diagnosis and treatment can be performed concomitantly, and the patients do not need to wait for a long time and undergo potential side effects of medical treatment [11]. Surgical management of infertile women with minimal and mild endometriosis is controversial. Some studies suggest that surgery has no advantages over expectant management [14], but others propose that laparoscopic surgery in even early stages of endometriosis would result in higher pregnancy rates compared with expectant management [15]. The recurrence of endometriosis after surgery is still an unsolved problem and the effectiveness of medical treatment is still controversial [3–7].
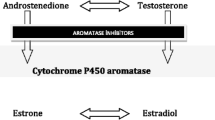
Medical treatment has been purposed to eradicate endometriosis lesions, in two ways. First through immunomodulated agents such as TNF (α) binding protein, recombinant interferon-α2β, iaxorbine, leukotriene receptor antagonists, anti-inflammatory agents such as pentoxifylline inhibition of matrix metalloproteinase (MMPS) and second through hormonal agents including estrogen–progesterone combinations, progesterone alone, antiprogesterone agent, danazol, gonadotropin releasing hormone agonist agents [16].
Preoperative medical treatment has been suggested to improve pregnancy rate and reduce symptom recurrence and volume of nodular cyst size. A study has suggested treating the patients by a 3-month course of GnRH agonist prior to operation to reduce vascularization and nodular cysts size [17]. Another study showed that hormonal therapy prior to surgery improved the score in endometriosis but no effects were shown on the pain relief after surgery. Although, the excision of deep rectovaginal endometriosis together with preoperative medical treatment can decrease the likelihood of recurrence of the disease and its symptoms, there is no convincing evidence that the medical treatment before surgery improves either pain control or fertility ratio compared to the plain only surgical treatment method [18].
Postoperative medical therapy has been more controversial. Some studies showed that GnRH agonist postoperative treatment resulted in diminishing pain scores and a delay of symptom recurrence for more than 12 months [3, 4]. It has been reported by Lemay and colleagues [8] that pain resolved in 70% and improvement in discomfort in 15% of 24 subjects after 2–4 months of treatment with buserelin. Also a significant reduction in implant volume occurred as early as 2 weeks after initiation of treatment in rat model by Zanagnolo et al. [9]. However, recent research could not show any effects of post-surgery hormonal treatment on reducing symptoms and signs compared with surgery alone or surgery placebo [7]. There are few studies designed to evaluate the relation between postoperative medical therapies with subfertility because it prevents conception and postpones pregnancy since the golden time for pregnancy is only 6–12 months after conservative surgery [3, 4].
Considering symptom and sign recurrence, our trial showed 6.4% in group 1, 5% in group 2, and 5.3% in group 3 (P = 0.48), which was not statistically significant (Fig. 1). Although in our study we may have underdiagnosed the recurrence of endometriosis (due to the patient complaints and sonographic documents of recurrence), but we did not operate the patients for second look surgery because of the patients displeasure and also regarding some studies which have not shown significant efficacy for second look surgery [19]. Regarding the effectiveness of estrogen-lowering postoperative medical treatment, some randomized controlled trials have been done. In a research on symptom recurrence, those who received 3-month therapy of GnRH analogue as interventional group were compared with the case control. They found that disease recurrence was 9% in both groups [5]. Another study had reported approximately the same results, i.e., 23% in patients who received danazol versus 31% in those who did not receive any medication [6]. Also, one research found 400 μg/day nasal naferlin for 3 months after surgery did not improve short-term pelvic pain [7]. One recent study comparing 3-month administration of triptorelin with placebo mentioned that the argument is in contradiction to the results of some studies [3, 4] which resulted in prescribing estrogen-lowering postoperative medication has useful effects, particularly significant delay of endometriosis symptoms recurrence. One study has illustrated that 31% of the patients treated with GnRH analogue for 6 months needed a substitute therapy for pain recurrence as compared with 57% of the patients allocated to postoperative placebo [14]. Another research using meta-analysis concluded that the time of symptoms recurrence was longer in GnRH analogue group (P < 0.001) [8].
One pilot study prescribed 6 months of letrozole for 10 patients suffering from severe pelvic pain, who had not responded to previous medical and presacral neurectomy. They concluded that post-operation medical treatment with letrozole should be considered in patients with endometriosis (P < 0.001) [20]. In another research by administrating anastrazole to 15 premenopausal patients with documented refractory endometriosis and chronic pelvic pain statistically pain relief was achieved in about 93% of them (P < 0.005) [21]. After publishing the results from these researches, one prospective study was designed to treat 12 patients with rectovaginal endometriosis, which were resistant to treatment. After 1 month of letrozole therapy, the patients’ symptoms decreased dramatically in 11 cases but pain recurred quickly at 3 months of follow-up after discounting their medication [22].
Our findings regarding pregnancy rate were 27.5% in the triptorelin group and 28.1% in the case control group (P = 0.72, Table 2). The results of our trial do not confirm significant additional benefits of 2-month administration of GnRH analogue post-laparoscopic surgery. Pregnancy rate in one study was 33% in the interventional group and 40% in the control whereas another research showed 55% in patients who received medicine while 50% in the case control. No statistically significant difference was revealed between interventional groups compared with case control [5, 6]. There are investigations which reported that administering postsurgical therapy postpones conception rate in the interventional group compared with case control [3, 4]. Three month administration of triptorelin did not reveal any benefits over placebo in 60 patients in pregnancy rate [7].
Pregnancy rate was 23.4% in the letrozole group and 28.1% in the case control (P = 0.72, Table 3). There was no statistically significant difference between treatment and case control. As mentioned earlier, this study is the first research undertaken to evaluate the effect of postoperative letrozole treatment in pregnancy rate of patients with endometriosis.
It should be noted that although suppressing ovulation for some months after surgery in women with endometriosis who complained about pelvic pain poses desirable effects [3, 4], approximately all of them believe that postoperative therapy should be avoided in those wanting children [3–7]. In fact, it has never been proven to have additional benefits but it causes delay in conception because patients are unable to conceive during medical treatment.
There were controversies regarding different stages of endometriosis and pregnancy rate. While some articles stated that the result of surgery in infertility relief is probably related to the severity of endometriosis, there are some researches showing negative correlation between the stage of endometriosis and the overall cumulative pregnancy rate after laparoscopy [23]. This negative relation seems statistically significant, especially when the revised scores are more than 70 [23]. The rate of pregnancy among different stages of endometriosis was comparable in our study. Pregnancy rate in letrozole group was 20.8% in stages I and II, 26.1% in stages III and IV. These results were 26.7% in stages I and II, 28% in stages III and IV in triptorelin group versus 30.8% in stage I and II, 25.8% in stage III and IV in the case control group, (P = 0.72, Table 3). One of the earlier prospective studies showed the same pregnancy rates in different stages of endometriosis by using pentoxifylline with case control (36.5 and 35.6%, respectively, P = 0.83) [16]. This fact has also been shown in another retrospective study that pregnancy rate among four stages of endometriosis becomes comparable [24].
Looking at the relationship of disease stages with recurrence of endometriosis, we found a direct association between them (P = 0.008). The rate of symptom recurrence increases with the stage of disease and duration of follow-ups. This fact has also been shown in another article which revealed that 5 years after completion of treatment, recurrence rate for minimal to mild disease was 37 and 74.6% for moderate to severe endometriosis [2]. The stage of disease at initial diagnosis of laparoscopy was significantly associated with a higher degree of pain recurrence at follow-ups [2, 25].
In summary, this study shows that pregnancy rates were comparable in patients taking either letrozole or triptorelin for 2 months versus the case control. Also the recurrence of symptoms and signs was comparable among the 3 groups. Therefore, considering the cost and side effects of short-term medications, taking post-operation drugs is not recommended.
Use of the statistics
We used chi-square test and ANOVA (Kruskal–Wallis H test) in our statistical analysis of the results to compare the 3 groups, and a P value less than 0.05 was considered significant.
References
Alborzi S, Zareie A, Alborzi S, Alborzi M (2006) Management of ovarian endometrioma. Clinical Obstet Gynecol 49:480–491
Fedele L, Bianchi S, DiNola G, Canadiani M, Bussaca M, Vignali M (1994) The recurrence of endometriosis. Ann N Y Acad Sci 734:358–364
Vercellini P, Frontino G, De Giorgi O, Pietropaolo G, Pasin R, Crosignani PG (2003) Endometriosis Preoperative and postoperative medical treatment. Obstet Gynecol Clin North Am 30:163–180
Vercellini P, Crosiginani PG, Fadini R, Belloni C, Sismondi P, Radici LE (1999) A gonadotropin-releasing hormone agonist compared with expectant management after conservative surgery for symptomatic endometriosis. B J Obstet Gynecol 106:672–677
Busacca M, Somigliana E, Bianchi S, De Marinis S, Calia C, Candiani M et al (2001) Post-operative GnRH analogue treatment after conservative surgery for symptomatic endometriosis stage III-IV: a randomized controlled trial. Hum Reprod 16:2399–2402
Bianchi S, Busacca M, Agnoli B, Candiani M, Calia C, Vignali M (1999) Effects of 3 month therapy with danazol after laparoscopic surgery for stage III/IV endometriosis: a randomized study. Hum Reprod 14:1335–1337
Hesla JS, Rock JA (2008) Endometriosis. In: Rock JA, Jones HW (eds) Telinde’s operative gynecology. Williams and Wilkins, Philadelphia, pp 438–473
Lemay A, Maheux R, Faure N, Jean C, Fazekas AT (1984) Reversible hypogonadism induced by a luteinizing hormone-releasing hormone (LH-RH) agonist (buserelin) as a new therapeutic approach for endometriosis. Fertil Steril 41:863–871
Zanagnolo VL, Beck R, Schlaff WD, Damewood MD, Bobbie D, Rock JA (1991) Time related effects of gonadotropin-releasing hormone analog treatment in experimentally induced endometriosis in the rat. Fertil Steril 55:411–415
American Society for Reproductive Medicine (1997) Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil Steril 5:817–821
Alborzi S, Ravanbakhsh R, Parasanezhad ME, Dehbashi S, Alborzi M, Alborzi S (2007) A comparison of follicular response of ovaries to ovulation induction after laparoscopic ovarian cystectomy or fenestration and coagulation versus normal ovaries in patients with endometrioma. Fertil Steril 88:507–509
Revill SI, Robinson JO, Rosen M, Hogg MIJ (1976) The reliability of a linear analogue scale for evaluating pain. Anesthesis 31:1191–1196
Adams Hillard PJ (2007) Benign disease of the female reproductive tract. In: Berek JS (ed) Berek and Novak’s Gynecology. Williams andWilkins, Philadelphia, pp 431–504
Rosen GF (1992) Treatment of endometriosis-associated infertility. Infert Reprod Med Clin North Am 3:721–730
Marcoux S, Maheux R, Berube S (1977) Laparoscopic surgery in infertile women with minimal or mild endometriosis. N Engl J Med 337:217–222
Alborzi S, Ghotbi S, Parsanezhad ME, Dehbashi S, Alborzi S, Alborzi M (2007) Pentoxifyline therapy after laparoscopic surgery for different stages of endometriosis: a prospective, double-blind, randomized, placebo-controlled study. J Minim Invasive Gynecol 14:54–58
Donnez J, Pirard C, Smets M, Jadoul P, Squifflet J (2003) Pre-and post- surgical management of endometriosis. Semin Reprod Med 2l:235–242
Audebert A, Descampes P, Marret H, Ory-Lavollee L, Bailleul F, Hamamah S (1998) Pre or post- operative medical treatment with nafarelin in stage III-IV endometriosis: a French multicentered study. Eur J Obstet Gynecol Reprod Biol 79:145–148
Steensma AB, Abbott JA, Broome JD, Vancaillie TG (2001) The role of second-look laparoscopy in treatment of women with endometriosis and pelvic pain. J Am Gynecol Laprascop 8:67–68
Ailawadi RK, Jobanputra S, Kataria M, Gurates B, Bulun SE (2004) Treatment of endometriosis and chronic pelvic pain with letrozole and norethindrone acetate: a pilot study. Fertil Steril 81:290–296
Amsterdam LL, Gentry W, Jobanputra S, Wolf M, Rubin SD, Bulun SE (2005) Anastrazole and oral contraceptives: a novel treatment for endometriosis. Fertil Steril 84:300–304
Remorgida V, Abbamonte HL, Ragni N, Fulcheri E, Ferrero S (2007) Letrozole and norethisterone acetate in rectovaginal endometriosis. Fertil Steril 88:724–726
Nowroozi K, Chase JS, Check JH (1987) The importance of laparoscopic coagulation of mild endometriosis in infertile women. Int J Fertil Steril 32:442–444
Guzick DS, Silliman NP, Adamson GD, Buttram VC, Canis M, Malinak LR, Schenken RS (1997) Prediction of pregnancy in infertile women based on the American Society for Reproductive Medicine’s revised classification of endometriosis. Fertil Steril 67:822–829
Stovall DW, Bowser LM, Arcer DF, Guzick DS (1997) Endometriosis-associated pelvic pain: evidence for an association between the stage of disease and a history of chronic pelvic pain. Fertil Steril 68:13–18
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alborzi, S., Hamedi, B., Omidvar, A. et al. A comparison of the effect of short-term aromatase inhibitor (letrozole) and GnRH agonist (triptorelin) versus case control on pregnancy rate and symptom and sign recurrence after laparoscopic treatment of endometriosis. Arch Gynecol Obstet 284, 105–110 (2011). https://doi.org/10.1007/s00404-010-1599-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-010-1599-6