Abstract
Purpose
To assess the diagnostic accuracy of endometrial thickness measurements of transvaginal ultrasound (TVUS) in asymptomatic postmenopausal women in the detection of endometrial malignancy.
Methods
A retrospective cohort study in a university hospital was undertaken with 276 consecutive asymptomatic postmenopausal women undergoing dilatation and curettage (D&C) and hysteroscopy for an incidental finding of thickened endometrium (≥4 mm) between 2003 and 2012. Different endometrial thickness cutoff values were tested on the basis of a pathologic report with carcinoma conditions (endometrial hyperplasia with atypia and endometrial carcinoma).
Results
The mean age of patients was 59.8 ± 9.0 years. The mean duration of menopause was 11.2 ± 8.9 years. The final pathology diagnoses included 107 (38.8 %) patients with polyps, 42 (15.2 %) with atrophic endometrium, 39 (14.1 %) with estrogen exposure, and 19 (6.9 %) with normal endometrium. With regard to carcinoma conditions, nine patients (3.3 %) had endometrial hyperplasia with atypia and eight patients (2.9 %) had endometrial carcinoma. The area under the ROC curve was 0.52 (95 % CI 0.44–0.57), which indicated a poor accuracy of endometrial thickness of TVUS for carcinoma conditions.
Conclusions
Routine use of endometrial thickness measurement with TVUS does not seem to be an effective diagnostic tool for endometrial cancer because it has a low diagnostic performance in asymptomatic postmenopausal women. Further prospective studies are required to assess the endometrial thickness measurement with TVUS as a screening method in these women.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Endometrial cancer is the most common gynecologic malignancy, and its incidence worldwide has risen over the last 20 years [1]. Every year about 200 000 new endometrial cancer cases are diagnosed around the world and an estimated 50 000 women die from this disease [2]. Endometrial cancer is mostly diagnosed in the sixth or seventh decade and 70 % of these cases are postmenopausal. Vaginal bleeding is the most common symptom; however, up to 20 % of patients who are diagnosed as having endometrial cancer are asymptomatic at the time of diagnosis [3].
Commonly used techniques in the assessment of endometrium in symptomatic postmenopausal women include transvaginal ultrasound (TVUS) for endometrial thickness, endometrial sampling, saline infusion sonography, and hysteroscopy [4, 5]. There is an accepted cutoff value of endometrial thickness (ET) of ≥5 mm for postmenopausal women who present with vaginal bleeding that warrants further investigation [6]. However, there is no well-established threshold ET value to direct pathologic evaluation of endometrium for asymptomatic postmenopausal women [7]. Asymptomatic women may undergo TVUS for pelvic organ prolapse or abdominal discomfort. The number of identified asymptomatic intrauterine lesions increases with use of high-frequency ultrasound examinations. Many physicians also use the same ≥5 mm cutoff level in asymptomatic patients due to the lack of clear threshold levels, which leads to inappropriate investigations with considerable physical and psychologic disabilities [8]. TVUS has been found to be an unreliable screening method in the detection of endometrial cancer with evaluation of ET in asymptomatic women [9, 10].
In this study, we aimed to evaluate the diagnostic value of endometrial thickness for the prediction of endometrial carcinoma in asymptomatic postmenopausal women.
Materials and methods
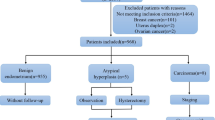
In this retrospective study, we reviewed the medical records of 276 consecutive postmenopausal patients who were referred to the outpatient clinic of Istanbul University School of Medicine for routine follow-ups from February 2003 to December 2012 after obtaining Ethics Committee approval of Istanbul University School of Medicine. Postmenopausal status was confirmed with a history of absence of menses within the last 12 months. Exclusion criteria included: (1) abnormal uterine bleeding; (2) history of endometrial pathologies such as hyperplasia or cancer; (3) history or current use of hormone replacement therapy; (4) use of raloxifene and/or tamoxifen.
Transvaginal ultrasonography was performed by three gynecologists, 40 % of which was performed by C.Y, 30 % by O.D., and the remaining 30 % was performed by F.G.U. Ultrasounds were performed for a variety of reasons including routine follow-up, pelvic pain, pelvic mass on examination and family history of gynecologic cancer. All three gynecologists used the same ultrasound scanner to perform the TVUS, a General Electric Logic 5 ultrasound unit (General Electric, Wauekesha, Wisc., USA) with a curved linear array 5-MHz endovaginal probe. A longitudinal axis view was used to obtain the baseline measurement of endometrial stripe thickness. During the measurement, the thickest section of the echo was selected. All patients had an empty bladder during TVUS. Only patients with an endometrial thickness of ≥4 mm were included in the study. Endometrial cavities were regarded abnormal when endometrial thickening of ≥4 mm or an endometrial lesion was observed. Also the women with intracavitary fluid collection were excluded from the study.
Patients’ medical records were reviewed for demographic characteristics, which were age, body mass index (BMI), age at menopause, gravity, and parity. All patients underwent endometrial evaluation with pipelle endometrial sampling either during hysteroscopy or alone, or fractional dilatation and curettage (D&C). The results of these tests were also collected for review.
All statistical analyses were performed using Statistical Package for Social Sciences version 20.0 (SPSS Inc., Chicago, IL, USA). Variables were presented with descriptive statistics (mean ± standard deviation for continuous variables and number and percentage for categorical variables). P values less than 0.05 were regarded as statistically significant. The receiver-operating characteristics (ROC) curve was prepared (plot of sensitivity vs. 1-specificity) and the areas under the curves (AUC) estimated. AUC = 1 indicates a perfect test, AUC >0.9 indicates high accuracy, and AUC between 0.7 and 0.9 indicates moderate accuracy.
Results
In total, 2358 consecutive postmenopausal women underwent TVUS examination between February 2003 and December 2012 and 276 of them met the inclusion criteria of the present study. The demographic characteristics of the 276 women are presented in Table 1. All patients were Caucasian and from the metropolitan area of Istanbul. The mean age of our study cohort was 59.8 years (SD = 9.0) with the last menstrual period being 11.22 years (SD = 8.89) earlier. Among risk factors for endometrial cancer, hypertension was present in 129 women (46.7 %) and diabetes mellitus was present in 53 women (19.2 %). The mean body mass index (BMI) was found as 29.67 kg/m2 (SD = 3.11). The mean endometrial thickness was 9.99 mm (SD = 3.59). Of these 276 women, 120 (43.5 %) had an endometrial thickness between 4 and 7 mm, 94 (34.1 %) 8 and 11 mm, and 62 (22.5 %) 12 mm or greater.
Two hundred sixteen (78.3 %) women underwent endometrial sampling via fractional dilatation and curettage (D&C), 60 women (21.7 %) via pipelle. Endometrial biopsies revealed an endometrial polyp in 107 women (38.8 %), atrophic endometrium in 42 (15.2 %), estrogen exposure in 39 (14.1 %), normal endometrium in 19 (6.9 %), and endometrial hyperplasia with atypia in nine women (3.3 %). There was insufficient sample in 52 women (18.8 %), and endometrial carcinoma was detected in eight (2.9 %).
A comparison of endometrial thickness and histologic findings is presented in Table 2.
The distribution of endometrial thickness according to benign or carcinoma conditions (endometrial hyperplasia with atypia and endometrial carcinoma) is given in Table 3. Carcinoma conditions were equally distributed according to endometrial thickness groups, six patients (2.1 %) had 4–7 mm, five patients (1.8 %) had 8–11 mm, and six patients (2.1 %) had ≥12 mm.
None of the endometrial thickness cutoff values showed optimal diagnostic accuracy for the detection of carcinoma conditions (Table 4.) The highest sensitivity (100 %) was found using a cutoff point of 4 mm. By increasing the cutoff point from 4 to 12 mm, the sensitivity decreases but the specificity increases.
A ROC curve was constructed and Fig. 1 shows the estimated diagnostic performance of TVUS measurements of endometrial thickness for the detection of endometrium carcinoma. The area under the ROC curve was 0.52 [95 % CI (0.44–0.57)].
Discussion
TVUS has been used as a first step in screening for endometrial cancer because of its high negative predictive value. In the literature, the most frequently used optimal threshold level of endometrial thickness measured using ultrasound to separate patients into low-risk and high-risk patients is 4–5 mm [6–12].
Lynch syndrome, a genetic disorder with a lifetime endometrial cancer risk of 40–60 %, is the only disease for which screening for endometrial cancer is recommended [13]. In the general population, there is no established screening method for endometrial cancers. Women at average or increased risk because of a history of unopposed estrogen therapy, tamoxifen therapy, late menopause, nulliparity, infertility, obesity, diabetes and hypertension should be informed about risks and symptoms and encouraged to report these symptoms to their physicians [14].
Our study shows that postmenopausal women without vaginal bleeding had endometrial thickness of ≥4 mm, and the prevalence of atypical endometrial hyperplasia and endometrial carcinoma was 3.3 and 2.9 %, respectively. Positive predictive values for carcinoma-related conditions (endometrial carcinoma and atypical endometrial hyperplasia) for all given endometrial thickness cutoff values were between 6.1 and 9.6 %. The negative predictive values of TVUS were between 94.8 and 100 % at all endometrial thickness cutoff values for carcinoma-related conditions. Furthermore, use of a negative test in asymptomatic postmenopausal women is very limited owing to the low absolute risk of disease.
TVUS has been the technique of choice for endometrial evaluation of postmenopausal bleeding over the last two decades because of its high accuracy and non-invasive nature [15]. The cutoff value for endometrial thickness measurement in asymptomatic postmenopausal women remains unclear. A recent study of endometrial thickness measurements in women with postmenopausal bleeding for detection of endometrial cancer reported that an endometrial thickness for 3 mm had a sensitivity of 97 % and a specificity of 45.3 %, for 4 mm 94.1 and 66.8 %, for 5 mm 93.5 and 74 %, respectively [16]. A variety of studies have been performed to establish cutoff levels of endometrial thickness to exclude malignancy and findings are equivocal. The United Kingdom Collaborative Trial of Ovarian Cancer Screening (UKCTOCS) involved 37,038 women in their cohort and aimed to provide information about endometrial thickness in asymptomatic women. They divided the study population into risk groups according to a logistic regression model and the high-risk population achieved sensitivity of 84.3 % and specificity of 89.9 % with a cutoff of 6.75 mm [17]. In a prospective cohort observational study, Kasraeian et al. studied over 259 postmenopausal women using 3- and 5-mm cutoff values during ultrasonographic evaluation for endometrial carcinoma. Using a cutoff point of 3 mm, the authors reported sensitivity, specificity, PPV and NPV of 100, 56.2, 0.87, and 100 %, respectively. When using 5 mm as a cutoff point, they found sensitivity of 100 %, specificity of 84.4 %, PPV of 2.43 %, and NPV of 100 % [18]. We also showed that TVUS with an AUC of 0.52 was poorly accurate for detecting carcinoma conditions in this group.
In our study, endometrial samples were reported as insufficient tissue in 52 (18.8 %) patients of the study group. All these women underwent hysteroscopic evaluation and we found no intrauterine pathology in this group. Ragupathy et al. reported that the rate of inadequate sampling might reach a level of 12 % in women with significant endometrial thickness (≥4 mm) [19].
The results from our study are inconsistent with conclusion of Smith-Bindman et al. who suggested a biopsy is not needed if the endometrium measures 11 mm or less, according to theoretical cohort [20]. In our study, there were 6 (2.1 %) cases of endometrial hyperplasia with atypia and 5 (1.8 %) cases of endometrial cancer with endometrial thickness of 11 mm or less, which accounts for 64.7 % of carcinoma conditions. In a retrospective study of 148 postmenopausal women without bleeding, one (0.7 %) case of endometrial cancer was found and in this patient endometrial thickness was 16 mm [21]. A similar retrospective study of 65 asymptomatic women found two (3.1 %) cases of atypia and no cases of cancer; the endometrial measurement was not stated [22].
Various endometrial sampling techniques, D&C, aspiration procedures and hysteroscopy, are used to diagnose endometrial abnormalities. Although D&C is currently considered as the gold standard for endometrial sampling, reports revealed that general accuracy rate of D&C was 70 % with additional risks of general anesthesia, infection and perforation [23]. As aspiration procedures, such as pipelle, are easy to perform, convenient, less expensive and general accuracy rate was 67 %, they become more popular [23]. Hysteroscopy has the advantage of achieving panoramic view of uterine cavity and giving opportunity to biopsies under direct vision. Diagnostic accuracy of hysteroscopy is high for endometrial cancer with sensitivity 82.6 % and specificity 99.7 % [24].
The major strengths of our study are the large sample size and that all TVUSs were performed by three experienced gynecologists in a dedicated menopausal clinic from which original data of patients over a 15-year period were available. Also, all women had received a definitive histologic diagnosis, which provided an optimal reference standard. The main limitations of our study stem from its retrospective nature and very low incidence of cancer-related conditions in the cohort, which results in poor information about very rare occurrences.
Conclusions
In line with previous studies, our analysis indicated that endometrial thickness cannot predict carcinoma conditions and provided poor diagnostic value in asymptomatic women. With low prevalence of atypical endometrial hyperplasia and endometrial cancer in asymptomatic postmenopausal women, involvement of TVUS endometrial thickness measurements in diagnostic tests for this group leads to an increase in the number of unnecessary examinations including benign intrauterine lesions and atrophy cases. As clinical characteristics are possible predictors of endometrial malignancy, the need for further diagnostic evaluation should be assessed on an individual basis. However, TVUS can be used to exclude pre-malignancy or malignancy in asymptomatic postmenopausal women with risk factors because of its low false negative rate. Also further prospective studies are required to assess the endometrial thickness measurement with TVUS as a screening method in these women.
References
von Gruenigen VE, Gil KM, Frasure HE, Jenison EL, Hopkins MP (2005) The impact of obesity and age on quality of life in gynecologic surgery. Am J Obstet Gynecol 193:1369–1375
Bray F, Loos AH, Oostindier M, Weiderpass E (2005) Geographic and temporal variations in cancer of the corpus uteri: incidence and mortality in pre- and post- menopausal women in Europe. Int J Cancer 117:123–131
Malkasian GD Jr, Annegers JF, Fountain KS (1980) Carcinoma of the endometrium: stage I. Am J Obstet Gynecol 136:872–888
Van Hanegem N, Breijer MC, Khan KS, Clark TJ, Burger MPM, Mol BJW, Timmermans A (2011) Diagnostic evaluation of the endometrium in postmenopausal bleeding: an evidence-based approach. Maturitas 68:155–164
Dimitraki M, Tsikouras P, Bouchlariotou S, Dafopoulas A, Liberis V, Maroulis G, Teichmann AT (2011) Clinical evaluation of women with PMB. Is it always necessary an endometrial biopsy to be performed? A review of literature. Arch Gynecol Obstet 283:261–266
Timmermans A, Opmeer BC, Khan KS, Bachmann LM, Epstein E, Clark TJ et al (2010) Endometrial thickness measurement for detecting endometrial cancer in women with postmenopausal bleeding: a systematic review and meta-analysis. Obstet Gynecol 116:160–167
Wolfman W, Leyland N, Heywood M, Singh SS, Rittenberg DA, Soucy R et al (2010) Asymptomatic endometrial thickening. J Onstet Gynaecol Can 32:990–999
Goldstein SR (2004) The endometrial echo revisited: have we created a monster? Am J Obstet Gynecol 191:1092–1096
Kanat-Pektas M, Gungor T, Mollamahmutoglu L (2008) The evaluation of endometrial tumors by transvaginal and Doppler ultrasonography. Arch Gynecol Obstet 277:495–499
Breijer MC, Peeters JA, Opmeer BC, Clark TJ, Verheijen RH, Mol BW, Timmermans A (2012) Capacity of endometrial thickness measurement to diagnose endometrial carcinoma in asymptomatic postmenopausal women: a systematic review and meta-analysis. Ultrasound Obstet Gynecol 40:621–629
Dueholm M, Marinovskij E, Hansen ES, Moller C, Ortoft G (2015) Diagnostic methods for fast-track identification of endometrial cancer in women with postmenopausal bleeding and endometrial thickness greater than 5 mm. Menopause 22:616–626
Smith-Bindman R, Kerlikowske K, Feldstein VA, Subak L, Scheidler J, Segal M, Brand R, Grady D (1998) Endometrial vaginal ultrasound to exclude endometrial cancer and other endometrial abnormalities. JAMA 280:1510–1517
Lynch HT, Lynch JF (2004) Lynch syndrome; history and current status. Dis Markers 20:181–198
Smith RA, Manassaram-Baptiste D, Brooks D, Doroshenk M, Fedewa S, Saslow D, Brawley OW, Wender R (2015) Cancer screening in the United States, 2015: a review of current American Cancer Society guidelines and issues in cancer screening. CA Cancer J Clin 65:30–54
Saidi MH, Sadler RK, Theis VD, Akright BD, Farhart SA, Villanueva GR (1997) Comparison of sonography, sonohysterography and hysteroscopy for evaluation of abnormal uterine bleeding. J Ultrasound Med 16:587–591
Wong AW, Lao TH, Cheung CW, Yeung SW, Fan HL, Ng PS, Yuen PM, Sahota DS (2015) Reappraisal of endometrial thickness for the detection of endometrial cancer in postmenopausal bleeding: a retrospective cohort study. BJOG. doi:10.1111/1471-0528.13342
Jacobs I, Gentry-Maharaj A, Burnell M, Mancahanda R, Singh N, Sharma A et al (2011) Sensitivity of transvaginal ultrasound screening for endometrial cancer in postmenopausal women: a case–control study within the UKCTOCS cohort. Lancet Oncol 12:38–48
Kasraeian M, Asadi N, Ghaffarpasand F, Karimi AA (2011) Value of transvaginal ultrasonography in endometrial evaluation of non-bleeding postmenopausal women. Climacteric 14:126–131
Ragupathy K, Cawley N, Ridout A, Igbal P, Alloub M (2013) Non-assessable endometrium in women with post-menopausal bleeding: to investigate or ignore. Arch Gynecol Obstet 288:375–378
Smith-Bindman R, Weiss E, Feldstein V (2004) How is too thick? When endometrial thickness should prompt biopsy in postmenopausal women without vaginal bleeding. Ultrasound Obstet Gynecol 24:558–565
Gambacianni M, Monteleonne P, Ciaponi M, Sacco A, Genazzani AR (2004) Clinical usefulness of endometrial screening by ultrasound in asymptomatic postmenopausal women. Maturitas 48:421–424
Jr Worley, Dean KL, Lin SN, Caputo TA, Post RC (2011) The significance of a thickened endometrial echo in asymptomatic postmenopausal patients. Maturitas 68:179–181
Demirkıran F, Yavuz E, Erenel H, Bese T, Arvas M, Sanioglu C (2012) Which is the best technique for endometrial sampling? Aspiration (pipelle) versus dilatation and curettage (D&C). Arch Gynecol Obstet 286:1277–1282
Gkrozou F, Dimakopoulos G, Vrekoussis T, Lavasidis L, Koutlas A, Navrozoglou I, Stefos T, Paschopoulos M (2015) Hysteroscopy in women with abnormal uterine bleeding: a meta-analysis on four major endometrial pathologies. Arch Gynecol Obstet 291:1347–1354
Acknowledgments
The authors thank David F. Chapman for language editing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
Authors declare that they have all participated in the design, execution, and analysis of the paper, and that they have approved the final version. Additionally, there are no conflicts of interest in connection with this paper.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Yasa, C., Dural, O., Bastu, E. et al. Evaluation of the diagnostic role of transvaginal ultrasound measurements of endometrial thickness to detect endometrial malignancy in asymptomatic postmenopausal women. Arch Gynecol Obstet 294, 311–316 (2016). https://doi.org/10.1007/s00404-016-4054-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4054-5