Abstract
Purpose
To compare the clinical and perinatal outcomes in eclamptic women with and without posterior reversible encephalopathy syndrome (PRES).
Methods
This single-center, retrospective, cohort study was conducted between 2008 and 2013. The clinical and perinatal outcomes of eclamptic patients were obtained from hospital records. Magnetic resonance imaging was used for the diagnosis of PRES. Eighty-one eclamptic women were divided into two groups: 45 and 36 patients were included in the PRES and non-PRES groups, respectively.
Results
In the PRES group, headache and visual impairment together (60.0 %) were the most common presenting symptoms. In the non-PRES group, only headache was the most common (50 %) presenting symptom. Occipital and parietal lobes were the most frequently affected areas in the PRES group. Women in the PRES group had a higher body mass index value (p = 0.005), longer hospitalization time (p = 0.001), and higher level of proteinuria (p = 0.012) than those in the non-PRES group. Women in the non-PRES group had higher Apgar scores (p = 0.002) than those in the PRES group.
Conclusions
This study indicates that PRES manifests predominantly with headache and visual impairment together. Adverse neonatal outcomes are also common in these patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pre-eclampsia is a syndrome characterized by hypertension (>140/90 mmHg on two separate occasions at least 6 h apart) and proteinuria as >300 mg in 24 h between the 20th week of gestation and the sixth postpartum week. It is seen in 3–10 % of pregnant women. Pre-eclampsia is usually associated with neurologic symptoms such as visual deficits, headache, reduced consciousness, and confusion [1, 2]. Together with pre-eclampsia symptoms and signs, the occurrence of seizures unrelated to other cerebral conditions is called eclampsia [3].
Posterior reversible encephalopathy syndrome (PRES) was first described by Hinchey et al. in 1996. It is a clinico-radiological entity with a varying combination of symptoms and signs including headache, visual abnormalities, nausea, vomiting, impaired consciousness, seizure activity, and focal neurologic deficits [4–6]. Some other conditions including autoimmune disease, severe hypertension, transplantation, cytotoxic drugs, sepsis, and immunosuppressive therapy have been shown to be associated with PRES [7]. Although its pathophysiology is poorly understood, the same pathophysiological mechanisms of eclampsia are shared. Typically, parieto-occipital and vasogenic cerebral edema are reversible [4, 8]. Typical systemic processes having an inflammatory response and some degree of endothelial dysfunction constitute the conditions associated with PRES. An increased vulnerability of the cerebral vasculature to loss of autoregulation is possibly predisposed by the causative conditions and other unidentified processes. A shift of the cerebral autoregulation curve to the left or increased permeability of the blood–brain barrier or both may be the reason for it [9].
Hyperintensity on fluid attenuated inversion recovery (FLAIR) magnetic resonance imaging (MRI) is the typical imaging finding of PRES. However, some atypical imaging findings like contrast enhancement, various patterns of distribution, hemorrhage, infarction, and cytotoxic edema have also been recognized recently [10, 11].
Neuroimaging findings of PRES have been described in scores of eclamptic patients, usually in single case reports or small case series. In the literature, there is no large series revealing the relationship between eclampsia and PRES. Which eclamptic patients develop PRES remains a mystery. The aim of this study was to obtain insight about the association between eclampsia and PRES by comparing clinical, maternal, and perinatal outcomes.
Materials and methods
This single-center, retrospective cohort study was approved by the institutional ethics committee of Yuzuncu Yıl University in Van. The study included 81 eclamptic women who were diagnosed at the obstetric clinic of the Yuzuncu Yıl University Hospital between 2008 and 2013. The pregnant women with eclampsia occurring after week 20 of gestation or within 6 weeks of the postpartum period were included. Exclusion criteria were any history of neurologic disorders (e.g., epilepsy, cerebrovascular accident, cerebral hemorrhage, demyelinating disorders, intracranial infections, cranial surgery) and multiple pregnancy.
We investigated all women diagnosed with eclampsia who underwent neuroimaging studies upon admission to our tertiary care referral hospital. All patients were divided into two groups: PRES group (n = 45) and non-PRES group (n = 36). Demographic data, initial neurological symptoms, blood pressure level, and related symptoms were recorded.
An onset of hypertension with a blood pressure of ≥140/90 mmHg measured 6 h apart together with constant proteinuria of ≥300 mg/day and epileptic seizures in the second half of the gestation remitting remotely after delivery was defined as eclampsia.
We included all patients underwent whole-brain MR imaging with a standard head coil on a 1.5 T system (Magneton Vision, Siemens, Erlangen, Germany). The diagnosis was made by using the standard radiological criteria for PRES, i.e., a unique MRI imaging appearance demonstrated as a subcortical and gyral fluid attenuated inversion recovery (FLAIR) and T2-weighted signal hyperintensities that become more diffuse as the external edema increases. Focal areas include symmetric multilobar/hemispheric edema with involvement of parieto-occipital lobes, predominantly. All eclamptic patients received intravenous MgSO4 at a rate of 1 g/h for 24 h. All patients in group 1 were applied supportive therapy for PRES.
The perinatal outcomes of pregnant women including birth weight, gestational age at birth, small for gestational age (SGA), Apgar scores, stillbirth, early neonatal death, admission to the neonatal intensive care unit, mode of delivery, history of pre-eclampsia and timing of convulsions were obtained from hospital records. According to customized curves, SGA was defined as a birth weight <10th percentile. One-third of the systolic pressure plus 2/3 of the diastolic pressure was used to calculate the mean arterial pressure.
Statistical analyses
Descriptive statistics for continuous variables (characteristics) were presented as mean ± standard deviation, while categorical variables were presented as numbers and percentages. Student’s t test was used to compare the means of the PRES and non-PRES groups for the variables studied. A two proportions Z test was used for comparison of percentage values. Statistical significance level was considered as 5 % and SPSS (version 13) was used for all statistical analyses.
Results
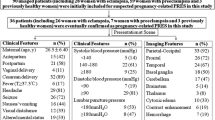
We managed to obtain the records of 81 patients diagnosed with eclampsia. Among the 81 eclamptic women, 45 patients were in the PRES group (group 1) and 36 in the non-PRES group (group 2). The mean gestational age of all patients at delivery was 33.45 ± 4.19 weeks and total mean birth weight was 2039.75 ± 874.82 g. Overall, the perinatal mortality rate was 19.75 %. There was no maternal mortality in the study population. The demographic, clinical characteristics and presenting symptoms of the patients with eclampsia are presented in Table 1. Among the 81 patients, 58 (71.6 %) had convulsions during the antepartum period, while 23 patients (28.4 %) had convulsions during the postpartum period.
The gestational age at birth ranged between 23 and 40 weeks, with median values of 33.4 and 33.5 weeks for groups 1 and 2, respectively (Table 1). Mean gravidity was 3.73 for group 1 and 3.94 for group 2. In groups 1 and 2, mean parity values were 2.49 and 2.25, respectively. Of the patients in group 1, 14 (31.1 %) were nulliparous, while 5 were nulliparous (13.9 %) in group 2. There was no significant difference between the groups in terms of gravidity, parity, nulliparity, blood pressure level, or mean arterial pressure. Group 1 had a higher body mass index (BMI) value (p = 0.005), longer hospitalization time (p = 0.001), and higher proteinuria level (p = 0.012) compared to group 2. Vaginal delivery and cesarean section rates were similar between the groups (26.7 and 73.3 % for group 1 and 22.2 and 77.8 % for group 2, respectively). PRES ratio were 60 % (12/20), 54.1 % (33/61) in patients with vaginal delivery and cesarean section, respectively. Of the patients in group 1, 10 (22.2 %) had a history of pre-eclampsia; while only 5 (13.9 %) patients in group 2 had a history of pre-eclampsia. In group 1, 35 (77.8 %) and 10 (22.2 %) patients had convulsions during the antepartum and postpartum periods, respectively. Of the patients in group 2, 23 (63.9 %) had convulsions during the antepartum period, while 13 (36.1 %) had convulsions during the postpartum period. The groups did not show any significant difference with respect to history of pre-eclampsia and convulsions during the antepartum/postpartum periods (p = 0.337 and p = 0.168, respectively). Headache and visual impairment together (60.0 %) was the most common presenting symptom followed by only visual impairment (26.7 %) in the PRES group. In the non-PRES group, only headache (50.0 %) was the most common symptom followed by epigastric tenderness (25.0 %). The symptoms of headache and visual impairment together and only visual impairment were more frequent in the PRES group than they were in the non-PRES group (p = 0.001 and p = 0.006, respectively). On the other hand, headache, epigastric tenderness, and other symptoms (nausea, vomiting, altered mental status, photophobia) were more frequent in the non-PRES group than they were in the PRES group (p = 0.001, p = 0.008, and p = 0.036, respectively).
The location of brain lesions in patients with PRES were distributed as 21 patients (46.7 %) in occipital lobe, 6 patients (13.3 %) in parietal lobe, 1 patient (2.2 %) in frontal lobe, 1 patient (2.2 %) in basal ganglia/cerebellum and 15 patients (33.3 %) in multiple areas. Occipital and parietal lobes were the most commonly affected areas in group 1 (46.7 and 13.3 %, respectively) (Fig. 1). Table 2 shows perinatal outcomes of groups 1 and 2. Early neonatal death in group 1 was 19 % (8 patients) while it was 15.2 % (5 patients) in group 2. In groups 1 and 2, 21 (46.6 %) and 22 babies (60.1 %) were admitted to the neonatal intensive care unit (NICU), respectively. The rate of stillbirth in group 1 was 6.7 % (3 patients) and all of them occurred between 23 and 25 weeks of gestation, while no stillbirth was observed in group 2. However, the difference between the groups was not statistically significant (p = 0.111). The perinatal mortality rate was 19.75 % and there was no maternal mortality in the study population. All of the neonatal deaths were due to complications of perinatal asphyxia (n = 5), respiratory distress syndrome (n = 4), early neonatal sepsis (n = 2), and necrotizing enterocolitis (n = 2).
a Diffusion weighted MRI demonstrates hyperintensive signal alterations predominantly in the areas of parietal and occipital lobes. b Axial FLAIR MRI shows edematous lesions in frontal and occipital lobes. c Axial FLAIR MRI demonstrates extensive vasogenic edema in the temporal and occipital lobes, bilaterally. d Axial FLAIR MRI shows an edema formation in mesencephalon and occipital lobes
Discussion
Our study presents clinical and perinatal outcomes of eclamptic women with and without PRES at a single tertiary referral center in eastern Turkey. Eclampsia is a rare and potentially life-threatening complication of hypertensive disorders in pregnancy [12, 13]. PRES is defined as a vasogenic edema associated with disruption of the blood–brain barrier. The abnormalities in MRI include both gray and white matter, commonly as bilateral hypointensities in the posterior parietal, occipital, or high frontal lobes. If adequate treatment (mainly magnesium sulfate administration and a decrease in blood pressure) is started, these abnormalities are reversible in most cases [14].
The symptoms of PRES include nausea/vomiting, decreased alertness, headache, impairment in vision (cortical blindness and blurred vision), and alteration in mental status [15]. Usually, the symptoms develop very quickly over a few hours and reach their worst in 12–48 h. Over several days, progression is common, and symptoms usually resolve within a week but in a few cases, they may persist for longer. In patients with PRES, visual loss and headache have been emphasized by most authors but seizure is the most frequent finding, seen in up to 90 % of cases and often preceding any of the other manifestations [6]. In the present study, all of the patients had seizures and the main symptom of PRES was headache and visual impairment (60.0 %) together. These two symptoms were not observed together in the non-PRES group. Only headache (without visual impairment) was the most common symptom in the non-PRES group. Patients in the non-PRES group had a greater tendency to have epigastric tenderness and other symptoms compared to the PRES group.
Eclamptic convulsions can begin during the antepartum period in 50 % of cases, during labor in 25 % of cases, and at the postpartum period in the rest [16]. In our study group, 71.6 and 28.4 % of the patients had eclamptic convulsions during the antepartum and postpartum periods, respectively. The frequency of PRES was similar in eclamptic patients during the antepartum and postpartum periods (p > 0.05).
The current popular theory for the brain edema that develops in PRES includes severe hypertension associated with failed autoregulation, injury to the capillary bed, and hyperperfusion [15, 17]. Autoregulation is limited by approximately 50–150 mmHg mean arterial pressure [18, 19]. When the blood pressure increases beyond the autoregulatory upper limit, studies in animals showed vessel injury with alteration in arterial morphology, breakthrough with passive dilatation in arteries, and pinocytic transfer of fluid [19]. Vasoconstriction secondary to evolving hypertension and autoregulatory compensation leading to reduced brain perfusion, ischemia, and subsequent vasogenic edema is suggested by the early original theory [20]. PRES, therefore, can develop in patients with only mild blood pressure elevation as well as in normotensive patients [3]. As normal cerebral autoregulation requires an intact vascular endothelium, breakthrough of the blood–brain barrier may also take place in the setting of mild hypertension and endothelial damage. In our study, hypertension was not found to reach the upper limit of autoregulation in the PRES group (mean arterial pressure value = 120.31 ± 16.65 mmHg). Additionally, there was no significant difference in mean arterial pressure values between the PRES and non-PRES groups (p = 0.461).
Late autopsy studies have described evidence of acute and chronic endothelial injury in PRES patients with the identification of segmental vessel narrowing, intimal thickening with dissection, and organized thrombi [21, 22]. Renal dysfunction associated with proteinuria leads to systemic edema as a result of a combination of reduced oncotic pressure and altered endothelial function. In our study, patients in the PRES group had higher BMI and proteinuria levels than those in the non-PRES group (p = 0.005 and p = 0.012, respectively). In PRES, vasogenic edema occurs when there is a breakthrough of the blood–brain barrier allowing the intravascular proteins and fluid to penetrate into the parenchymal extracellular space. PRES has also been associated with various non-obstetric systemic conditions such as systemic lupus erythematosus, acute glomerulonephritis, and immunosuppressive therapy [23–25].
Neuroimaging is essential for the diagnosis of PRES and radiological abnormalities are best demonstrated by MRI [26]. Areas of hyperintensive signal are shown by T2 weighted MRI, which is thought to capture the images with the best quality. However, fluid attenuated inversion recovery (FLAIR) sequences may help to distinguish vasogenic edema from cytotoxic edema by improving the detection of cortical/subcortical areas of injury [27]. On FLAIR MRI, PRES is usually characterized by parieto-occipital white matter edema [28]. In our study, the most affected brain region associated with PRES was the parieto-occipital lobe (60.0 %), which was in accordance with the literature. As a result of this study, we recommend MRI only for eclamptic patients with headache and visual impairment together.
Nearly 18 % of all maternal deaths worldwide are due to hypertensive disorders of pregnancy, with approximately 62,000–77,000 deaths per year [29]. According to the World Health Organization Multicountry Survey on Maternal and Newborn Health (WHOMCS) database, the global incidence of eclampsia was 0.28 % of all deliveries and the maternal mortality rate was 3.66 % in pregnant women with eclampsia [30]. Prior studies suggest that PRES with eclampsia was relatively protective against a fatal outcome than PRES in non-obstetric patients [31, 32]. In accordance with this finding, there was no maternal mortality in our study population. Although gestational age at birth and birth weight values were similar between the groups, Apgar score at birth was low in the PRES patients. In addition, perinatal mortality rate was higher in the PRES group (24.4 and 13.9 %, respectively).
Conclusion
Adverse neonatal outcomes are more common in eclamptic patients with PRES and it manifests predominantly with headache and visual impairment together. In eclamptic patients with PRES, mean blood pressure may not reach the upper limit of autoregulation. Among obstetricians, the detection rate of this probably under-recognized condition is expected to increase through increasing awareness of PRES.
References
Schwartz RB, Feske SK, Polak JF et al (2000) Preeclampsia eclampsia: clinical and neuroradiographic correlates and insights into the pathogenesis of hypertensive encephalopathy. Radiology 217:371–376
Zeeman GG (2009) Neurologic complications of pre-eclampsia. Semin Perinatol 33:166–172
Sibai BM (1990) Eclampsia VI. Maternal-perinatal outcome in 254 consecutive cases. Am J Obstet Gynecol 163:1049–1055
Hinchey J, Chaves C, Appignani B et al (1996) A reversible posterior leukoencephalopathy syndrome. N Engl J Med 334:494–500
Pula JH, Eggenberger E (2008) Posterior reversible encephalopathy syndrome. Curr Opin Ophthalmol 19(6):479–484
Roth C, Ferbert A (2011) The posterior reversible encephalopathy syndrome: what’s certain, what’s new? Pract Neurol 11:136–144
Sraykov D, Schwab S (2012) Posterior reversible encephalopathy syndrome. J Intensive Care Med 27:11–24
Zhang HL, Mao XJ, Zheng XY, Wu J (2010) Posterior reversible encephalopathy syndrome: imperative to define. Arch Neurol 67:1536–1537
Bartynski WS (2008) Posterior reversible encephalopathy syndrome, part 2: controversies surrounding pathophysiology of vasogenic edema. Am J Neuroradiol 29:1043–1049
Hefzy HM, Bartynski WS, Boardman JF, Lacomis D (2009) Hemorrhage in posterior reversible encephalopathy syndrome: imaging and clinical features. Am J Neuroradiol 30(7):1371–1379
Sharma A, Whitesell RT, Moran KJ (2010) Imaging pattern of intracranial hemorrhage in the setting of posterior reversible encephalopathy syndrome. Neuroradiology 52(10):855–863
Duley L (2009) The global impact of pre-eclampsia and eclampsia. Semin Perinatol 33(3):130–137
Fong A, Chau CT, Pan D, Ogunyemi DA (2013) Clinical morbidities, trends, and demographics of eclampsia: a population-based study. Am J Obstet Gynecol 209(3):229.e1–229.e7
Karumanchi SA, Lindheimer MD (2008) Advances in the understanding of eclampsia. Curr Hypertens Rep 10:305–312
Schwartz RB, Jones KM, Kalina P, Bajakian RL, Mantello MT, Garada B et al (1992) Hypertensive encephalopathy: wndings on CT, MR imaging, and SPECT imaging in 14 cases. Am J Roentgenol 159:379–383
Sibai BM, Abdella TN, Taylor HA (1982) Eclampsia in the first half of pregnancy. J Reprod Med 27:706
Dinsdale HB (1983) Hypertensive encephalopathy. Neurol Clin 1:3–16
Zwienenberg-Lee M, Muizelaar JP (2004) Clinical pathophysiology of traumatic brain injury. In: Winn HR (ed) Youmans neurological surgery, 5th edn. Saunders, Philadelphia, pp 5039–64
Auer LM (1978) The pathogenesis of hypertensive encephalopathy: experimental data and their clinical relevance with special reference to neurosurgical patients. Acta Neurochir Suppl 27:1–111
Toole JF (1999) Lacunar syndromes and hypertensive encephalopathy. In: Toole JF (ed) Cerebrovascular disorders, 5th ed. Raven, New York, pp 342–55
Bartynski WS, Zeigler Z, Spearman MP et al (2001) Etiology of cortical and white matter lesions in cyclosporin-A and FK-506 neurotoxicity. Am J Neuroradiol 22:1901–1914
Schiff D, Lopes MB (2005) Neuropathological correlates of reversible posterior leukoencephalopathy. Neurocrit Care 2:303–305
Stott VL, Hurrell MA, Anderson TJ (2005) Reversible posterior leukoencephalopathy syndrome: a misnomer reviewed. Intern Med J 35:83–90
Bartynski WS, Tan HP, Boardman JF, Shapiro R, Marsh JW (2008) Posterior reversible encephalopathy syndrome after solid organ transplantation. Am J Neuroradiol 29:924–930
Lamy C, Oppenheim C, M´eder JF, Mas JL (2004) Neuroimaging in posterior reversible encephalopathy syndrome. J Neuroimaging 14:89–96
Burnett M, Hess C, Roberts J, Bass N, Douglas V, Josephson SA (2010) Presentation of reversible posterior leukoencephalopathy syndrome in patients on calcineurin inhibitors. Clin Neurol Neurosurg 112:886–891
Fugate JE, Claassen DO, Cloft HJ, Kallmes DF, Kozak OS, Rabinstein AA (2010) Posterior reversible encephalopathy syndrome: associated clinical and radiologic findings. Mayo Clin Proc 85:427–432
Mckinney AM, Short J, Truwit LC, Mckinney ZJ, Kozak OS, SantaCruz KS et al (2007) Posterior reversible encephalopathy syndrome: incidence of atypical regions of involvement and imaging findings. Am J Radiol 189:904–912
Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF (2006) WHO analysis of causes of maternal death: a systematic review. Lancet 367:1066–1074
Abalos E, Cuesta C, Carroli G, Qureshi Z, Widmer M, Vogel JP, Souza JP (2014) Preeclampsia, eclampsia and adverse maternal and perinatal outcomes: a secondary analysis of the World Health Organization Multicountry Survey on Maternal and Newborn Health. BJOG 121:14–24
Liman TG, Bohner G, Heuschmann PU, Scheel M, Endres M, Siebert E (2012) Clinical and radiological differences in posterior reversible encephalopathy syndrome between patients with preeclampsia–eclampsia and other predisposing diseases. Eur J Neurol 19:935–943
Pande AR, Ando K, Ishikura R, Nagami Y, Wada A, Watanabe Y et al (2006) Clinicoradiological factors influencing the reversibility of posterior reversible encephalopathy syndrome: a multicenter study. Radiat Med 24:659–668
Acknowledgments
The authors indicated that there was no financial relationship with the organization that sponsored the research.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kurdoglu, Z., Cetin, O., Sayın, R. et al. Clinical and perinatal outcomes in eclamptic women with posterior reversible encephalopathy syndrome. Arch Gynecol Obstet 292, 1013–1018 (2015). https://doi.org/10.1007/s00404-015-3738-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-015-3738-6