Abstract
Purpose
The present study aimed to correlate anti-Müllerian hormone (AMH) levels in follicular fluid (FF) with oocyte maturity stages, morphological quality of metaphase II (MII) oocyte and fertilization capacity of MII oocytes.
Methods
A total of 92 infertile women undergoing controlled ovarian stimulation and intracytoplasmic sperm injection were analyzed. Patients were divided into two groups according to age: <35 years (n = 43) and ≥35 years (n = 49). An FF sample was obtained from a single dominant follicle in each patient for a total of 92 follicular fluid samples analyzed. AMH levels in serum and follicular fluid were measured by enzyme-linked immunosorbent assay. Mature MII oocytes, zygotes, and embryos were assessed for morphological quality.
Results
Serum AMH levels were significantly higher in patients aged <35 years. No correlation was observed between FF AMH level and oocyte maturation stages or morphological quality of MII oocyte. Significantly lower FF AMH levels were observed in fertilized MII oocytes than in non-fertilized MII oocytes in patients aged <35 years (2.56 ± 2.0 ng/ml vs. 4.81 ± 4.14 ng/ml; p = 0.032).
Conclusions
The present study revealed no correlation between FF AMH and oocyte maturity stage or morphological quality of MII oocyte. However, FF AMH might be a predictive marker for fertilization capacity of MII oocytes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oocyte quality is a key factor of success in artificial reproductive technology (ART). The intrinsic developmental potential of an oocyte has a crucial role in fertilization and embryo development [1]. Oocyte quality is affected by the age of the woman, ovarian reserve, controlled ovarian stimulation protocol, and the composition of follicular fluid [2, 3]. Follicular fluid (FF) is a product of secretory activity of granulosa and thecal cells and provides a very important microenvironment for the development of oocytes [4]. Some biochemical substances of the FF surrounding the oocyte may play a critical role in determining oocyte quality and consequently the capacity of fertilization and embryo development [5].
From July 2009 to August 2012 in Croatia, a restrictive law regulating assisted reproduction limited the number of oocytes that could be inseminated to a maximum of three oocytes per cycle. Any remaining mature oocytes were cryopreserved, and embryo cryopreservation was forbidden. The selection of three female gametes for IVF/ICSI treatment was made on the basis of morphological aspects of the oocyte. In the case of conventional IVF, the evaluation of oocyte maturity was based on the expansion and radiance of the cumulus-corona complex surrounding the collected oocyte [6]. In the case of ICSI, metaphase II (MII) oocyte of good morphology implies a clear, moderately granular cytoplasm, a small perivitelline space, an intact first polar body, and a colorless zona pellucida [7, 8]. Due to the small number of oocytes in which insemination was permitted and the difficulties regarding morphological assessment in the cases of conventional IVF, law restrictions had negative effects on fertilization and pregnancy rates.
An assessment of morphology often fails to predict the oocytes fertilization and developmental capacity [9] and until today, many studies have been made to find a biochemical predictor of the functional viability of oocyte and embryo in follicular fluid [5]. It was showed that follicular fluid anti-Müllerian hormone (AMH), may play a critical role in determining the highest quality oocyte [3, 5]. Serum AMH has been evaluated as a novel clinical marker of ovarian reserve [10–13] with a poor ability to predict pregnancy after IVF [14]. Several studies have found a positive correlation between serum AMH levels and oocyte quality [15, 16], fertilization rate [17, 18], embryo morphology [19, 20] and blastocyst development [21], but results are inconsistent [22–25]. Very few studies have been published so far on the relationship of follicular fluid AMH levels and the quality of oocytes and embryos, and results are still controversial [26–32].
With the intention to minimize the negative effect of law restrictions on fertilization and pregnancy rate, we focused our research on oocyte selection and clarifying the relationship between follicular fluid AMH and oocyte quality. The aim of the present study was to assess whether FF AMH level might be a predictive marker for the selection of mature MII oocytes and whether FF AMH levels correlate with the morphological quality of MII oocytes and the fertilization capacity of MII oocytes.
Materials and methods
This study was performed at the Reproductive Unit of the Department of Obstetrics and Gynecology, Clinical Hospital Center Rijeka, University of Rijeka. Ninety-two patients, aged 26–43 (mean age 34 ± 4 years), undergoing controlled ovarian stimulation and ICSI treatment at our Center between August 2010 and July 2011 were included in this study, regardless of the previous treatment history. The inclusion criteria for women were normal ovulatory cycles and a body mass index (BMI) ranging from 18 to 28 kg/m2. Couples with a male diagnosis of severe oligoasthenozoospermia (fresh sperm concentration <1 × 106/ml, motility <30 %) were excluded from the study. Two groups of patients were formed according to age: <35 (n = 43) and ≥35 years (n = 49). Serum levels of follicle-stimulating hormone (FSH), luteinizing hormone (LH), prolactin (PRL), and anti-Müllerian hormone (AMH) were determined. Women with endocrine abnormalities, such as polycystic ovarian syndrome or hyperprolactinemia, were excluded from the study.
All patients received the luteal down-regulation protocol with the gonadotropin-releasing hormone (GnRH) agonist triptorelin (Decapeptyl, Ferring Pharmaceuticals, Düsseldorf, Germany). After pituitary suppression was achieved, ovarian stimulation was initiated with recombinant FSH (rFSH) (follitropin alfa, Gonal-F, Serono, Geneva, Switzerland) or human menopausal gonadotropin (HP-hMG) (Menopur, Ferring Pharmaceuticals A/S, Copenhagen, Denmark). Ovulation was induced with hCG (Choragon, Ferring Pharmaceuticals, Düsseldorf, Germany) when more than two follicles with a diameter of ≥17 mm were present. Oocyte retrieval was performed 34–36 h after hCG injection under transvaginal ultrasound guidance. Embryo transfer was performed 3 days later. Luteal support (Utrogestane, Laboratoires Besins International, Montrouge, France) was provided from the day of embryo transfer until 12 weeks of gestational age or negative serum hCG test (3 weeks after embryo transfer). Each pregnancy was confirmed as a normal intrauterine pregnancy with a live embryo by ultrasonography.
Follicular fluids (FF) were aspirated under transvaginal ultrasound guidance. The FF from the single dominant follicle of each patient (which is aspirated first) was separated and maintained at steady temperature conditions (37 °C) until the oocyte was identified and isolated. The oocyte from the dominant follicle was cultivated separately (Fertilization Medium, Cook, Limerick, Ireland). FF samples were centrifuged at 500 g for 15 min to remove cellular elements, aliquoted and frozen at −20 °C.
Blood samples were collected on day 3 of the menstrual cycle and the serum was stored at −20 °C. FSH, LH, and PRL concentrations in serum were determined by electrochemiluminescence immunoassay (Roche Diagnostics GmbH, Mannheim, Germany). AMH levels in serum and follicular fluid were measured by enzyme-linked immunosorbent assay (Immunotech-Beckman-Coulter, Marseilles, France). The assay range was 0–20.4 ng/ml with a functional sensitivity of 0.08 ng/ml. Intra-assay and inter-assay coefficients of variation were <8 %.
Two to four hours after retrieval, oocytes were denuded using the enzyme hyaluronidase (Hyadase, Cook, Limerick, Ireland). Denuded oocytes were assessed for the maturity stage. MII oocytes were identified by the presence of the first polar body. Metaphase I oocytes (MI stage) were identified by the absence of the germinal vesicle (GV) and the first polar body. Prophase I oocytes (PI stage) were identified by the presence of the germinal vesicle. Atretic and aged oocytes were recognized by breakdown of the zona pellucida during the denuding procedure. The ICSI procedure was performed 3–6 h after oocyte retrieval as published previously [33]. MII oocytes were assessed for morphological quality before and during the ICSI procedure on 200× magnification (Olympus IX51, Japan). Three morphologic and one functional parameter were assessed: the presence and morphology of the first polar body, the presence of central granularity, the presence of inclusions and vacuoles, and the resistance of the plasma membrane at ICSI [34–37]. MII oocytes were graded using a three-point scoring system: oocytes without any irregularities were graded as excellent-quality, oocytes with one irregularity were graded as good-quality, and oocytes with two or more irregularities were graded as poor-quality oocytes. Graded and injected oocytes were cultured separately.
The fertilization rate was assessed 16–18 h after the ICSI procedure (Day 1). Fertilized oocytes (zygotes) were graded with respect to the size of the two pronuclei, the arrangement of nucleolar precursor bodies, and the presence of the halo effect, as described previously [38–40]. Zygotes were graded using a three-point scoring system: zygotes without any irregularities were graded as excellent-quality, zygotes with one irregularity were graded as good-quality, and zygotes with two or more irregularities were graded as poor-quality zygotes.
Embryo cleavage rate and morphology were evaluated 64–76 h after ICSI (Day 3). Embryo morphology was graded according to the number of blastomeres, the evenness of blastomeres, and the relative proportion of fragmentation [6, 41, 42]. A three-point scoring system was used for embryo grading: embryos with seven or more cells, equally sized blastomeres, and <20 % fragmentation, were graded as excellent-quality; embryos with four to six cells, equally or unequally sized blastomeres, and <20 % fragmentation were graded as good-quality; embryos with less than four cells or with >50 % fragmentation were graded as poor-quality.
Statistical analysis
Depending on the data characteristics (e.g., group size, measurement scale of a parameter, group variance, and data distribution), parametric or non-parametric tests for group comparison were applied. Student’s t tests were used to examine differences between patients aged <35 and ≥35 in patients characteristics and ovarian response (Table 1). The χ 2 tests were used to examined differences between patients aged <35 and ≥35 in maturity stages of oocytes, morphological quality of MII oocytes, zygotes and embryos, and fertilized oocytes (Table 1). Student’s t tests were used to examine differences between MII oocytes and immature/atretic oocytes in follicular fluid AMH levels (Tables 2, 3). To examine differences in follicular fluid AMH levels between fertilized oocytes and non-fertilized oocytes Student’s t tests were used (Tables 2, 3). When comparisons were made between morphological excellent-quality, good-quality, and poor-quality MII ooyctes and embryos in follicular fluid AMH levels analyses of variance (ANOVAs) were applied (Table 2, 3). In some cases (e.g., uniquely group sizes in Tables 2, 3), the results of parametric tests (t test and ANOVA) were re-examined using non-parametric tests (the Mann–Whitney U test and the Kruskal–Wallis test). The results of the non-parametric tests supported our conclusions based on the results of the parametric tests. Results are presented in tables as mean ± standard deviation (SD) and number/total number (%). Statistical significance was set at p < 0.05 for all analyses. Data were analyzed using the software Statistical Package for Social Sciences version 17 (SPSS, USA).
Results
No significant differences were observed in BMI, FSH, LH, and PRL levels among groups. Serum AMH levels were significantly lower in patients aged ≥35 years compared to patients aged <35 years (Table 1). There was no significant difference in the number of oocytes retrieved after controlled ovarian stimulation between groups according to age (Table 1).
No significant differences were observed with respect to two different gonadotropins used in controlled ovarian stimulation (rFSH and HP-hMG) in terms of mean age, BMI, FSH, LH, PRL, serum AMH level, number of oocytes retrieved, embryo quality rate, and FF AMH level (data not shown).
There was no significant difference in percentages of maturity stages of oocytes, morphological quality of MII oocytes, fertilized oocytes, and morphological quality of zygotes between groups (Table 1). Patients aged <35 years had significantly higher percentages of morphological good-quality embryos (Table 1).
No significant difference of FF AMH levels between MII oocytes and immature/atretic oocytes were observed in patients <35 years (Table 2) and in patients ≥35 years (Table 3). There was no significant difference in the FF AMH levels in relation to the morphological quality of MII oocytes and embryos in patients <35 years (Table 2) and in patients ≥35 years (Table 3).
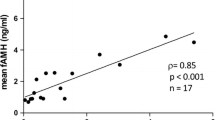
FF AMH levels were significantly lower in fertilized MII oocytes than in non-fertilized MII oocytes in patients <35 years (Table 2); however, there was no significant difference of the FF AMH levels between fertilized and non-fertilized MII oocytes in patients aged ≥35 years (Table 3).
Discussion
Oocyte quality is one of the most important parameter of success in IVF/ICSI procedures. However, morphological quality of oocytes noted during in vitro culture cannot always predict successful fertilization and developmental capacity of oocytes. The role of follicular fluid AMH as indicator of oocyte quality is not yet clarified. By correlating oocyte maturity and morphological quality of MII oocyte noted during ICSI procedure with follicular fluid AMH levels, the present investigation aimed to clarify this question.
Taking into account that female fertility declines with the advancing age of woman and that age-related reproductive failure results from diminished oocyte quality [43], it was decided to subdivide patients into two groups according to age (<35 years and ≥35 years). A negative correlation of serum AMH to female age was found, as described previously [44–46]. Despite data from literature reporting that serum AMH is good predictor of oocyte yield [45, 46], the present study failed to show a correlation between the oocyte yield and serum AMH levels (Table 1). Similar results were also described by Takahashi et al. [31].
This study analyzed percentages of maturity stages of oocytes and percentages of morphological quality of MII oocytes, zygotes, and embryos in patients aged <35 and ≥35 years. Each group consisted of single dominant oocyte of each patient. Percentages of maturity stages of analyzed oocytes and morphological quality of MII oocytes were similar regardless of the patient age and serum AMH level. Percentage of morphological good-quality embryos was significantly higher in patients aged <35 years which support previously published results that the success of IVF mainly depend on maternal age [14, 47].
Some studies demonstrated a clear relationship between serum AMH levels and the quality of oocytes and embryos [15, 16, 19, 21], while others showed a lack of a consistent correlation [22–24, 48]. One recent study suggested an alteration of the follicular metabolism in conventional gonadotrophin stimulated IVF and excluded any relevant impact of AMH serum concentration on the follicular fluid AMH concentration [50]. However, a limited number of studies have analyzed quality of oocyte and embryo with regard to FF AMH levels. The present study revealed no correlation between FF AMH levels and maturity stages of oocytes. Similarly, previous studies described FF AMH concentrations having no effect on embryo quality [28, 29]. In contrast to our results, others showed a negative correlation between FF AMH and oocyte quality [27, 30] and a recent study [28] showed AMH is highly expressed and secreted in preovulatory follicles containing immature and atretic oocytes than in follicles containing MII oocytes. Inconsistency in literature can be result in difference of procedure. The present investigation measured AMH levels in single dominant follicle of each patient while others [27, 30] estimated AMH concentration in pooled follicular fluids. Also, Mehta et al. [30] estimated the maturity of oocyte prior conventional IVF according to cumulus-oophorus radiance which is often difficult to assess. Morphological assessment of MII oocyte prepared for ICSI (without cumulus-oophorus cells), can provide more accurate information about the quality of the MII oocyte. In contrast to previous observations, that different serum AMH levels can predict the morphological quality of an oocyte [15, 16], this study found no relationship between FF AMH levels and morphological quality of MII oocytes.
The present study showed a significant negative correlation between FF AMH levels and fertilization potential of MII oocytes in patients aged <35 years. Fertilized oocytes in this group had significantly lower levels of FF AMH in comparison to non-fertilized oocytes. Higher levels of FF AMH in non-fertilized oocytes suggest that, regardless the same morphological quality of MII oocytes, oocytes from follicles with higher levels of FF AMH had a poor fertilization potential. However, we found no correlation in patients aged ≥35 years. A disadvantage of the present study is its small sample size, which could be a cause of incompatible results in the two patients’ groups. Present results are consistent with the recent study [30] which demonstrated higher percentages of fertilization in low FF AMH group. In contrast to our results, some studies [26, 31] found a positive relationship between FF AMH and fertilization rate. Others found no significant correlation between fertilization rate and serum AMH or FF AMH levels [13, 28, 32]. The inconsistency in literature may in part be explained by sperm quality that can affect fertilization and the application of different fertilization procedures (conventional IVF vs. ICSI). In our study, the ICSI method was used because the IVF method is not optimal for the analysis of oocyte quality. We are aware that ICSI itself can also affect zygote and embryo quality and development, but in the hands of one person, interference of methodology is somehow standardized. Previous study in mice suggests that oocyte can regulate AMH expression and may play a role in intra-follicular regulation of the rate of follicle growth [49]; therefore, we assume that oocytes with good fertilization potential had a good utilization of AMH from follicular fluid.
In conclusion, this study demonstrated that FF AMH levels were significantly lower in fertilized oocytes than in non-fertilized oocytes in patients aged <35 years. It appears that FF AMH levels have no correlation to oocyte maturity stage and morphological quality of MII oocyte but might be a predictive marker of fertilization capacity of MII oocytes in younger patients. Further studies are needed to clarify this hypothesis.
References
Gilchrist RB, Lane M, Thompson JG (2008) Oocyte-secreted factors: regulators of cumulus cell function and oocyte quality. Hum Reprod Update 14(2):159–177
Balaban B, Urman B (2006) Effect of oocyte morphology on embryo development and implantation. Reprod Biomed Online 12(5):608–615
Ubaldi F, Rienzi L (2008) Morphological selection of gametes. Placenta 1(29):115–120
Fortune JE (1994) Ovarian follicular growth and development in mammals. Biol Reprod 50(2):225–232
Revelli A, Delle Piane L, Casano S, Molinari E, Massobrio M, Rinaudo P (2009) Follicular fluide content and oocyte quality: from single biochemical markers to metabolomics. Reprod Biol Endocrinol 7:40
Veeck L (1990) The morphological assessment of human oocytes and early concepts. Handb Lab Diagn Treat Infertil
Ebner T, Yaman C, Moser M, Sommergruber M, Feichtinger O, Tews G (2000) Prognostic value of first polar body morphology on fertilization rate and embryo quality in intracytoplasmic sperm injection. Hum Reprod 15(2):427–430
Xia P (1997) Intracytoplasmic sperm injection: correlation of oocyte grade based on polar body, perivitelline space and cytoplasmic inclusions with fertilization rate and embryo quality. Hum Reprod 12(8):1750–1755
Rienzi L, Vajta G, Ubaldi F (2011) Predictive value of oocyte morphology in human IVF: a systematic review of the literature. Hum Reprod Update 17(1):34–45
Broekmans FJ, Kwee J, Hendriks DJ, Mol BW, Lambalk CB (2006) A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update 12:685–718
Broer SL, Mol BWJ, Hendriks D, Broekmans FJM (2009) The role of antimullerian hormone in prediction of outcome after IVF: comparison with the antral follicle count. Fertil Steril 91(3):705–714
Nelson SM, Yates RW, Fleming R (2007) Serum anti-Müllerian hormone and FSH: prediction of live birth and extremes of response in stimulated cycles—implications for individualization of therapy. Hum Reprod 22(9):2414–2421
Wunder DM, Guibourdenche J, Birkhäuser MH, Bersinger NA (2008) Anti-Müllerian hormone and inhibin B as predictors of pregnancy after treatment by in vitro fertilization/intracytoplasmic sperm injection. Fertil Steril 90(6):2203–2210
Broer SL, van Disseldorp J, Broeze KA, Dolleman M, Opmeer BC, Bossuyt P et al (2013) Added value of ovarian reserve testing on patient characteristics in the prediction of ovarian response and ongoing pregnancy: an individual patient data approach. Hum Reprod Update 19(1):26–36
Ebner T, Sommergruber M, Moser M, Shebl O, Schreier-Lechner E, Tews G (2006) Basal level of anti-Mullerian hormone is associated with oocyte quality in stimulated cycles. Hum Reprod 21:2022–2026
Irez T, Ocal P, Guralp O, Cetin M, Aydogan B, Sahmay S (2011) Different serum anti-Müllerian hormone concentrations are associated with oocyte quality, embryo development parameters and IVF-ICSI outcomes. Arch Gynecol Obstet 284(5):1295–1301
Lekamge DN, Barry M, Kolo M, Lane M, Gilchrist RB, Tremellen KP (2007) Anti-Müllerian hormone as a predictor of IVF outcome. Reprod Biomed Online 14(5):602–610
Majumder K, Gelbaya TA, Laing I, Nardo LG (2010) The use of anti-Mullerian hormone and antral follicle count to predict the potential of oocytes and embryos. Eur J Obstet Gynecol Reprod Biol 150:166–170
Silberstein T, MacLaughlin DT, Shai I, Trimarchi JR, Lambert-Messerlian G, Seifer DB et al (2006) Müllerian inhibiting substance levels at the time of HCG administration in IVF cycles predict both ovarian reserve and embryo morphology. Hum Reprod 21(1):159–163
Lin W-Q, Yao L-N, Zhang D-X, Zhang W, Yang X-J, Yu R (2013) The predictive value of anti-mullerian hormone on embryo quality, blastocyst development, and pregnancy rate following in vitro fertilization-embryo transfer (IVF-ET). J Assist Reprod Genet 30(5):649–655
Sills ES, Collins G, Brady A, Walsh D, Marron K, Peck A et al (2011) Bivariate analysis of basal serum anti-Mullerian hormone measurements and human blastocyst development after IVF. Reprod Biol Endocrinol 9(1):153
Smeenk JMJ, Sweep FCGJ, Zielhuis GA, Kremer JAM, Thomas CMG, Braat DDM (2007) Antimüllerian hormone predicts ovarian responsiveness, but not embryo quality or pregnancy, after in vitro fertilization or intracyoplasmic sperm injection. Fertil Steril 87(1):223–226
Fong SL, Baart E, Martini E, Schipper I, Visser J, Themmen A et al (2008) Anti-Müllerian hormone: a marker for oocyte quantity, oocyte quality and embryo quality? Reprod Biomed Online 16(5):664–670
Guerif F, Lemseffer M, Couet M-L, Gervereau O, Ract V, Royere D (2009) Serum antimullerian hormone is not predictive of oocyte quality in vitro fertilization. Ann Endocrinol 70(4):230–234
Anckaert E, Smitz J, Schiettecatte J, Klein MB, Arce J-C (2012) The value of anti-Mullerian hormone measurement in the long GnRH agonist protocol: association with ovarian response and gonadotrophin dose adjustments. Hum Reprod 27:1829–1839
Aflatoonian A, Mashayekhy M, Mohamadian F, Mansoori Moghaddam F (2010) The correlation between follicular fluid anti-mullerian hormone levels and fertilization and embryo quality in ART cycles. Iran. J Reprod Med 8(4):157–160
Cupisti S, Dittrich R, Mueller A, Strick R, Stiegler E, Binder H et al (2007) Correlations between anti-Mullerian hormone, inhibin B, and activin A in follicular fluid in IVF/ICSI patients for assessing the maturation and developmental potential of oocytes. Eur J Med Res 12:604–608
Fanchin R, Mendez Lozano DH, Frydman N, Gougeon A, di Clemente N, Frydman R et al (2007) Anti-Müllerian hormone concentrations in the follicular fluid of the preovulatory follicle are predictive of the implantation potential of the ensuing embryo obtained by in vitro fertilization. J Clin Endocrinol Metab 92(5):1796–1802
Jančar N, Virant-Klun I, Vrtačnik Bokal E (2009) Serum and follicular endocrine profile is different in modified natural cycles than in cycles stimulated with gonadotropin and gonadotropin-releasing hormone antagonist. Fertil Steril 92(6):3
Mehta B, Chimote M, Chimote N, Nath N, Chimote N (2013) Follicular-fluid anti-Mullerian hormone (FF AMH) is a plausible biochemical indicator of functional viability of oocyte in conventional in vitro fertilization (IVF) cycles. J Hum Reprod Sci 6(2):99–105
Takahashi C, Fujito A, Kazuka M, Sugiyama R, Ito H, Isaka K (2008) Anti-Müllerian hormone substance from follicular fluid is positively associated with success in oocyte fertilization during in vitro fertilization. Fertil Steril 89(3):586–591
Kedem-Dickman A, Maman E, Yung Y, Yerushalmi GM, Hemi R, Hanochi M et al (2012) Anti-Müllerian hormone is highly expressed and secreted from cumulus granulosa cells of stimulated preovulatory immature and atretic oocytes. Reprod Biomed Online 24(5):540–546
Palermo G, Joris H, Devroey P, Van Steirteghem AC (1992) Pregnancies after intracytoplasmic injection of single spermatozoon into an oocyte. Orig Publ 340(8810):17–18
Balaban B, Ata B, Isiklar A, Yakin K, Urman B (2008) Severe cytoplasmic abnormalities of the oocyte decrease cryosurvival and subsequent embryonic development of cryopreserved embryos. Hum Reprod 23(8):1778–1785
Ebner T, Moser M, Sommergruber M, Tews G (2003) Selection based on morphological assessment of oocytes and embryos at different stages of preimplantation development: a review. Hum Reprod Update 9(3):251–262
Rienzi L, Ubaldi FM, Iacobelli M, Minasi MG, Romano S, Ferrero S et al (2008) Significance of metaphase II human oocyte morphology on ICSI outcome. Fertil Steril 90(5):1692–1700
Wilding M, Matteo L, D’Andretti S, Montanaro N, Capobianco C, Dale B (2007) An oocyte score for use in assisted reproduction. J Assist Reprod Genet 24(8):350–358
Scott L, Alvero R, Leondires M, Miller B (2000) The morphology of human pronuclear embryos is positively related to blastocyst development and implantation. Hum Reprod 15(11):2394–2403
Tesarik J, Greco E (1999) The probability of abnormal preimplantation development can be predicted by a single static observation on pronuclear stage morphology. Hum Reprod 14(5):1318–1323
Zollner U, Zollner K-P, Hartl G, Dietl J, Steck T (2002) The use of a detailed zygote score after IVF/ICSI to obtain good quality blastocysts: the German experience. Hum Reprod 17(5):1327–1333
Hardarson T, Hanson C, Sjögren A, Lundin K (2001) Human embryos with unevenly sized blastomeres have lower pregnancy and implantation rates: indications for aneuploidy and multinucleation. Hum Reprod 16(2):313–318
Van Royen E, Mangelschots K, De Neubourg D, Valkenburg M, Van de Meerssche M, Ryckaert G et al (1999) Characterization of a top quality embryo, a step towards single-embryo transfer. Hum Reprod 14(9):2345–2349
Battaglia DE, Goodwin P, Klein NA, Soules MR (1996) Fertilization and early embryology: influence of maternal age on meiotic spindle assembly oocytes from naturally cycling women. Hum Reprod 11(10):2217–2222
Van Rooij IA, Broekmans FJ, Scheffer GJ, Looman CW, Habbema JD, de Jong FH et al (2005) Serum antimullerian hormone levels best reflect the reproductive decline with age in normal women with proven fertility: a longitudinal study. Fertil Steril 83:979–987
La Marca A, Sighinolfi G, Radi D, Argento C, Baraldi E, Artenisio AC et al (2010) Anti-Müllerian hormone (AMH) as a predictive marker in assisted reproductive technology (ART). Hum Reprod Update 16(2):113–130
Broer SL, Mol B, Dólleman M, Fauser BC, Broekmans FJ (2010) The role of anti-Mullerian hormone assessment in assisted reproductive technology outcome. Curr Opin Obstet Gynecol 22(3):193–201
La Marca A, Papaleo E, D’Ippolito G, Grisendi V, Argento C, Volpe A (2011) The ovarian follicular pool and reproductive outcome in women. Gynecol Endocrinol 28(3):166–169
Anckaert E, Smitz J, Schiettecatte J, Klein BM, Arce J-C (2012) The value of anti-Müllerian hormone measurement in the long GnRH agonist protocol: association with ovarian response and gonadotrophin-dose adjustments. Hum Reprod 27(6):1829–1839
Salmon NA, Handyside AH, Joyce IM (2004) Oocyte regulation of anti-Müllerian hormone expression in granulosa cells during ovarian follicle development in mice. Dev Biol 266(1):201–208
von Wolff M, Kollmann Z, Flück CE, Stute P, Marti U, Weiss B, Bersinger NA (2014) Gonadotrophin stimulation for in vitro fertilization significantly alters the hormone mileu in follicular fluid: a comparative study between natural cycle IVF and conventional IVF. Hum Reprod 29(5):1049–1057
Acknowledgments
The authors thank the Department of Histology and Embryology, Rijeka School of Medicine, University of Rijeka for their support during the study. The authors also thank Marina Merkaš for assistance in statistical analysis. This research was funded by the Ministry of Science, Education and Sport of the Republic of Croatia, grant number 62-00000-3553. The funders had no role in study design, collection, analysis, and interpretation of data, writing of the report and decision to submit the article for publication. The authors had no financial relationship with the organization that sponsored the research.
Conflict of interest
The authors declare that they have no conflict of interest. The authors have full control of all primary data and agree to alow the journal to review data if requested.
Ethical standards
The study design was approved by the Ethics Committee of the Clinical Hospital Center Rijeka, and written consent was obtained from all participants prior to their inclusion in the study. The study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. The authors have full control of all primary data and agree to alow the journal to review data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tramišak Milaković, T., Panić Horvat, L., Čavlović, K. et al. Follicular fluid anti-Müllerian hormone: a predictive marker of fertilization capacity of MII oocytes. Arch Gynecol Obstet 291, 681–687 (2015). https://doi.org/10.1007/s00404-014-3460-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-014-3460-9