Abstract
Purpose
To compare the efficacy of clomiphene citrate (CC) and recombinant FSH (rFSH) protocols in ovarian stimulation (OS)/intrauterine insemination (IUI) cycles for couples with unexplained infertility or male subfertility.
Methods
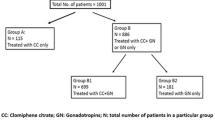
One hundred and eighty-nine patients with unexplained or male subfertility were randomized to treatment with 100 mg/day CC for 5 days (93 patients) or rFSH with starting dose of 75–100 IU daily (96 patients). The main outcome measurement was ongoing pregnancy rate (OPR).
Results
The number of preovulatory (≥17 mm) follicles on the day of hCG administration was significantly greater in the rFSH group than in the CC group (1.7 vs. 1.4, P = .01). Multifollicular growth was observed in 35.1% in the CC group and 54.8% in the FSH group (P = .01). The OPR per cycle was 9.6 and 15.6% for CC and rFSH groups, respectively (P = .31).
Conclusions
Recombinant FSH is superior to CC for enabling multifollicular development in OS/IUI cycles of unexplained and male subfertile couples. Although this finding did not lead to a statistically significant superiority of rFSH in terms of clinical outcomes, the presence of relative increase by 62.5% in OPR with rFSH may be regarded as a clinically significant trend.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intrauterine insemination (IUI) combined with ovarian stimulation (OS) is regarded a simple first line treatment option for couples with unexplained or mild male factor infertility [1–3]. The rationale is to increase the number of gametes available for fertilization in a given cycle. Despite relatively lower pregnancy rates per attempt, cumulative pregnancy rates after three cycles are around 30% in appropriately selected couples [4–6].
An important limitation of OS/IUI is the relatively high risk of multiple pregnancies in case of multifollicular growth. Therefore, it is aimed to limit the number of mature follicles with a maximum of three. Majority of the studies comparing gonadotropin and anti-estrogens used human menopausal gonadotropin [7–9]. Presently available data suggests that gonadotropin is somewhat more effective than oral anti-estrogens [7, 8, 10, 11]. However, higher the cost of gonadotropin and inconvenience of daily injections are a cause of concern. The only randomized controlled trial (RCT) published as full-text comparing rFSH versus CC failed to demonstrate a significant difference in treatment outcomes [12].
The present RCT aimed to compare the effectiveness of CC and rFSH for OS in couples with unexplained infertility and male subfertility undergoing IUI.
Materials and methods
Trial population
Participants were recruited at the infertility clinic of a university-based tertiary care hospital between May 2008 and April 2010. The inclusion criteria were failure to conceive for ≥24 months of unprotected intercourse, female age <38 years, basal (day 3) FSH levels <12 IU/l, and a diagnosis of unexplained or mild-moderate male factor infertility. Exclusion criteria were as follows; ovarian cysts larger than 15 mm on baseline transvaginal ultrasound, severe endometriosis (according to the revised American Fertility Society stage III and IV), the total number of inseminated motile sperm being <1.0 × 106, or contraindications for one of the ovarian stimulation drugs. Each woman were only included with one treatment cycle. All couples had a standard infertility evaluation that included a medical history, physical examination, assessment of tubal patency either by hysterosalpingography or laparoscopy, confirmation of an ovulatory cycle by mid-luteal serum progesterone, and a semen analysis (abnormal results confirmed by a second analysis at least 6 weeks apart). Semen samples with a concentration of >20 million/mL, type A + type B motility >50% and normal morphology >14% were considered normal [13, 14]. Couples with normal sperm parameters, bilateral patent Fallopian tubes and regular ovulatory cycles between 21 and 35 days were diagnosed with unexplained infertility. Mild-male factor infertility was defined with a semen analysis result failing to meet above mentioned reference criteria but having a total motile sperm count of >5 million.
Sample size calculation
While planning the present study, we were able to detect two studies [12, 15] in the literature that could guide us in terms of prestudy power analysis and we chose the study that included a larger patient population with increased number of cycles [12]. On the basis of that study, when a power analysis was performed with 80% power and an α-value of 0.05 for an approximately 1.4% difference in live birth rate per cycle, patient number for each study arm should be 6,746 for the confirmation of statistical significance. Thus, in the present study type II statistical error could not be excluded for this parameter. Considering the difficulty of recruiting so many participants to a single center trial, the current trial aimed was to be finished in 2 years with 200 participants, which could be included in future meta-analyses on the issue.
Randomization
Randomization was performed according to a randomly computer-generated number list by an independent investigator. Participants were randomized to one of the two OS protocols using either CC (Klomen®; Kocak Farma, Istanbul, Turkey) or rFSH; follitropin beta (Puregon®; Schering-Plough, Istanbul, Turkey) at a ratio of 1:1. From the randomization list, an independent secretary prepared and sealed the numbered and opaque envelopes. The envelopes were opened in consecutive order by one of the investigators after verbal and written consent, after the ultrasound exam which was performed on cycle day 2–3, and before starting the treatment protocol. The treatment group sizes were not disclosed during the study. All of the spare envelopes were unopened at the end of the study.
Interventions
A transvaginal ultrasound exam was performed on cyle day 2 or 3. Women with ovarian cysts ≥15 mm were excluded. Women assigned to CC received CC 100 mg/daily orally for five consecutive days starting from cycle days 2–4. Ovarian monitoring was carried out by vaginal ultrasound and estradiol monitoring, starting on day 8 of the menstrual cycle. Women allocated to rFSH were stratified according to body mass index (BMI). Starting rFSH dosage was 75 IU/day for women with a BMI <25 kg/m2 and 100 IU/day for women with BMI ≥25 kg/m2. rFSH injections were commenced on cycle day 2–4. The first monitoring scan was done on the 6th day of gonadotropin stimulation, and repeated after 2 or 3 days, depending on the follicular growth. If at least one of the follicle’s diameters was not >10 mm at the 8th and 9th day of stimulation, the dose of gonadotropin was increased by 50%. The gonadotropin dose remained the same until the day of hCG after the leading follicle reached to 12 mm in diameter. hCG (Pregnyl®, Schering-Plough, Istanbul, Turkey) 10,000 IU was administered when the leading follicle reached ≥18 mm in both groups.
Multifollicular growth was defined as at least two dominant follicles reaching minimum 17 mm in diameter, hCG injection was not given if there were >3 follicles ≥17 mm, or >5 follicles ≥14 mm to reduce the risk of multiple pregnancy and/or ovarian hyperstimulation.
A single IUI was performed 36–40 h after hCG injection. Semen samples used for insemination were processed within 1 hour after ejaculation, using a density gradient centrifugation followed by washing with culture medium. Women had bed rest for 15–20 min after the IUI. No luteal phase support was given.
Outcome measures
The primary outcome measure was ongoing pregnancy rate (OPR). The secondary outcome measures were multiple pregnancy rate, number of preovulatory follicles, endometrial thickness on the day of hCG administration, miscarriage, and ovarian hyperstimulation rates.
Pregnancy was determined as positive by β-hCG levels after 12–14 days from the insemination procedure. Ongoing pregnancy is defined as pregnancy proceeding beyond 20 weeks of gestation. Miscarriage was defined as pregnancy loss before 20 weeks.
The study was performed under the rules of the Declaration of Helsinki, and approved by the Institutional Review Board of the University. Standard written informed consent for OS/IUI was obtained from all patients before entering the study.
Statistical considerations
SigmaStat for Windows, version 3.1 (Jandel Scientific Corporation, San Rafael, CA) was used for statistical analysis. Continuous variables were compared with student’s t test or Mann–Whitney U test according to distribution of each variable. Categorical variables were compared with Chi square test or Fisher’s exact test where appropriate. A P value of <0.05 was considered statistically significant.
Results
One hundred and eighty-nine couples diagnosed with unexplained infertility and mild male subfertility were recruited. Demographic and baseline variables are presented in Table 1. There were no significant differences in terms of mean age of male or female, body mass index (BMI), serum FSH and E2 levels on the 3rd day of the spontaneous cycle, total progressive motile (type A and B) sperm count in male factor infertility, number of previous OS/IUI cycle, and duration of infertility. The distribution of patients with primary infertility, unexplained infertility, and male factor infertility was similar in both groups. The cycle characteristics of the study groups are shown in Table 2. The number of preovulatory (≥17 mm) follicles were significantly greater in rFSH group than that in the CC group (1.7 vs. 1.4, respectively, P = .01). Multifollicular growth occurred in 35.1% (32/91) and 54.8% (51/93) of women in CC and rFSH groups, respectively (P = .01). Cycle duration and endometrial thickness on the day of hCG were not significantly different between the two groups.
The treatment outcomes are shown in Table 3. In the CC group, two cycles (2.1%) were cancelled. Both were cancelled due to poor ovarian response. In the rFSH group, three (3.1%) cycles were cancelled: two due to high ovarian response; one of these patients had five follicles ≥17 mm, and the other had seven follicles ≥14 mm, and one due to poor ovarian response. The ongoing pregnancy rate was 9.6% (9/93) and 15.6% (15/96) in CC and rFSH groups, respectively. However, the difference was not statistically significant (P = .31). The overall miscarriage rate was 14.2% (4/28). Of these, 2 (18.1%) occurred in the CC and 2 (11.7%) in the rFSH group (P = .62). Two (13.3%) twin pregnancies occurred in the rFSH group. There was one case of mild OHSS in the rFSH group.
The OPR were similar when couples with unexplained infertility (18.0% (9/50) in rFSH and 11.6% (5/43) in CC and male subfertility group (13.0% (6/46) and 8% (4/50) in rFSH and CC groups, respectively (P = .51)) were compared separately.
Cycles with monofollicular and multifollicular growth were analyzed separately (Fig. 1). The OPRs were 9.9% (10/101) in monofollicular group and 16.8% (14/83) in multifollicular group (P = .23). The OPR in monofollicular and multifollicular cycles of the CC group were 8.4% (5/59) and 12.5% (4/32), respectively, and this difference was not statistically significant (P = .71). In the rFSH group, these rates were 11.9% (5/42) and 19.6% (10/51) for monofollicular versus multifollicular, respectively and this difference was not statistically significant (P = .47).
Discussion
The results obtained from this study indicate comparable pregnancy rates for rFSH and CC in OS/IUI cycles. This observation is generally consistent with those of Dankert et al. [12], in which there is only one RCT published as full-text comparing the CC protocol with the rFSH protocol in couples with unexplained infertility or male subfertility in the literature. In this study, the OPR per cycle for couples with unexplained subfertility was 12.2% in the CC group and 9.8% in the rFSH group. For male subfertility, these rates were 8.3 and 7.6% for CC versus rFSH, respectively. On the contrary, in the present study, the OPRs in the rFSH group, tend to be higher although not statistically significant. The main methodological difference between Dankert’s study and our study is that in their study, they included up to four cycles of the same patient if pregnancy did not occur. Therefore, in Dankert’s study, cumulative pregnancy and live birth rates could be given as the primary outcome. On the other hand, in the present study, we randomized only one cycle of each patient to one of the treatment groups.
In the present study it was observed that the number of mean preovulatory follicles and cycles with multifollicular growth were significantly higher in the rFSH group, when compared with the CC group. However, there was an increased follicular growth in the rFSH group, which did not result in an obvious benefit for the pregnancy rate. The fact that this positive situation in favor of the rFSH in the cycle parameters was not reflected on the pregnancy outcomes and this might have been caused by the fact that the power of the study was insufficient for pregnancy outcomes. Indeed, a recent analysis revealed that the “ideal” OS regimen, together with sufficient amount of E2, should be able to enable the development of two preovulatory (>16 mm) follicles. In this study which includes 1038 IUI cycles, while OPR per cycle was 9.8% in monofollicular cycles, this rate was 14.5% in the cycles where two follicles developed and this rate was found statistically significant [16]. However, one of the concerns about the cycles showing multifollicular development is the increase in the rates of multiple pregnancies and it is known that this situation is apparently higher, especially in the presence of 3 or more preovulatory follicles [16]. In the present study, multiple pregnancies were observed only in two patients and both of them were in the rFSH group.
In a meta-analysis, ovarian stimulation in combination with IUI for unexplained infertility was shown to result significantly higher in pregnancy rates per woman when compared with IUI in the natural cycle [2]. On the other hand, the treatment results of OS/IUI for male subfertility could not reveal a clear superiority over the natural cycle IUI [3]. Despite this uncertainty, OS/IUI is a widely preferred treatment modality today in male subfertility treatment as it is in the treatment of unexplained infertility. However, there is still a dispute about which drug should be the first choice for ovarian hyperstimulation. Many studies have compared different forms of ovarian stimulation. Particularly in the studies that were published in the 1990 s, gonadotropins were compared with CC, which had been the most frequently preferred agent in OS/IUI cycles until that period. Karlstrom et al. showed that for couples with unexplained subfertility, a statistically nonsignificant difference in pregnancy rates in HMG-stimulated IUI cycles (20%), when compared with CC-stimulated IUI cycles (6%) [7]. Also, Hannoun et al. [8] reported that IUI cycles with hMG stimulation showed slightly higher but not significant pregnancy rates than cycles stimulated with CC. Ecochard et al. [9] concluded that CC was an effective alternative to hMG for initial attempts at IUI in unselected patients during the first four cycles of therapy. Balasch et al. [10] described a significantly higher pregnancy rate in IUI cycles with late low dose purified FSH (13%) compared to stimulation by CC (4%), in couples with male or unexplained subfertility. Also, Matorras et al., in IUI cycles with donor sperm, highly purified FSH stimulated cycles showed statistically significant higher pregnancy rates than CC stimulated cycles. Pregnancy rates per started cycle were 6.1% in the CC group and 12.6% in the FSH group. Cumulative PR was 31.4% and 61.2% in the CC and FSH groups, respectively [11]. When the results of the above mentioned studies are evaluated generally, the gonadotropin regimens seem to be more successful protocols, when compared to CC regimens in IUI cycles. However, a systematic review of five randomized controlled trials compared CC and gonadotropin for stimulated IUI in couples with unexplained fertility and found no significant difference in live birth rates per couple although the pregnancy rate seemed to be higher with gonadotropin [17]. A more recent systematic review of seven studies comparing gonadotropin with anti-estrogens (CC) in couples with subfertility showing significant higher pregnancy rates with gonadotropin [18].
Another controversial issue regarding the OS regimes used in IUI cycles is whether or not different gonadotropin regimes have any superiority over each other. All the FSH preparations which had been used until the second half of the 1990s were produced from postmenopausal urine extracts and after this date, FSH preparations produced with recombinant technology came into use [19]. It was suggested that rFSH preparations would have some advantages in ovulation induction, when compared with the urinary products [20]. However, in a systematic review including small RCTs, the clear superiority of rFSH over the other gonadotropin (uFSH or hMG) and CC has not been proven in terms of pregnancy rates in gonadotropin-combined IUI cycles of subfertile couples [18]. In contrast to this result, Demirol et al. [21], in a RCT included 241 cycles of 241 patients, compared the effectiveness of different gonadotropin preparations in IUI cycles for patients with unexplained infertility and reported that the clinical pregnancy rate was significantly higher in the rFSH group (25.9%), when compared with uFSH (13.8%) and HMG (12.5%) groups.
One of the main drawbacks of our study is the limited number of patients. While we were planning our study, the pregnancy rates which we used as samples for the power analysis were the OPRs per cycle obtained from Dankert’s study [12]. According to this data, we estimated that 6,746 patients were required in each treatment arm so that approximately 1.4% difference between the two treatment groups could be statistically significant. It was not realistic to expect to have this number of patients or cycles in a prospective randomized study carried out in a single centre. On the other hand, even if we tried to increase this number by including all the repeated IUI cycles of the patients in the study, it was rather difficult to reach this number of cycles. Therefore, we started the study by aiming to reach nearly 200 cycles in total. The results of our study revealed that overall OPR per cycle was 6% higher in the rFSH group but the difference was not statistically significant. Owing to the possibility of beta error, it is unclear whether this finding is due to the genuine lack of any superiority rFSH on CC in clinical efficacy or the lack of statistical power to detect a statistically significant difference. In order to determine whether or not the difference in OPR carried statistical significance, new further studies should include at least 479 patients or cycles in each treatment arm.
In a meta-analysis published in 2002, five prospective randomized studies comparing CC and different gonadotropin regimes were included [17]. In this meta-analysis, there is only one study comparing rFSH and CC [12]. Unfortunately, this study was published as an abstract only and was carried out with a limited number of cycles (40 cycles in total). In this study, it was stated that an equal number of (four) pregnancies were obtained in both treatment arms. As a result, the authors emphasized that since the patient population in their series was small, it was necessary to compare these two protocols in studies with a larger patient population in order to reveal the optimal OS regime to be used in IUI cycles applied for such group of patients. The fact that only one study [12] comparing these two protocols was published throughout the time after the publishing of the abstract of this study reveals apparently that the literature still lacks such studies. Therefore, we expect that the results obtained from the present study would both shed a light on the future studies and contribute to the literature in terms of providing data for further meta-analyses to be carried out.
In conclusion, rFSH is superior to CC for enabling multifollicular development in OS/IUI cycles of unexplained and male subfertile couples. In the present study, although this finding did not lead to a significant superiority of rFSH in terms of pregnancy rates, further prospective randomized trials with larger numbers of patients/cycles and large meta-analyses are needed in order to confirm the possible positive correlation of this potential advantage with clinical outcomes.
References
Duran HE, Morshedi M, Kruger T, Oehninger S (2002) Intrauterine insemination: a systematic review on determinants of success. Hum Reprod Update 8:373–384
Verhulst SM, Cohlen BJ, Hughes E, Te Velde E, Heineman MJ (2006) Intra-uterine insemination for unexplained infertility. Cochrane Database Syst Rev 18:CD001838
Bensdorp A, Cohlen BJ, HeinemanMJ, Vanderkerchove P (2007) Intra-uterine insemination for male subfertility. Cochrane Database Syst Rev 4:CD000360
Vitthala S, Gelbaya TA, Hunter H, Roberts SA, Nardo LG (2008) Stimulated intrauterine insemination (SIUI) and donor insemination (DI) as first line management for a selected subfertile population: the Manchester experience. J Assist Reprod Genet 25:431–436
Bensdorp AJ, Slappendel E, Koks C et al (2009) The INeS study: prevention of multiple pregnancies: a randomised controlled trial comparing IUI COH versus IVF e SET versus MNC IVF in couples with unexplained or mild male subfertility. BMC Womens Health 9:35
Farhi J, Orvieto R (2010) Cumulative clinical pregnancy rates after COH and IUI in subfertile couples. Gynecol Endocrinol 26:500–504
Karlstrom PO, Bergh T, Lundkvist O (1993) A prospective randomized trial of artificial insemination versus intercourse in cycles stimulated with human menopausal gonadotropin or clomiphene citrate. Fertil Steril 59:554–559
Hannoun A, Abu-Musa A, Kaspar H, Khalil A (1998) Intrauterine insemination IUI: the effect of ovarian stimulation and infertility diagnosis on pregnancy outcome. Clin Exp Obstet Gynecol 25:144–146
Ecochard R, Mathieu C, Royere D, Blache G, Rabilloud M, Czyba JC (2000) A randomized prospective study comparing pregnancy rates after clomiphene citrate and human menopausal gonadotropin before intrauterine insemination. Fertil Steril 73:90–93
Balasch J, Ballesca JL, Pimentel C, Creus M, Fabregues F, Vanrell JA (1994) Late low-dose pure follicle stimulating hormone for ovarian stimulation in intra-uterine insemination cycles. Hum Reprod 9:1863–1866
Matorras R, Diaz T, Corcostegui B, Ramon O, Pijoan JI, Rodriguez-Escudero FJ (2002) Ovarian stimulation in intrauterine insemination with donor sperm: a randomized study comparing clomiphene citrate in fixed protocol versus highly purified urinary FSH. Hum Reprod 17:2107–2111
Dankert T, Kremer JA, Cohlen BJ et al (2007) A randomized clinical trial of clomiphene citrate versus low dose recombinant FSH for ovarian hyperstimulation in intrauterine insemination cycles for unexplained and male subfertility. Hum Reprod 22:792–797
World Health Organization (1999) Laboratory manual for the examination of human semen and semen-cervical mucus interaction, 4th edn. Cambridge University Press, Cambridge
Kruger TF, Acosta AA, Simmons KF, Swanson RJ, Matta JF, Oehninger S (1998) Predictive value of abnormal sperm morphology in in vitro fertilization. Fertil Steril 49:112–117
Nakajima AK, Smith LL, Wong B et al (1999) A randomized trial of CC plus IUI versus rFSH plus IUI for the treatment of subfertility. Fertil Steril (Suppl) 72:208
Merviel P, Heraud MH, Grenier N, Lourdel E, Sanguinet P, Copin H (2010) Predictive factors for pregnancy after intrauterine insemination (IUI): an analysis of 1038 cycles and a review of literature. Fertil Steril 93:79–88
Athaullah N, Proctor M, Johnson NP (2002) Oral versus injectable ovulation induction agents for unexplained subfertility. Cochrane Database Syst Rev 3:CD003052
Cantineau AEP, Cohlen BJ (2007) Ovarian stimulation protocols (anti-oestrogens, gonadotrophins with and without GnRH agonists/antagonists) for intrauterine insemination (IUI) in women with subfertility. Cochrane Database Syst Rev 2:CD005356
Howles CM (1996) Genetic engineering of human FSH (Gonal-F). Hum Reprod Update 2:172–191
Out HJ, Mannaerts BM, Driessen SG, Coelingh Benningk HJ (1996) Recombinant follicle stimulating hormone (rFSH; Puregon) in assisted reproduction: more oocytes, more pregnancies: results from five comparative studies. Hum Reprod Update 2:162–171
Demirol A, Gurgan T (2007) Comparison of different gonadotrophin preparations in intrauterine insemination cycles for the treatment of unexplained infertility: a prospective, randomized study. Hum Reprod 22:97–100
Acknowledgments
The authors thank İçten Kıvançlı, M.D., for helping collection of data and Barış Ata, M.D., for his suggestions and critical reading of the manuscript.
Conflict of interest
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Berker, B., Kahraman, K., Taskin, S. et al. Recombinant FSH versus clomiphene citrate for ovarian stimulation in couples with unexplained infertility and male subfertility undergoing intrauterine insemination: a randomized trial. Arch Gynecol Obstet 284, 1561–1566 (2011). https://doi.org/10.1007/s00404-011-1997-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-011-1997-4