Abstract
Purpose
Isolated tumor cells (ITC) in the bone marrow of breast cancer patients increase the risk of recurrence and decrease survival, both at primary diagnosis and during follow-up. We tested the efficacy of trastuzumab in clearing HER2/neu-positive ITC from the marrow of patients completing primary treatment.
Methods
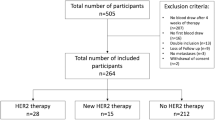
Ten recurrence-free patients with persistent HER2/neu-positive ITC after routine adjuvant treatment received trastuzumab 6 mg/kg q3w for 12 months in a non-randomized pilot phase II interventional study. Bone marrow ITC HER2/neu status was evaluated at baseline, after treatment for 3, 6 and 12 months, and yearly thereafter, in combination with clinical follow-up. Median follow-up was 23 (15–64) months after baseline bone marrow aspiration.
Results
Trastuzumab for 12 months eradicated HER2/neu-positive ITC from bone marrow in all patients (P = 0.002) and significantly reduced the number of ITC-positive patients (P = 0.031). However, HER2/neu-negative ITC persisted in three patients immediately after treatment and were detected at yearly bone marrow aspiration in five patients. Two patients with ITC counts ≥5 at yearly follow-up developed metastases and one died.
Conclusion
This is the first evidence that trastuzumab is effective in clearing HER2/neu-positive cells from bone marrow during recurrence-free follow-up in breast cancer patients. It also suggests, thanks to the antigen shift phenomenon, an important prognostic role for HER2/neu expression on marrow ITC as a real-time biopsy. However, treatment was mainly effective in patients with HER2/neu-positive ITC. Given the heterogeneity of minimal residual disease, these patients might benefit from a combination of targeted treatment approaches.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Isolated tumor cells (ITC) in bone marrow have recently been shown to be associated with reduced disease-free and overall survival in breast cancer patients at both primary diagnosis—pooled analysis of 4,703 patients [1]—and recurrence-free follow-up of primary local and systemic treatment [2]. ITC can thus be used to select patients at increased risk for relapse likely to benefit from additional treatment intervention.
Several authors have shown an antigen shift from the primary tumor to distant metastases [3–5]. Discordance in the therapeutically relevant HER2/neu receptor was observed in 10–20% of metastases, leading to a change of treatment in these patients. This observation prompted the recommendation to evaluate metastatic tissue where possible. Early disease stages show a high rate of concordance between the HER2/neu status of the primary tumor and that of ITC in blood and bone marrow [6], while HER2/neu amplification seems to become more frequent in systemic progression [7–9]. ITC detection can, thus, serve as a real-time biopsy and might provide more accurate phenotyping than the primary tumor, especially during follow-up or in patients with inaccessible metastases.
Therapies informed by ITC phenotyping could provide a more individualized, risk-specific approach to improving prognosis in patients with persistent ITC after standard adjuvant treatment. The humanized monoclonal antibody trastuzumab is an effective treatment of HER2/neu-positive primary breast cancer, achieving an absolute disease-free survival benefit of 12% [10]. In the current study, we investigated the therapeutic efficacy of trastuzumab against persistent ITC in bone marrow, irrespective of the HER2/neu status of the primary tumor.
Patients and methods
Study design and patients
This non-randomized phase II trial evaluated the efficacy of trastuzumab 6 mg/kg q3w × 12 months (8 mg/kg loading dose) in eliminating HER2/neu-positive ITC from bone marrow in women with primary breast cancer during recurrence-free follow-up. Bone marrow was retested at 3, 6 and 12 months and yearly intervals thereafter up to 36 months. Endpoints were the elimination of ITC from bone marrow, reduction in the ITC count, and change ITC HER2/neu status.
Eligible patients had histologically confirmed, completely excised primary breast cancer pT1-4 pN0-3 pM0 with evidence of at least one persistent HER2/neu-positive ITC in their bone marrow at least 6 months after completion of surgery and adjuvant chemotherapy, where indicated. Patients were required to have adequate cardiac function demonstrated by electrocardiography and ultrasonic cardiography (left ventricular ejection fraction ≥55% lower limit of normal) and to give written informed consent before inclusion. Patients previously treated with trastuzumab were ineligible. Adjuvant tamoxifen or an aromatase inhibitor was the only permitted concomitant antitumor treatment. The study protocol was approved by the institutional review board of Ludwig-Maximilians University, Munich.
Primary surgical and systemic treatment complied with national and international guidelines at diagnosis in all patients. The primary surgical treatment was either breast conservation (n = 8), or modified radical mastectomy (n = 2) leading to R0 resection in all reported cases. Routine axillary dissection included level I and II lymph nodes (n = 8). Since 2003, routine sentinel lymph node biopsy was only supplemented by axillary dissection if positive. Six patients received anthracycline and taxane-based chemotherapy, if indicated by the St. Gallen guidelines. Four patients did not qualify for adjuvant chemotherapy due to their low-risk profile at the time of diagnosis. Five patients were treated with six sequential courses of FEC, epirubicin (120 mg/m2), 5-fluorouracil (1,000 mg/m2) and cyclophosphamide (75 mg/m2 p.o. days 1–14) every 28 days, while one patient received EC-Doc, four courses of epirubicin (90 mg/m2) and cyclophosphamide (600 mg/m2) followed by four cycles of docetaxel (100 mg/m2) every 21 days. Radiotherapy was administered to all patients treated with breast conservation and one patient following mastectomy. Patients with hormone receptor-positive disease received endocrine therapy with tamoxifen or an aromatase inhibitor, if indicated.
Detection of ITC in bone marrow
Bone marrow was tested using our unmodified published protocol [11, 12]. In summary, two bone marrow samples (3–8 ml each) were collected in EDTA-treated tubes. After centrifugation on a Ficoll-Hypaque (Pharmacia, Germany) density gradient, mononucleated interface cells were washed, and 106 cells were centrifuged onto glass slides at 150 g for 5 min. Monoclonal antibody A45-B/B3 (Micromet, Germany), directed against the cytokeratin (CK) heterodimers 8/18 and 8/19 [13], was used to detect tumor cells in the cytospin preparation. Isotype control was achieved using an appropriate dilution of unrelated mouse-myeloma antibody (Sigma, Deisenhofen, Germany) on patients’ bone marrow samples. The specific reaction of the primary antibody was developed with the alkaline phosphatase anti-alkaline phosphatase technique and stained with new fuchsin. Breast cancer cell line BT-20 served as a positive control for CK immunostaining [14]. An appropriate dilution of unrelated mouse-myeloma antibodies was used as an IgG1 isotype staining control on patient samples (MOPC21, Sigma). Those giving inconclusive results were excluded from the analysis.
HER2/neu status was determined by chromogenic in situ hybridization in all slides with CK-positive cells. After permeabilization and fixation cells were denatured at 68°C in formamide solution. HER2/neu kits (Zymed Germany) were used for hybridization and detection. Patients with at least one CK-positive cell and more than two HER2/neu signals were regarded as HER2/neu-positive.
A semi-automated screening system (MDS, Applied Biosystems, GB) was used to screen 2 × 106 bone marrow cells per patient. All slides were examined by two independent observers (>95% concordance). In addition, a group of 203 patients with benign disease was used as a methodological control [15].
Follow-up
Patients attended our oncology outpatient department as clinically necessary. Follow-up included clinical examination at each visit and 6-monthly mammography. Blood tests, chest radiography, liver ultrasonography, bone scan and computed tomography of the appropriate region were performed as indicated by tumor signs and/or symptoms. If patients sought care elsewhere, data were collected from the family physicians or gynecologists in charge. The median observation time after primary diagnosis was 41 months (range 29–136 months).
Statistical analysis
Data quality was controlled by reviewing the original data files to verify all event reports during follow-up. The McNemar test was used to compare categorical variables, and the Wilcoxon test to calculate differences between samples with continuous variables. P values below 0.05 were considered significant in two-sided tests. All tests were conducted using Statistical Package for Social Sciences 17.0 (SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics
Median age at primary diagnosis was 58 years (range 39–69). Most patients had T1 tumors (70%) and 40% were node-negative. Tumors tended to be hormone receptor-positive (70%), but histopathological grading was unfavorable in 90% (Table 1). While patients were required to have evidence of HER2/neu-positive ITC in their bone marrow, primary tumor HER2/neu status was negative in six cases by both immunohistochemistry (IHC) and fluorescent in situ hybridization (FISH). Retrospective FISH analysis showed discordant results in one patient with poor tissue quality and 3+ IHC staining but no gene amplification. One case was diagnosed as chromosome-17 monosomy and one as polysomy: both were counted as HER2/neu-negative. None of the HER/neu positive patients had received adjuvant trastuzumab.
All patients had completed primary surgical and chemotherapy treatment, if indicated (n = 6), at least 6 months previously. Cotreatments during and/or after trastuzumab were tamoxifen 20 mg/day (n = 5), a gonadotropin-releasing hormone analog (n = 1), and an aromatase inhibitor (n = 1). Overall, trastuzumab was well tolerated with no toxicity of note. One patient discontinued treatment prematurely after 8 months due to visual impairment, which improved thereafter.
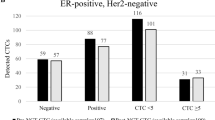
ITC in bone marrow before and after trastuzumab treatment
Bone marrow aspiration was performed at baseline 12.2 (6.6–120.8) months after primary diagnosis and repeated at 3, 6 and 12 months and at yearly intervals thereafter for 23 (15–64) months after study entry. At baseline aspiration, the median CK+ cell count was 2 (range 1–10) with 1 HER2/neu-positive cell (range 1–4). Trastuzumab treatment for 12 months completely eliminated HER2/neu-positive ITC from the bone marrow of all patients (P = 0.002, McNemar) and significantly reduced the number of ITC-positive (CK+) patients (P = 0.031, McNemar) (Figs. 1, 2). However, HER2/neu-negative ITC persisted in three patients immediately after treatment (median 0 ITC, range 0–4) (Table 2).
ITC in bone marrow after completion of trastuzumab treatment and clinical follow-up
Median follow-up after completing trastuzumab therapy was 41 (29–136) months after primary diagnosis and 23 (15–64) months after baseline bone marrow aspiration. The median number of yearly follow-up aspirations was 1 (range 1–3; n = 8). Although one patient showed persistently negative bone marrow status, ITC were detected at least once in seven patients after completing trastuzumab treatment: HER2/neu-negative ITC in five patients, HER2/neu-positive ITC in one patient, and indeterminate ITC HER2/neu status in the remaining patient. Two patients with ITC counts ≥5 during follow-up developed metastases while all other patients had ITC levels <5. One patient with a baseline ITC count of 10 and complete clearance from her bone marrow while on trastuzumab showed an increase in her post-treatment count to 58: she was diagnosed with distant metastases 13 months after completing trastuzumab and died 6 weeks later.
Discussion
This pilot study showed that trastuzumab is markedly effective in clearing HER2/neu-positive cells from bone marrow during recurrence-free follow-up. Patients at risk of relapse were selected on the basis of persistent ITC and received 12 months of trastuzumab treatment. The main treatment effect was the complete elimination of HER2/neu-positive ITC, with HER2/neu-negative ITC persisting in a substantial number of patients.
Pooled analyses have confirmed the prognostic significance of bone marrow ITC, whether at primary diagnosis [1] or during follow-up [2], regardless of established prognostic factors. Pooled analysis of 4,703 patients with primary breast cancer showed that the presence of ITC was a significant prognostic parameter for poor overall and disease-free survival during the entire 10-year observation period (P < 0.001) [1]. Three independent European groups collected bone marrow aspirates during recurrence-free follow-up at a mean interval of 31.7 ± 19.4 months after primary diagnosis of breast cancer and followed the patients for a median of 54.5 ± 25.1 months. Persistent ITC were detected in 15.4% of patients during recurrence-free follow-up and were associated with significantly shorter disease-free and overall survival (P < 0.0001 for both parameters) [2]. Our study, therefore, used the detection of bone marrow ITC evading primary local and systemic treatment to select patients at increased risk of relapse who might benefit from additional treatment approaches.
Beyond prognostic relevance, phenotyping of ITC can reveal targets for individualized treatment approaches. Differences in HER2/neu expression between primary tumor and distant metastases have been described in 10–20% of patients [3–5]. Two hypotheses have been advanced in explanation: either HER2/neu amplification is acquired during dissemination and disease progression [16], or HER2/neu-positive clones of the primary tumor have a greater tendency to break away to form metastases. [8, 9, 17–20] Although positive HER2/neu status predicts the presence of ITC in blood [16], HER2/neu-positive ITC are frequently detected in the bone marrow and blood of patients with HER2/neu-negative primary tumors [8, 9, 18–21]. In our study, we found HER2/neu-positive ITC in 60% of patients with HER2/neu-negative primary tumors. Thus, ITC might represent a more relevant disease phenotype than the primary tumor, especially during follow-up or in patients with inaccessible metastases.
The few trials on systemic treatments in ITC-positive patients are mainly small. Cytostatic treatment had no significant effect [22], possibly due to the low expression of proliferation markers, suggesting that the cells were dormant [23, 24]. Cell-cycle-independent agents directed against specific ITC characteristics might therefore be more promising. Bisphosphonates clear ITC from bone marrow in about 80% of patients [21, 25]. This finding parallels the recently observed prolongation of survival in early breast cancer patients [26–28].
Regarding targeted treatment approaches after phenotyping ITC, three non-randomized phase II trials targeting treatment to ITC phenotype showed significant tumor cell elimination in patients receiving the monoclonal antibody 17-1A (edrecolomab) directed against EpCAM [29–31]. HER2/neu overexpression or amplification is associated with more aggressive tumor behavior and resistance to endocrine and cytostatic treatment, yet agents such as trastuzumab directed against HER2/neu have proved highly effective in both early and metastatic disease with only minor side effects [10, 32, 33]. Trastuzumab could prove similarly effective in patients with HER2/neu-positive residual disease.
Our study used ITC both as a therapeutic target, after defining the cells’ HER2/neu status, and an early marker of treatment response. Trastuzumab completely eliminated HER2/neu-positive ITC during treatment, although 30% of patients continued to show HER2/neu-negative ITC. This confirms that trastuzumab is effective in eliminating HER2/neu-positive disease, but also suggests that a purely HER2/neu-based strategy has limited efficacy against the heterogeneity of minimal residual disease. Our data confirm earlier reports of CK-19 mRNA elimination in 93% of patients treated with trastuzumab [34], and are also consistent with the clinical response reported in three out of four initially HER2/neu-negative patients with metastatic breast cancer receiving trastuzumab for HER2/neu-positive ITC in blood [9].
In contrast to other studies, we performed preplanned yearly follow-up aspiration for a median 23 months. Five out of eight patients showed HER2/neu-negative ITC after completing trastuzumab therapy; only one showed HER2/neu-positive ITC, followed shortly afterwards by distant metastases. In such cases ITC might reflect occult tumor burden, which is inhibited but not totally eliminated by trastuzumab. Persistent HER2/neu-negative ITC might reflect heterogeneity in minimal residual disease, in which case patients could benefit from a combination of targeted treatment approaches.
While our study suggests clinical efficacy of targeted agents on the elimination of minimal residual disease, our approach has several shortcomings. The rather low sensitivity of presently available techniques for the detection of ITC in bone marrow and blood limits the number of patients available for clinical trials, especially during recurrence-free follow-up. Taking into account the low sample size, the inhomogeneity of systemic treatment at primary diagnosis and the non-randomized design, results should be interpreted with appropriate caution. However, the results of this study can be used as hypothesis generating basis pointing out the need of randomized clinical trials.
Persistent bone marrow ITC predict an increased risk of relapse and reduced survival. ITC phenotyping can be used to tailor more individualized treatment approaches for patients with no evidence of disease during follow-up as well as for those with metastatic breast cancer. We have shown that trastuzumab is highly effective against HER2/neu-positive ITC. A combination of targeted treatment options might further improve outcome in these patients.
Ethical approval This study was approved by the ethical committee of the Ludwig-Maximilians-University.
References
Braun S, Vogl FD, Naume B, Janni W, Osborne MP, Coombes RC, Schlimok G, Diel IJ, Gerber B, Gebauer G, Pierga JY, Marth C, Oruzio D, Wiedswang G, Solomayer EF, Kundt G, Strobl B, Fehm T, Wong GY, Bliss J, Vincent-Salomon A, Pantel K (2005) A pooled analysis of bone marrow micrometastasis in breast cancer. N Engl J Med 353:793–802
Janni W, Vogl FD, Wiedswang G, Synnestvedt M, Fehm T, Jückstock J, Borgen E, Rack B, Braun S, Sommer H, Solomayer E, Pantel K, Nesland J, Friese K, Naume B (2011) Persistence of disseminated tumor cells in the bone marrow of breast cancer patients predicts increased risk for relapse—a European pooled analysis. Clin Cancer Res 17(9):2967–2976
Simmons C, Miller N, Geddie W, Gianfelice D, Oldfield M, Dranitsaris G, Clemons MJ (2009) Does confirmatory tumor biopsy alter the management of breast cancer patients with distant metastases? Ann Oncol 20:1499–1504
Santinelli A, Pisa E, Stramazzotti D, Fabris G (2008) HER-2 status discrepancy between primary breast cancer and metastatic sites. Impact on target therapy. Int J Cancer 122:999–1004
Yonemori K, Tsuta K, Shimizu C, Hatanaka Y, Hashizume K, Ono M, Nakanishi Y, Hasegawa T, Miyakita Y, Narita Y, Shibui S, Fujiwara Y (2008) Immunohistochemical profiles of brain metastases from breast cancer. J Neurooncol 90:223–228
Vincent-Salomon A, Pierga JY, Couturier J, d’Enghien CD, Nos C, Sigal-Zafrani B, Lae M, Freneaux P, Dieras V, Thiery JP, Sastre-Garau X (2007) HER2 status of bone marrow micrometastasis and their corresponding primary tumours in a pilot study of 27 cases: a possible tool for anti-HER2 therapy management? Br J Cancer 96:654–659
Schardt JA, Meyer M, Hartmann CH, Schubert F, Schmidt-Kittler O, Fuhrmann C, Polzer B, Petronio M, Eils R, Klein CA (2005) Genomic analysis of single cytokeratin-positive cells from bone marrow reveals early mutational events in breast cancer. Cancer Cell 8:227–239
Fehm T, Muller V, Aktas B, Janni W, Schneeweiss A, Stickeler E, Lattrich C, Lohberg CR, Solomayer E, Rack B, Riethdorf S, Klein C, Schindlbeck C, Brocker K, Kasimir-Bauer S, Wallwiener D, Pantel K (2010) HER2 status of circulating tumor cells in patients with metastatic breast cancer: a prospective, multicenter trial. Breast Cancer Res Treat 124(2):403–412
Meng S, Tripathy D, Shete S, Ashfaq R, Haley B, Perkins S, Beitsch P, Khan A, Euhus D, Osborne C, Frenkel E, Hoover S, Leitch M, Clifford E, Vitetta E, Morrison L, Herlyn D, Terstappen LW, Fleming T, Fehm T, Tucker T, Lane N, Wang J, Uhr J (2004) HER-2 gene amplification can be acquired as breast cancer progresses. Proc Natl Acad Sci USA 101:9393–9398
Romond EH, Perez EA, Bryant J, Suman VJ, Geyer CE Jr, Davidson NE, Tan-Chiu E, Martino S, Paik S, Kaufman PA, Swain SM, Pisansky TM, Fehrenbacher L, Kutteh LA, Vogel VG, Visscher DW, Yothers G, Jenkins RB, Brown AM, Dakhil SR, Mamounas EP, Lingle WL, Klein PM, Ingle JN, Wolmark N (2005) Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med 353:1673–1684
Fehm T, Braun S, Muller V, Janni W, Gebauer G, Marth C, Schindlbeck C, Wallwiener D, Borgen E, Naume B, Pantel K, Solomayer E (2006) A concept for the standardized detection of disseminated tumor cells in bone marrow from patients with primary breast cancer and its clinical implementation. Cancer 107:885–892
Janni W, Hepp F, Rjosk D, Kentenich C, Strobl B, Schindlbeck C, Hantschmann P, Sommer H, Pantel K, Braun S (2001) The fate and prognostic value of occult metastatic cells in the bone marrow of patients with breast carcinoma between primary treatment and recurrence. Cancer 92:46–53
Stigbrand T, Andres C, Bellanger L, Bishr OM, Bodenmuller H, Bonfrer H, Brundell J, Einarsson R, Erlandsson A, Johansson A, Leca JF, Levi M, Meier T, Nap M, Nustad K, Seguin P, Sjodin A, Sundstrom B, van Dalen A, Wiebelhaus E, Wiklund B, Arlestig L, Hilgers J (1998) Epitope specificity of 30 monoclonal antibodies against cytokeratin antigens: the ISOBM TD5-1 Workshop. Tumour Biol 19:132–152
Pantel K, Felber E, Schlimok G (1994) Detection and characterization of residual disease in breast cancer. J Hematother 3:315–322
Braun S, Pantel K, Muller P, Janni W, Hepp F, Kentenich CR, Gastroph S, Wischnik A, Dimpfl T, Kindermann G, Riethmuller G, Schlimok G (2000) Cytokeratin-positive cells in the bone marrow and survival of patients with stage I, II, or III breast cancer. N Engl J Med 342:525–533
Lang JE, Mosalpuria K, Cristofanilli M, Krishnamurthy S, Reuben J, Singh B, Bedrosian I, Meric-Bernstam F, Lucci A (2009) HER2 status predicts the presence of circulating tumor cells in patients with operable breast cancer. Breast Cancer Res Treat 113:501–507
Solomayer EF, Becker S, Pergola-Becker G, Bachmann R, Kramer B, Vogel U, Neubauer H, Wallwiener D, Huober J, Fehm TN (2006) Comparison of HER2 status between primary tumor and disseminated tumor cells in primary breast cancer patients. Breast Cancer Res Treat 98:179–184
Hayes DF, Walker TM, Singh B, Vitetta ES, Uhr JW, Gross S, Rao C, Doyle GV, Terstappen LW (2002) Monitoring expression of HER-2 on circulating epithelial cells in patients with advanced breast cancer. Int J Oncol 21:1111–1117
Pestrin M, Bessi S, Galardi F, Truglia M, Biggeri A, Biagioni C, Cappadona S, Biganzoli L, Giannini A, Di Leo A (2009) Correlation of HER2 status between primary tumors and corresponding circulating tumor cells in advanced breast cancer patients. Breast Cancer Res Treat 118:523–530
Wulfing P, Borchard J, Buerger H, Heidl S, Zanker KS, Kiesel L, Brandt B (2006) HER2-positive circulating tumor cells indicate poor clinical outcome in stage I to III breast cancer patients. Clin Cancer Res 12:1715–1720
Solomayer E, Gebauer G, Hirnle P, Janni W, Lück HJ, Becker S, Huober J, Kraemer B, Wackwitz B, Fehm T (2008) Influence of zoledronic acid on disseminated tumor cells (DTC) in primary breast cancer patients. Cancer Res 69(Suppl 2):170s–171s
Braun S, Kentenich C, Janni W, Hepp F, de Waal J, Willgeroth F, Sommer H, Pantel K (2000) Lack of effect of adjuvant chemotherapy on the elimination of single dormant tumor cells in bone marrow of high-risk breast cancer patients. J Clin Oncol 18:80–86
Klein CA, Schmidt-Kittler O, Schardt JA, Pantel K, Speicher MR, Riethmuller G (1999) Comparative genomic hybridization, loss of heterozygosity, and DNA sequence analysis of single cells. Proc Natl Acad Sci USA 96:4494–4499
Pantel K, Muller V, Auer M, Nusser N, Harbeck N, Braun S (2003) Detection and clinical implications of early systemic tumor cell dissemination in breast cancer. Clin Cancer Res 9:6326–6334
Rack B, Schindlbeck C, Strobl B, Sommer H, Friese K, Janni W (2008) Efficacy of zoledronate in treating persisting isolated tumor cells in bone marrow in patients with breast cancer. A phase II pilot study. Dtsch Med Wochenschr 133:285–289
Eidtmann H, de Boer R, Bundred N, Llombart-Cussac A, Davidson N, Neven P, von Minckwitz G, Miller J, Schenk N, Coleman R (2010) Efficacy of zoledronic acid in postmenopausal women with early breast cancer receiving adjuvant letrozole: 36-month results of the ZO-FAST study. Ann Oncol 21(11):2188–2194
Gnant M, Mlineritsch B, Stoeger H, Luschin-Ebengreuth G, Heck D, Menzel C, Jakesz R, Seifert M, Hubalek M, Pristauz G, Bauernhofer T, Eidtmann H, Eiermann W, Steger G, Kwasny W, Dubsky P, Hochreiner G, Forsthuber EP, Fesl C, Greil R (2011) Adjuvant endocrine therapy plus zoledronic acid in premenopausal women with early-stage breast cancer: 62-month follow-up from the ABCSG-12 randomised trial. Lancet Oncol 12(7):631–641
Diel IJ, Jaschke A, Solomayer EF, Gollan C, Bastert G, Sohn C, Schuetz F (2008) Adjuvant oral clodronate improves the overall survival of primary breast cancer patients with micrometastases to the bone marrow: a long-term follow-up. Ann Oncol 19:2007–2011
Braun S, Hepp F, Kentenich CR, Janni W, Pantel K, Riethmuller G, Willgeroth F, Sommer HL (1999) Monoclonal antibody therapy with edrecolomab in breast cancer patients: monitoring of elimination of disseminated cytokeratin-positive tumor cells in bone marrow. Clin Cancer Res 5:3999–4004
Hempel P, Muller P, Oruzio D, Behr W, Brockmeyer C, Wochner M, Ehnle S, Riethmuller R, Schlimok G (2000) Combination of high-dose chemotherapy and monoclonal antibody in breast-cancer patients: a pilot trial to monitor treatment effects on disseminated tumor cells. Cytotherapy 2:287–295
Kirchner EM, Gerhards R, Voigtmann R (2002) Sequential immunochemotherapy and edrecolomab in the adjuvant therapy of breast cancer: reduction of 17-1A-positive disseminated tumour cells. Ann Oncol 13:1044–1048
Piccart-Gebhart MJ, Procter M, Leyland-Jones B, Goldhirsch A, Untch M, Smith I, Gianni L, Baselga J, Bell R, Jackisch C, Cameron D, Dowsett M, Barrios CH, Steger G, Huang CS, Andersson M, Inbar M, Lichinitser M, Lang I, Nitz U, Iwata H, Thomssen C, Lohrisch C, Suter TM, Ruschoff J, Suto T, Greatorex V, Ward C, Straehle C, McFadden E, Dolci MS, Gelber RD (2005) Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med 353:1659–1672
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M, Baselga J, Norton L (2001) Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med 344:783–792
Bozionellou V, Mavroudis D, Perraki M, Papadopoulos S, Apostolaki S, Stathopoulos E, Stathopoulou A, Lianidou E, Georgoulias V (2004) Trastuzumab administration can effectively target chemotherapy-resistant cytokeratin-19 messenger RNA-positive tumor cells in the peripheral blood and bone marrow of patients with breast cancer. Clin Cancer Res 10:8185–8194
Acknowledgments
Supported by a grant from Roche and the Friedrich-Baur-Stiftung, Munich, Germany. Neither Roche nor the Friedrich-Baur-Stiftung had any influence on the study design, collection, analysis and interpretation of the data or writing of the manuscript. The authors are sincerely grateful to Heidi Coleman for her editorial support.
Conflict of interest
Brigitte Rack, Christian Schindlbeck and Wolfgang Janni have received research funding and speakers honoraria from Roche. Julia Jückstock, Margit Günthner-Biller, Ulrich Andergassen, Julia Neugebauer, Philip Hepp, Alexandra Schoberth, Doris Mayr, Thomas Zwingers and Klaus Friese have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rack, B., Jückstock, J., Günthner-Biller, M. et al. Trastuzumab clears HER2/neu-positive isolated tumor cells from bone marrow in primary breast cancer patients. Arch Gynecol Obstet 285, 485–492 (2012). https://doi.org/10.1007/s00404-011-1954-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-011-1954-2