Abstract
Aims and objectives
To compare the three techniques of hysterectomy—total laparoscopic hysterectomy (TLH), laparoscopic assisted vaginal hysterectomy (LAVH) and non-descent vaginal hysterectomy (NDVH).
Materials and methods
Ninety women with benign disease of uterus with failed medical management or not amenable to medical management were randomised into three groups for either technique of hysterectomy, thirty in each group, by the same surgeon. For each patient, intra-operative parameters including total duration of surgery, blood loss, surgical difficulty and intra-operative complications were recorded. Total hospital stay, adverse events, satisfaction rate and recuperation time was analysed and compared. Statistical analysis was done using SPSS15 software.
Results
Non-descent vaginal hysterectomy (NDVH) took least operative time and significantly lesser blood loss (p = 0.02) compared to TLH and LAVH. There was no significant difference between adverse events, recuperation time and postoperative pain between the three techniques.
Conclusions
Non-descent vaginal hysterectomy may be a preferred technique over laparoscopic hysterectomy for benign diseases of uterus where extensive pelvic dissection is not required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hysterectomy is the second most common major surgical procedure performed on women after caesarean section [1]. In India, the incidence of hysterectomy is 4–6% out of which 90% are performed for benign indications [2]. While, the incidence of hysterectomy in the Western countries is 10–20% with the highest rate in the United states and the lowest in Norway and Sweden. There are various possible approaches to hysterectomy for benign disease of uterus—abdominal hysterectomy (AH), vaginal hysterectomy (VH) and laparoscopic hysterectomy (LH). Laparoscopic approach may be used either to facilitate the ease of vaginal delivery of uterus as in laparoscopy assisted vaginal hysterectomy (LAVH) or it may be carried out completely till final detachment of uterus from pelvic wall i.e., total laparoscopic hysterectomy (TLH). Although laparoscopic hysterectomy (LH) takes longer time, its proponents have emphasized several advantages over abdominal hysterectomy in terms of intraoperative blood loss, less postoperative morbidity, rapid recovery time, shorter hospital stay, fewer febrile episodes and early return to normal activities [3].
Various studies reported till date have compared either abdominal hysterectomy with vaginal and laparoscopic hysterectomy [4–7] or vaginal with laparoscopic hysterectomy [8, 9]. A very few studies compare various techniques of hysterectomy by a same surgeon to enable a decision on a best route for gynaecologist [10–13]. The present study was conducted to compare the intra-operative and postoperative parameters among the three approaches—non-descent vaginal hysterectomy, laparoscopically assisted vaginal hysterectomy and total laparoscopic hysterectomy.
Materials and methods
This was a prospective randomised study carried out in a tertiary hospital with established laparoscopy surgery unit from April, 2007 to June, 2009. The women were recruited from the gynaecological outpatient department. The women with benign pathology of the uterus not amenable to or failed medical management were considered for the enrollment. The ethical clearance by the Institutional Review Board was taken prior to the commencement of the study.
A detailed clinical history, including past surgical history especially any high risk factors, was taken. Complete physical examination was performed before enrollment and anthropometric data including age, height, weight, and body mass index (BMI) were noted. All patients underwent a preoperative endometrial aspiration to rule out malignancy and a transvaginal ultrasound scan to estimate uterine weight according to ellipsoid formula (uterine weight = length × width × anteroposterior diameter × 0.523). Patients with uterus weighing less than 400 g were included in the study. The primary exclusion criteria were genital malignancy, acute pelvic inflammatory disease and utero-vaginal descent greater than first degree. Patients with any contraindication to laparoscopy including underlying medical conditions that could be worsened by pneumoperitoneum or trendelenburg position were also excluded from the study.
Sample size was calculated using operative time as a primary outcome measure. With a type I error of 0.05 and a power of 80%, a sample size of 30 women in each arm was required. One hundred and nine women were screened for the study. Out of these, 99 agreed to provide informed written consent. Ninety-nine women were recruited for hysterectomy and subjected to any of the three-planned procedures for hysterectomy. Randomisation was revealed to the surgeon just before induction of anaesthesia. All the procedures were performed by the same surgeon (first author). Patients in group A underwent TLH in which whole procedure was preformed laparoscopically. The patients in group B were subjected to LAVH in which laparoscopic part included transection of round ligament, ovarian ligament and medial end of the tube and dissection of bladder peritoneum. Rest of the procedure was performed vaginally. Vaginal hysterectomy in a non-prolapsed uterus without laparoscopic assistance, termed as non-descent vaginal hysterectomy constituted group C.
For laparoscopic hysterectomy, four ports were made. A 10 mm umbilical port for laparoscope, two 5 mm ports for accessory instruments in left and right iliac fossa and one extra 10 mm port on left lateral side for 10 mm ligasure. All the pedicels were coagulated and transected laparoscopically. For preservation of adnexa, the fallopian tube and the ovarian ligament were coagulated and transected. If salpingo-oophorectomy was required, the infundibulopelvic ligament was isolated, coagulated and transected following visualisation of the ureter. The uterus was cut at the vault laparoscopically with aid of intrauterine Karl Storz Carlmont Ferrand (26168D) manipulator inserted through vagina. Uterus was delivered vaginally and vault was sutured laparoscopically.
In group B, the laparoscopic part included coagulation and transection of the round ligament, ovarian ligament and medial end of the tube followed by dissection of bladder peritoneum. The procedure was then completed vaginally. The anterior and posterior cul-de-sac were opened by sharp and blunt dissection. The uterosacral ligaments, cardinal ligaments and the uterine vessels were ligated and transected. The uterus was extracted vaginally. Vaginal cuff closure was performed by number “0” vicryl suture.
Non-descent vaginal hysterectomy was carried out vaginally for group C. Incision was made in cervicovesical junction anteriorly. Bladder was pushed up anteriorly and pouch of Douglas opened posteriorly. Uterosacral ligaments, mackenrodt ligament, uterine vessels followed by round and ovarian ligament were clamped, transected. In cases of large uteri, bisection of the specimen or myomectomy was done to reduce the bulk of the uterus after uterine artery ligation. Vaginal cuff closure was performed by number “0” vicryl.
For each patient, intra-operative parameters including total duration of surgery and blood loss were recorded as primary outcome measures. Surgical difficulty, intra-operative complications, postoperative complications such as pain, febrile morbidity or infection, total duration of hospital stay, satisfaction and sexual dysfunction were recorded as secondary outcome measures. Patient satisfaction was evaluated using HRQOL (Health related quality of life) and SF-12 i.e., 12-item Short Form health survey questionnaire. Sexual dysfunction was assessed in self-designed proforma in a questionnaire where she was asked “overall, how has your sexual function been after hysterectomy” on the scale of 1–3 where 1 = very dissatisfied. 2 = somewhat dissatisfied 3 = satisfied (same as before). The patients were routinely discharged after 72 h. Follow-up visits in outpatient clinic were done at 1, 3 and 6 months.
Statistical analysis was performed using SPSS version.15, Lead tools (1991–2000 LEAD, Technology). Comparison of continuous variables (baseline characterstics) in the three groups was done using ANOVA. Kruskal–Willlis test with Mann–Whitney post hoc test was used to assess continuous variables (operating time, blood loss, hospital stay and recuperation time). Categorical variables were assessed using Fisher’s exact test. A p value < 0.05 was considered significant.
Results
Of 99 operated women, five patients were excluded (3 in group A and 2 in group B) as they required adnexal removal. This was done to minimise the selection bias leading to interference in operative time and blood loss. Four women did not come for follow-up. Hence, 90 women (30 in each group) were statistically analysed for the present study.
Baseline characteristics and indication for hysterectomy are depicted in Table 1. The mean age was 43.02 (SD ± 5.88) with a range from 32 to 56 years. Body mass index of women and uterine weight (as measured in post-surgical specimen) was comparable in three groups. When the weight of the uterus measured postoperatively was compared with that measured ultrasonographically, it showed a poor correlation using Karl Pearson correlation coefficient (r). Most common indication for hysterectomy was leiomyoma uterus (57.8% cases). Adenomyosis and abnormal uterine bleeding were other common indications.
All the patients were analysed for intra-operative and postoperative outcomes. Intraoperative parameters are tabulated in Table 2. Operating time was assessed in group A and B from initial skin incision for Verres needle to final skin closure. In group C it was estimated from first incision on cervico-vaginal junction to final suture in the vault. In the present study, TLH took significantly longer time (105 ± 23 min, mean ± SD) than NDVH (67 ± 29 min) and LAVH (89 ± 21 min). It was observed that NDVH takes less operating time than both TLH and LAVH (p = 0.004). Blood loss was quantified by measuring the amount of fluid in suction machine and then subtracting the amount of irrigation solution used. The blood loss assessed by the number of sponges soaked during vaginal hysterectomy was added in group B and C. The mean blood loss was 290 ± 124 ml in TLH, 308 ± 130 ml in LAVH and 200 ± 155 ml in NDVH. There was found to be significant difference between LAVH and NDVH (p = 0.01); also between TLH and NDVH (p = 0.02) with blood loss being minimum in NDVH group. The blood loss was more in laparoscopic hysterectomy as compared to standard vaginal hysterectomy. There was one patient in TLH group who had excessive intra-operative bleeding requiring blood transfusion in postoperative period. Another patient in LAVH group had injury due to inferior epigastric artery which was managed laparoscopically.
Surgical difficulty was assessed based on surgeon’s experience, considering the following parameters—difficulty due to adhesions, dissection of urinary bladder, difficulty due to uterine size, approach to uterine artery and need for conversion to laparotomy. There was no significant difference among the three groups in terms of surgical difficulty, visceral injury and other complications. There were four cases with previous caesarean and four cases with previous abdominal surgery. There was no major difficulty in operating these cases by either route.
There was one case of conversion to laparotomy in group A. She was a case of previous caesarean with dense adhesions between bladder peritoneum and anterior surface of uterus. Due to poor mobilisation of uterus, there was a difficulty in coagulating uterine vessels. Hence, decision was taken to perform laparotomy.
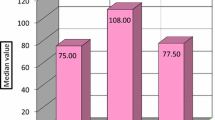
The three groups were comparable in terms of postoperative parameters including infection, vaginal bleeding, febrile episode, pain score, hospital stay and recuperation time (Table 3). Postoperative pain was determined by visual analogue scale on a grade of 1–10 as no pain to worst pain possible. Pain scoring was done at 24 h and at one week. There was no significant difference between three groups (p = 0.8). Recuperation time was defined as the time to return to normal activity. Recuperation time was the shortest in group C (14 days). When satisfaction was compared among three groups, it was similar at 4 weeks and 3 month visit. But after 6 months of surgery, there was significantly higher satisfaction rate among patients who underwent TLH and NDVH than those who underwent LAVH (p = 0.003). The satisfaction was similar between TLH and NDVH group.
Discussion
Hysterectomy is the most common gynaecological surgical procedure performed on women.
There are three popular approaches to hysterectomy for benign disease—abdominal hysterectomy (AH), vaginal hysterectomy (VH) and laparoscopic hysterectomy (LH). Laparoscopic hysterectomy has three further subdivisions—laparoscopic assisted vaginal hysterectomy (LAVH) where a vaginal hysterectomy is assisted by laparoscopic procedures that do not include uterine artery ligation, laparoscopic hysterectomy (which we will abbreviate to LH where the laparoscopic procedures include uterine artery ligation, and total laparoscopic hysterectomy (TLH) where there is no vaginal component and the vaginal vault is sutured laparoscopically [14]. Recently, robotic hysterectomy has also come in the field but it is not widely practised yet.
Multicentre studies have shown clearly that it is usually carried out by laparotomy, accounting for about three-quarters of all hysterectomies [4, 15].
The primary disadvantage of abdominal hysterectomy is the prolonged recovery period mainly contributed by longer period of pain and general malaise. This may be due to the larger abdominal incision and the procedure of laparotomy itself [16–18]. Vaginal hysterectomy is associated with fewer complications, lower need for blood transfusion and shorter period of postoperative recovery [19, 20]. The progress in laparoscopic surgery made over the past few years has proved that total laparoscopic hysterectomy (TLH) is a feasible technique [9, 21]. Laparoscopic assisted vaginal hysterectomy (LAVH) has been introduced as a surgical alternative to the standard methods of abdominal and non-descent vaginal hysterectomy. There are many surgical advantages to laparoscopy, particularly the magnification of anatomy and pathology, the ability to achieve complete haemostasis and clot evacuation during underwater examination. Patient advantages are multiple and are related to avoidance of a painful abdominal incision. These include small key-hole incision, reduced duration of hospitalisation and recuperation, and an extremely low rate of infection and paralytic ileus.
There are a very few prospective randomised studies comparing various routes and types of hysterectomies. Most of the data published involves retrospective analysis of surgical techniques. Present study was a randomised prospective clinical analysis.
The demographic profile of the patients including body mass index (BMI) and parity was comparable in the present series to the studies done previously. In all the studies comparing NDVH with LAVH, NDVH took significantly less operative time than LAVH [9, 22, 23]. The present study also showed similar result as mean time taken for NDVH was less than that for LAVH. Matteson et al. in 2009 [8] compared TLH and NDVH prospectively. The mean time for NDVH was 81 ± 30 min and that for TLH was 99 ± 25 min (p = 0.033). When we compared the three groups together, it was seen that NDVH took minimum operating time and TLH took the maximum (p = 0.004) similar to results reported in literature [8, 24–26].
We compared blood loss among three groups and found significant difference (p = 0.02), with minimum blood loss in NDVH group and maximum in LAVH group. The mean intra-operative blood loss for NDVH and LAVH in present study was comparable to that in previous studies [22, 27]. Long et al. [24] compared blood loss between TLH (mean loss of 248 ml) and LAVH (mean loss of 274 ml) and found no significant difference. There was no significant difference found between TLH and LAVH in the present study in terms of blood loss. Higher blood loss in laparoscopic surgeries may be due to longer duration for which the transacted vessels are open till occlusion is achieved by laparoscopic coagulation devices. In vaginal surgeries, the transacted vessels remained occluded by a clamp till final suture was placed.
There was no visceral injury in any of the three procedures in the present study. Complication rate of 1–2% is acceptable in hands of laparoscopically trained surgeons [28, 29]. Urinary tract injury (bladder and ureter) is the most common visceral injury encountered in laparoscopic hysterectomies. Bowel injury is rare and is usually thermal injury. Laparoscopic uterine artery ligation is the most common manoeuvre likely to increase the risk of ureteric injury especially if the surgeon is unskilled.
In our study, postoperative pain was assessed by using WHO visual analogue scale (VAS) after 24 h of surgery. All the patients were given injectable analgesics round the clock for the first 24 h. Two patients (6.6%) in TLH group had severe pain for which she required more injections of analgesics, and four patients (13.3%) in LAVH group required additional dose of analgesics due to severe pain after 24 h. In NDVH group, none of the patient had severe pain. The overall pain score and analgesic requirement in the 90 patients in three groups was not significantly different (p = 0.7).Though, the literature reports the postoperative pain and analgesic requirement may be lesser in laparoscopic surgeries [23, 30].
The three groups were similar in terms of postoperative infection, vaginal bleeding and febrile episode. The mean hospital stay in the study was minimum in NDVH group (57.6 h or 2.4 days) and it was same in LAVH (64.8 h) and TLH group (64 h), the difference being statistically non-significant (p = 0.15). The mean time to recuperation (return to normal activities or convalescence) was maximum in LAVH group (21.66 ± 10.3 days) and minimum in NDVH group (13.8 ± 4.9 days) and in TLH group, it was 16.4 ± 7.6 days. Speedier return to normal activities and improved secondary outcomes in vaginal hysterectomies has been proven in meta-analysis of randomised controlled trials [31].
When we compared sexual dysfunction in patients during follow-up at 6 weeks, 3 months and 6 months after surgery, we found no significant difference among the three groups. But in the previous study by Long et al. [24] who compared LAVH with TLH, dyspareunia decreased significantly postoperatively in the LAVH group, but not in the TLH group (p < 0.05). Patient satisfaction was evaluated after surgery at 6 weeks, 3 months and 6 months in the present study. There was significantly higher satisfaction in TLH and NDVH group as compared to LAVH group at 6 month visit. However, it has been reported that these differences disappear at 1 year [27]. Present study was limited by lack of long term follow-up at 1 year.
To conclude, non-descent vaginal hysterectomy may be a preferred approach for hysterectomy as it takes lesser operating time, it is associated with less blood loss and postoperative pain with quicker recovery and more patient satisfaction. However, the study is limited by a small sample size to differentiate in complication rates. Bias may exist due to study being carried out by a same surgeon in a single centre setup. Recall bias in reporting postoperative complication also limits the study. In cases of large uterine size, presence of adhesions due to previous abdominal surgeries and in cases where salpingo-oophorectomy is necessary, the vaginal procedure may have limitations and adjunctive laparoscopy may be required.
Total laparoscopic hysterectomy is comparable to non-descent vaginal hysterectomy in terms of postoperative parameters and satisfaction, but it has a significantly longer operative time and requires laparoscopic surgery skills.
References
Centers for Disease Control (CDC), MMWR (2002) Hysterectomy Surveillance—United States, 1994–1999. Surveillance summaries 51(SS05): 1–8
Singh AJ, Arora AK (2003) Effect of uterine prolapse on the lines of rural North Indian women. Singapore J Obstet Gynecol 34:52–58
Meikle SF, Nugent EW, Orleans M (1997) Complications and recovery from laparoscopy-assisted vaginal hysterectomy compared with abdominal and vaginal hysterectomy. Obstet Gynecol 89(2):304–311
Ribiero SC, Ribiero RM, Santos NC, Pinotti JA (2003) A randomised study of total abdominal, vaginal and laparoscopic hysterectomy. Int J Gynecol Obstet 83:37–43
Lumsden MA, Twaddle S, Hawthorn R (2000) A randomised comparison and economic evaluation of laparoscopic assisted hysterectomy and abdominal hysterectomy. BJOG 107:1386–1391
Ajmera Sachin K, Mettler L, Jonat W (2006) Operative spectrum of hysterectomy in a German university hospital. J Obstet Gynecol India 56(1):59–63
Chapron C, Laforest L, Ansquer Y, Fauconnier A, Fernandez B, Breart G et al (1999) Hysterectomy techniques used for benign pathologies: results of a French multicentric study. Hum Reprod 14(10):2464–2470
Matteson KA, Phipps MG, Raker C, Sacco LJ, Jackson AL (2009) Laparoscopic versus vaginal hysterectomy for benign pathology. Am J Obstet Gynecol 200:368e1–368e7
Summitt RL, Stovall TG, Lipscomb GH, Ling FW (1992) Randomised comparison of laparoscopic assisted vaginal hysterectomy with standard vaginal hysterectomy in an outpatient setting. Obstet Gynecol 80:895–901
Drahonovsky J, Haakova L, Otcenasek M, Krofta L, Kucera E, Feyereisl J (2010) A prospective randomized comparison of vaginal hysterectomy, laparoscopically assisted vaginal hysterectomy, and total laparoscopic hysterectomy in women with benign uterine disease. Eur J Obstet Gynecol Reprod Biol 148(2):172–176
Müller A, Thiel FC, Renner SP, Winkler M, Häberle L, Beckmann MW (2010) Hysterectomy-a comparison of approaches. Dtsch Arztebl Int 107(20):353–359
Johnson N, Barlow D, Lethaby A, Tavender E, Curr E, Garry R (2006) Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev 2:CD003677
Drahonovský J, Pán M, Baresová S, Kucera E, Feyereisl J (2006) Clinical comparison of laparoscopy-assisted vaginal hysterectomy (LAVH) and total laparoscopy hysterectomy (TLH) in women with benign disease of uterus–a prospective randomized study. Ceska Gynekol 71(6):431–437
Nieboer TE, Johnson N, Lethaby A, Tavender E, Curr E, Garry R, van Voorst S, Mol BW, Kluivers KB (2009) Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev 3:CD003677
Olsson J-H, Ferraz-Nunes J, Ellstrom M, Hahlin M (1998) A randomised trial with a cost-consequence analysis after laparoscopic and abdominal hysterectomy. Obstet Gynecol 91(1):30–34
Raju KS, Auld BJ (1994) A randomised study prospective study of laparoscopic vaginal hysterectomy versus abdominal hysterectomy each with bilateral salpingo-oophorectomy. Br J Obstet Gynecol 101:1068–1071
Nezhat F, Nezhat C, Gordon S, Wilkins E (1992) Laparoscopic versus abdominal hysterectomy. J Reprod Med 37(3):247–250
Phipps JH, John M, Nayak S (1993) Comparison of laparoscopically assisted vaginal hysterectomy and bilateral salpingo-oophorectomy with conventional abdominal hysterectomy and bilateral salpingo-oophorectomy. Br J Obstet Gynecol 100:698–700
Benassi L, Rossi T, Kaihura CT, Ricci L, Bedocchi L, Galanti B (2002) Abdominal or vaginal hysterectomy for enlarged uteri: a randomized clinical trial. Am J Obstet Gynecol 187:1561–1565
Miskry T, Magos A (2003) Randomised, prospective, double-blind comparison of abdominal and vaginal hysterectomy in women without uterovaginal prolapse. Acta Obstet Gynecol Scand 82:351–358
Reich H, Decaprio J, McGlynn F (1989) Laparoscopic hysterectomy. J Gynecol Surg 5:213–216
Ottosen C, Lingman G, Ottosen L (2000) Three methods for hysterectomy: a randomised, prospective study of short term outcome. BJOG 107:1380–1385
Soriano D, Goldstein A, Lecuru F, Darai E (2001) Recovery from vaginal hysterectomy compared with laparoscopic assisted hysterectomy: a prospective, randomised, multicentric study. Acta Obstet Gynecol Scand 80:337–341
Long CY, Fang JH, Chen WC, Su JH, Hsu SC (2002) Comparison of total laparoscopic hysterectomy and laparoscopically assisted vaginal hysterectomy. Gynecol Obstet Invest 53:214–219
Schindlbeck C, Klauser K, Dian D, Janni W, Friese K (2008) Comparison of total laparoscopic, vaginal and abdominal hysterectomy. Arch Gynecol Obstet 277(4):331–337
David-Montefiore E, Rouzier R, Chapron C, Daraï E (2007) Surgical routes and complications of hysterectomy for benign disorders: a prospective observational study in French University Hospitals. Hum Reprod 22(1):260–265
Garry R, Fountain J, Mason S, Hawe J, Napp V, Abbott J, Clayton R, Phillips G, Whittaker M, Lilford R, Bridgman S, Brown J (2004) The eVALuate study: two parallel randomized trials, one comparing laparoscopic with abdominal hysterectomy, the other comparing laparoscopic with vaginal hysterectomy. BMJ 328(7432):129–133
Canis MJ, Wattiez A, Mage G, Bruhat MA (2004) Results of eVALuate study of hysterectomy techniques: laparoscopic hysterectomy may yet have a bright future. BMJ 328(7440):642–643
Thiel F, renner S, Oppelt P (2006) Establishment of total laparoscopic hysterectomy (TLH in a university gynaecology department: results of the first 100 operations. Geburtshilfe Frauenheilkd 66:665–669
Nascimento MC, Kelley A, Martitsch C, Weidner I, Obermair A (2005) Postoperative analgesic requirements - total laparoscopic hysterectomy versus vaginal hysterectomy. Aust N Z J Obstet Gynaecol 45(2):140–143
Johnson N, Barlow D, Lethaby A, Tavender E, Curr L, Garry R (2005) Methods of hysterectomy: systematic review and meta-analysis of randomised controlled trials. BMJ 330(7506):1478
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roy, K.K., Goyal, M., Singla, S. et al. A prospective randomised study of total laparoscopic hysterectomy, laparoscopically assisted vaginal hysterectomy and non-descent vaginal hysterectomy for the treatment of benign diseases of the uterus. Arch Gynecol Obstet 284, 907–912 (2011). https://doi.org/10.1007/s00404-010-1778-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-010-1778-5