Abstract
Introduction
Peritoneal tuberculosis predominantly involves the omentum, intestinal tract, liver, spleen, and genitourinary tract and occurs in 1–4% of patients with pulmonary tuberculosis. Peritoneal tuberculosis may mimic a pelvic mass in imaging studies and also may increase CA-125 levels. Peritoneal tuberculosis may also produce massive ascites, and intraperitoneal gross appearance might be similar to the peritoneal carcinomatosis. Therefore, peritoneal tuberculosis is often confused with advanced-stage epithelial carcinoma because of similar clinical, radiologic, and laboratory findings and later intraoperative findings.
Materials and methods
The pathology records between January 2000 and August 2008 were retrospectively reviewed at 19 Mayis University Hospital. Twenty-two patients were found to have peritoneal caseating necrosis. A total of 13 out of 22 patients were found to have high CA 125 level.
Results
Among these 13 patients, 8 patients received/are receiving anti-tuberculous therapy after they were incidentally diagnosed with peritoneal tuberculosis.
Conclusion
Increased CA 125 levels should be evaluated carefully prior to aggressive surgical approach, especially in premenopausal women and frozen section evaluation should be done before extensive surgical procedure if there is any suspicion.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Peritoneal tuberculosis predominantly involves the omentum, intestinal tract, liver, spleen, and genitourinary tract and occurs in 1–4% of patients with pulmonary tuberculosis [1–3]. Although in some instances, peritoneal tuberculosis can be diagnosed clinically and radiologically, a difficulty is encountered in patients who lack typical symptoms and laboratory data. Majority of symptomless patients remain undiscovered, and the precise incidence of peritoneal tuberculosis cannot be determined [4].
Peritoneal tuberculosis may mimic a pelvic mass in imaging studies and also may increase CA 125 levels [5, 6]. Peritoneal tuberculosis may also produce massive ascites, and intraperitoneal gross appearance might be similar to the peritoneal carcinomatosis. Therefore, peritoneal tuberculosis is often confused with advanced stage epithelial carcinoma because of similar clinical, radiologic, and laboratory findings and later intraoperative findings [5–9].
In this report, we present our experience with 8 patients having high level of CA 125 who were incidentally diagnosed with peritoneal tuberculosis.
Materials and methods
The pathology records between January 2000 and August 2008 were retrospectively reviewed at the 19 Mayis University. As much as 22 patients were found to have peritoneal caseating necrosis. Among these 22 patients, 3 were either male or pediatric patients and they were excluded from the study since we did not study CA 125 levels on these patients. As much as 13 out of the 18 (72.2%) patients were found to have high CA 125 level. Among these 13 patients, 8 patients received anti-tuberculous therapy after which they were incidentally diagnosed with peritoneal tuberculosis.
Results
Eight patients with high CA 125 level were incidentally diagnosed with peritoneal tuberculosis. Six of them (75%) were premenopausal and 5 patients (57.1%) age were ≤30. Four patients underwent surgery with the preoperative diagnosis of advanced ovarian cancer. Four patients underwent surgery for benign reasons: primary infertility, pyosalpinx and cholelithiasis (and to rule out peritoneal carcinomatosis), and ascites, respectively.
Six of them were diagnosed by diagnostic laparoscopy and peritoneal biopsy; intraoperative gross appearance was consistent with peritoneal tuberculosis in five patients and one patient’s (with cholelithiasis) intraoperative findings were more suggestive of peritoneal carcinomatosis. We considered a malignant diagnosis other than tuberculosis in this patient. A laparoscopic biopsy was done for pathological diagnosis, the report of which was peritoneal tuberculosis.
Two patients, who had hysterectomy and salpingo-oophorectomy, directly had explorative laparotomy with a preoperative diagnosis of advanced stage ovarian carcinoma. Although the intraoperative findings were more suggestive of peritoneal tuberculosis than the peritoneal carcinomatosis, the surgical team has preferred to do hysterectomy and bilateral salpingo-oophorectomy which is an unnecessary operation for this benign disease.
Once these patients were diagnosed with peritoneal tuberculosis, they had chest CT to find out if they have pulmonary tuberculosis. Two patients were diagnosed with pulmonary tuberculosis. Seven patients received and one patient is receiving appropriate anti-tuberculosis treatment. All patients’ who finished the treatment, CA 125 levels returned to normal levels. The demographics, clinical characteristics, and preoperative diagnosis of the patients are shown in Table 1.
Discussion
Common symptoms of the peritoneal tuberculosis are abdominal pain, ascites, fever, weight loss, and anemia. It is well known that peritoneal tuberculosis may mimic a pelvic mass in imaging studies and also may increase CA 125 levels. Intraperitoneal gross appearance of peritoneal tuberculosis might be similar to that of the peritoneal carcinomatosis [5–9].
On physical examination ascites, abdominal tenderness, and irregular abdominopelvic masses are the most common findings in both cases with peritoneal tuberculosis and with advanced stage ovarian cancer [1, 4, 10]. Therefore, peritoneal tuberculosis is often confused with advanced stage epithelial carcinoma because of similar clinical, radiologic, and laboratory findings and later intraoperative findings [5–9].
Although CA 125 is a useful marker for the treatment monitoring and relapse detection of epithelial ovarian carcinoma, it has a low sensitivity especially in premenopausal women [9, 11]. A pelvic mass with increased tumor markers is generally accepted to the part of a malignant process [11]. Much benign gynecologic and non-gynecologic pathology, including endometriosis, leiomyomas, pelvic infection, pregnancy, renal failure, nephrotic syndrome, fulminant hepatic failure, and pancreatitis can result in elevated serum CA 125 levels, especially in younger patients [12–14]. The possibility of benign reasons, especially peritoneal tuberculosis should be considered in the differential diagnosis of ovarian carcinoma in premenopausal women [6, 13] as our three out of four patients presented with pelvic mass were premenopausal.
As much as 6 patients in this study were premenopausal and 5 were ≤30 years. Three out of the five patients’ preoperative diagnoses were primary infertility, pyosalpinx, and ascites, respectively. Tuberculosis is one of the most common causes of infertility in underdeveloped countries [15, 16].
Although there are some suggestive signs and appearance of peritoneal tuberculosis with ultrasonography and CT, these imaging studies do not have enough sensitivity or specificity for the exact diagnosis of peritoneal tuberculosis. Imaging studies would be useful in order to avoid clinical mismanagement and unnecessary surgical explorations in the peritoneal tuberculosis [9, 17]. Ultrasonographic findings of peritoneal tuberculosis consist of large volumes of ascites including septa and membranes, thickened ileal valve and bowel, mesenteric adhesions, and lymphadenopathy [9, 17]. At CT scan, one half of the patients with gastrointestinal tuberculosis show circumferential thickening of the cecum and terminal ileum, enlargement of the ileocecal valve, thickening of the medial cecal wall, exophytic extension and engulfment of the terminal ileum, and massive adenopathy are more suggestive of tuberculosis [9, 18].
The patient with cholelithiasis had vague abdominal pain. Her abdominal CT was suspicious for peritoneal carcinomatosis. Many malignancies that are not ovarian, such as gastrointestinal adenocarcinomas, have also been associated with elevated serum CA 125 levels [12, 19, 20]. We thought this patient had a gastrointestinal cancer and peritoneal metastasis. Gastroscopy, colonoscopy, chest CT, and mammography studies were done to rule out any cancer. We did not consider peritoneal tuberculosis since the patients’ history was not consistent with tuberculosis.
Laparoscopic biopsy with frozen section evaluation may be used to spare a significant number of patients from a more extensive surgical procedure, especially young women with ascites and high levels of CA 125 [1, 6]. The first trocar should be placed by open technique since these patients are more prone to intestinal injury, as we had one (patient #7) [6, 11]. Laparoscopy may not always be sufficient to provide diagnosis of tuberculous peritonitis since the gross appearance of peritoneal tuberculosis may resemble advanced ovarian carcinoma. Frozen section is mandatory to discriminate the two clinical presentations from each other [1].
Six patients underwent diagnostic laparoscopy and peritoneal biopsy. Since their biopsy came back as granulomatous inflammation and caseating necrosis the surgery was abandoned with the diagnosis of peritoneal tuberculosis. Two patients underwent unnecessary extended surgery. Similar unnecessary extended surgeries have been reported [1].
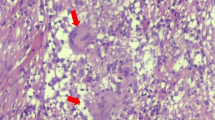
Chronic granulomatous reaction and inflammation are consistent but not pathognomonic for tuberculosis infection at histological evaluation. There are many reasons for granulomatous inflammations, such as some parasitic and fungal infections. However, these are rarely seen in omentum when compared to the tuberculosis infection. Bacteriological examination of biopsy specimen obtained at surgery should be done in addition to histology and include both staining for acid-fast bacilli and also culture for tuberculosis [1]. Mycobacterium DNA can be detected in surgical specimen by PCR [21, 22]. Elevated adenosine deaminase enzyme activity can be a helpful diagnostic test for peritoneal tuberculosis [23].
Serum CA 125 can be used to monitor the response of peritoneal tuberculosis to anti-tuberculous treatment [6, 24, 25]. CA-125 levels in all of our patients other than patient #8 (she recently started the treatment) start to decrease during the anti-tuberculous treatment and eventually decreased to normal levels (Table 2).
In conclusion, the rarity of peritoneal tuberculosis in females contributes to a low index of suspicion and therefore a low incidence of accurate preoperative diagnosis. Routine physical, radiographic, and laboratory examinations are not sensitive enough to determine the presence of peritoneal tuberculosis or to differentiate those from advanced ovarian cancers [1]. High index of suspicion in this rare presentation is perhaps as important as any diagnostic and therapeutic procedure [26]. Therefore, increased CA 125 levels should be evaluated carefully prior to aggressive surgical approach, especially in premenopausal women and frozen section evaluation should be done before extensive surgical procedure if there is any suspicion [4, 11]. Peritoneal tuberculosis should be included in the differential diagnosis of intraabdominal pathologies especially in the regions where tuberculosis is very rare [26].
References
Koc S, Beydilli G, Tulunay G, Ocalan R, Boran N, Ozgul N, Kose MF, Erdogan Z (2006) Peritoneal tuberculosis mimicking advanced ovarian cancer: a retrospective review of 22 cases. Gynecol Oncol 103:565–569
Hopewell PC (1994) Overview of clinical tuberculosis. In: Bloom BR (ed) Tuberculosis, pathogenesis, protection and control, 1st edn, Chap 3. American Society for Microbiology, Washington, DC, pp 25–46
Sinan T, Sheikh M, Ramadan S, Sahwney S, Behbehani A (2002) CT features in abdominal tuberculosis: 20 years experience. BMC Med Imaging 2:3
Mahdavi A, Malviya VK, Herschman BR (2002) Peritoneal tuberculosis disguised as ovarian cancer: an emerging clinical challenge. Gynecol Oncol 84:167–170
Engin G, Acunaş B, Acunaş G, Tunaci M (2000) Imaging of extrapulmonary tuberculosis. Radiographics 20:471–488
Bilgin T, Karabay A, Dolar E, Develioğlu OH (2001) Peritoneal tuberculosis with pelvic abdominal mass, ascites and elevated CA 125 mimicking advanced ovarian carcinoma: a series of 10 cases. Int J Gynecol Cancer 11:290–294
Tan O, Luchansky E, Rosenman S, Pua T, Azodi M (2009) Peritoneal tuberculosis with elevated serum Ca-125 level mimicking advanced stage ovarian cancer: a case report. Arch Gynecol Obstet 280:333–335
Ibrahim G, Gelzayd B, DeMatia F, Maas L (1999) CA-125 tumor-associated antigen in a patient with tuberculous peritonitis. South Med J 92:1103–1104
Dursun P, Ersoz S, Gultekin M, Aksan G, Yüce K, Ayhan A (2006) Disseminated peritoneal tuberculosis mimicking advanced-stage endodermal sinus tumor: a case report. Int J Gynecol Cancer 16:303–307
Chow KM, Chow VCY, Szeto CC (2003) Indication for peritoneal biopsy in tuberculous peritonitis. Am J Surg 185:567–573
Sheth SS (1996) Elevated CA 125 in advanced abdominal or pelvic tuberculosis. Int J Gynaecol Obstet 52:167–171
Sevinc A, Adli M, Kalender ME, Camci C (2007) Benign causes of increased serum CA-125 concentration. Lancet Oncol 8:1054–1055
Barbieri RL, Niloff JM, Bast RC Jr, Scaetzl E, Kistner RW, Knapp RC (1986) Elevated serum concentrations of CA-125 in patients with advanced endometriosis. Fertil Steril 45:630–634
Ulusoy M, Ayer A, Feyizoğlu H, Alan MS, Keskin K, Gürkan Y, Cengiz I, Kuyubaşi Z (2005) Tuberculous peritonitis and elevated serum CA 125 in a patient with chronic renal failure. Turk J Gastroenterol 16:117–118
Sheikh HH (1996) Infertility due to genital tuberculosis. J Am Assoc Gynecol Laparosc 3:453–459
Nezar M, Goda H, El-Negery M, El-Saied M, Wahab AA, Badawy AM (2009) Genital tract tuberculosis among infertile women: an old problem revisited. Arch Gynecol Obstet 280:787–791
Yapar EG, Ekici E, Karasahin E, Gökmen O (1995) Sonographic features of tuberculous peritonitis with female genital tract tuberculosis. Ultrasound Obstet Gynecol 6:121–125
Ha HK, Jung JI, Lee MS, Choi BG, Lee MG, Kim YH, Kim PN, Auh YH (1996) CT differentiation of tuberculous peritonitis and peritoneal carcinomatosis. AJR Am J Roentgenol 167:743–748
Kramer BS, Gohagan J, Prorok PC, Smart C (1993) A National Cancer Institute sponsored screening trial for prostatic, lung, colorectal, and ovarian cancers. Cancer 71:589–593
Simsek H, Kadayifci A, Okan E (1996) Importance of serum CA 125 levels in malignant peritoneal mesothelioma. Tumour Biol 17:1–4
Nordhock GT, Kolk AH, Bjunc G et al (1994) Sensitivity and specificity or PCR for detection of mycobacterium tuberculosis: a blind comparison study among seven laboratories. J Clin Microbiol 32:277–284
Akcan Y, Tuncer S, Hayran M, Sungur A, Unal S (1997) PCR on disseminated tuberculosis in bone marrow and liver biopsy specimens: correlation to histopathological and clinical diagnosis. Scand J Infect Dis 29:271–274
Voigt MD, Kalvaria I, Trey C, Berman P, Lombard C, Kirsch RE (1989) Diagnostic value of ascites adenosine deaminase in tuberculous peritonitis. Lancet 1:751–754
Thakur V, Mukherjee U, Kumar K (2001) Elevated serum cancer antigen 125 levels in advanced abdominal tuberculosis. Med Oncol 18:289–291
Mas MR, Cömert B, Sağlamkaya U, Yamanel L, Kuzhan O, Ateşkan U, Kocabalkan F (2000) CA-125; a new marker for diagnosis and follow-up of patients with tuberculous peritonitis. Dig Liver Dis 32:595–597
Sakorafas GH, Ntavatzikos A, Konstantiadou I, Karamitopoulou E, Kavatha D, Peros G (2009) Peritoneal tuberculosis in pregnancy mimicking advanced ovarian cancer: a plea to avoid hasty, radical and irreversible surgical decisions. Int J Infect Dis 13:270–272
Conflict of interest statement
There is no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ulusoy, A.N., Karabicak, I., Dicle, K. et al. Peritoneal tuberculosis in premenopausal patients with elevated serum CA 125. Arch Gynecol Obstet 282, 639–642 (2010). https://doi.org/10.1007/s00404-009-1283-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-009-1283-x