Abstract
Introduction
Genital tuberculosis is a major cause of tubal factor infertility in developing countries. Data regarding the current prevalence of tuberculosis in the infertile population are sparse.
Aims
To determine the incidence of tubal factor infertility in an infertile population seeking assisted reproduction and the prevalence of genital tuberculosis in this sub-group of patients and their symptomatology.
Materials and methods
A retrospective analysis of case records of infertile patients registered for in-vitro fertilization (IVF) between January 2007 and June 2007.
Results
Hundred and forty women with an indication for IVF were analyzed. Of these, 70 patients (50%) had tubal factor infertility. The prevalence of genital tuberculosis in tubal factor infertility was 34 out of 70 (48.5%). 82.8% of patients with tubal factor had history of prior treatment for tuberculosis. Menstrual abnormalities were seen in only 8 patients: hypomenorrhea (7) and secondary amenorrhea (1). A diagnostic hysteroscopy showed that 11 had uterine adhesions (18.9%) and 1 patient had pale endometrium. Twenty patients out of 70 cases (28.5%) showed evidence of extra genital tuberculosis.
Conclusion
Genital tuberculosis is the major causative factor for severe tubal disease requiring assisted reproduction in developing countries like India.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tuberculosis of the genital tract is one of the major causes of gynecological morbidity. Nearly 2 billion people all over the world are infected with tuberculosis; with genital tuberculosis having a global prevalence of 8–10 million [1]. Effective chemotherapy for tuberculosis has gone a long way in decreasing the spread of the disease. However, the prevalence of this condition is still increasing in developing countries probably due to increasing population and HIV infection.
Data regarding actual prevalence rates of genital tuberculosis in the general population is scant. In the infertile population, prevalence rates of <1% in the developed countries [2] has been reported. Prevalence in developing countries is on the rise with rates of 13% in 1976 [2] and 30% in 1997 [3]. Genital tuberculosis often poses a diagnostic dilemma with varied clinical presentation, diverse results on imaging and multiple diagnostic tests. It is often asymptomatic and being paucibacillary, is difficult to isolate and detect in the laboratory. In view of diverse diagnostic criteria and tests, varied prevalence rates are reported from different centres. India is an endemic country for tuberculosis (TB) with prevalence rates of genital tuberculosis in tubal factor infertility being reported to be as high as 41% [5]. But there has been no prior reported study from North India.
A retrospective analysis of case records of infertile patients registered for assisted reproduction in our tertiary care institute was done and the contribution of genital tuberculosis towards tubal factor infertility was analysed.
Materials and methods
The case records of 140 infertile women, registered for IVF (in-vitro fertilization) at the IVF clinic of the All India Institute of Medical Sciences between January 2007 and June 2007 were studied. This is a tertiary care institute that functions as a referral centre for patients from all over North India.
All the patients are investigated either in our hospital or at peripheral centres completely for factor causing infertility and on unsuccessful treatment are referred to the clinic for assisted reproduction. The incidence of tubal factor infertility and the prevalence of genital tuberculosis in this sub-group of patients, the mode of diagnosis of genital tuberculosis, their menstrual history, findings on laparoscopy and hysteroscopy and nature of tubal block were analysed.
Results
Hundred and forty women with an indication for IVF were analysed. Of these, 70 patients (50%) had tubal factor infertility. Fifty-eight women (41.4%) had been diagnosed to have tuberculosis previously. The indication for prior antitubercular treatment is shown in Table 1. The prevalence of genital tuberculosis in tubal factor infertility was 34 out of 70 patients (48.5%). 82.8% of patients with tubal factor had a history of prior treatment for tuberculosis including pulmonary, abdominal and TB lymphadenitis.
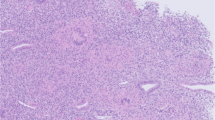
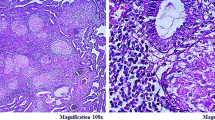
Unlike previous reports, a detailed symptomatology revealed menstrual abnormalities only in 8 patients. Rest of the 50 patients had a normal menstrual flow. Menstrual abnormalities were in the form of hypomenorrhoea (7) and secondary amenorrhoea (1). A diagnostic hysteroscopy was performed in 41 of the 58 patients. Twenty-nine patients had normal findings, 11 had uterine adhesions (18.9%) and 1 patient had pale endometrium. In cases of uterine adhesions, ten patients had Grade I adhesions on hysteroscopy and one patient had grade II adhesions that were released by operative hysteroscopy. This finding highlights that damage to the endometrium in genital tuberculosis is by far a late event and reversal of fertility in these cases is remote even after treatment.
The tubal status of all these 58 patients had been analysed by prior diagnostic or operative laparoscopy. Thirteen patients had bilateral fimbrial block, 21 had cornual block, 8 patients had unilateral hydrosalpinx and 2 bilateral hydrosalpinx, 4 had tubo-ovarian masses and 10 patients had free spill. The patients who had patent tubes had earlier been treated for tuberculosis for the following indications: granulomatous endometritis (2), PCR +ve (polymerase chain reaction) (1), pulmonary Koch’s (4), cervical tubercular lymphadenitis (1) and unknown indication (1).
Twenty patients out of 70 (28.5%) showed evidence of extra genital tuberculosis. The details of the same are shown in Table 1.
Discussion
Tubal factor infertility forms a major subset of patients requiring assisted reproduction. Genital tuberculosis was thought to be on the decline, but prevalence studies tell us that it is still a major contributor of tubal factor infertility. There has been worldwide effort to diagnose and effectively treat pulmonary tuberculosis; but extrapulmonary TB often poses a diagnostic dilemma. Being paucibacillary and asymptomatic, it is often under diagnosed. Further, in endemic countries lack of specific tests frequently leads to clinical over diagnosis and over treatment. There is a very wide difference in prevalence between developed and developing countries. Table 2 gives an overall picture of existing literature.
In comparison with previous studies our reported prevalence of 48.5% in tubal factor infertility is the highest so far. However, if we go by the gold standard for diagnosing genital TB; then the revised prevalence would be 19 out of 70 (27.14%) in our series. The criteria for diagnosis of genital tuberculosis in these 19 cases were: 8 (tubercular endometritis on histopathology), 8 (PCR +ve), 1 (peritoneal biopsy) and 1 (tubal biopsy). Fifteen cases were treated for tuberculosis for indications that do not fulfill the standard criteria for diagnosis: laparoscopy/imaging (9), Mantoux positive (3), ELISA positive (2) and pelvic abscess(1).
This study may not evidently reflect the prevalence of genital tuberculosis in the general population. But only reiterates that genital tuberculosis is the major causative factor for severe tubal disease requiring assisted reproduction in developing countries like India. There have been no earlier published reports of prevalence of tuberculosis in the infertile population requiring assisted reproduction from this part of our country for comparison. An recent case series found that the prevalence in the general infertile population was 26% and earlier reports put the number at 39–41% in tubal factor [4, 5, 15]. It may be difficult to conclude whether this represents the true scenario in the community. Firstly, the population that attends our clinic is the tip of the iceberg; ours being a tertiary referral centre for all end stage tubal disease requiring IVF. Secondly peripheral centres may not have the infrastructure to diagnose genital Koch’s nor have access to more sensitive testing, making many cases go undetected.
Earlier reports of menstrual disturbances in genital tuberculosis have been between 75 and 85% [4, 5]. But most of our patients had normal menstrual flow; 18.9 % of them had uterine adhesions on hysteroscopy. Poor conception rates are well known in these patients [5] since endometrial involvement and poor endometrium affect implantation rates in IVF [4, 6]. A recent study has questioned the role of latent tuberculosis and recurrent implantation failure [6]. This aspect requires more research and also calls for more diagnostic tests with greater specificity to detect active or latent infection. The need to treat latent infection in a country as endemic for tuberculosis like India has to be addressed to avoid over-treatment. Genital tuberculosis may cause hydrosalpinx, tubo-ovarian masses, destruction of endometrium and adhesions and questionably poorer ovarian reserve. All the above-mentioned factors may be responsible for poor conception rates in assisted reproduction.
WHO rightly called tuberculosis a global emergency; but genital tuberculosis still remains a much neglected area of research. Studies like these are grim reminders of the major role tuberculosis still plays in tubal factor infertility today. Since these patients have poor prognosis for conception, prevention is probably a better option.
References
Jassawala MJ (2006) Genital tuberculosis—a diagnostic dilemma. J Obstet Gynaecol India 56(3):203–204
Schaefer G (1976) Female genital tuberculosis. Female genital tuberculosis. Clin Obstet Gynecol 19:223
Desai P, Hazra M (1993) Tubal infertility: reappraisal of etiology. J Obstet Gynaecol India 43:76–78
Parikh FR, Nadkarni SG, Kamat SA, Naik N, Soonawala SB, Parikh RM (1997) Genital tuberculosis—a major factor causing infertility in Indian women. Fertil Steril 67:497–500
Tripathy SN, Tripathy SN (2002) Infertility and pregnancy outcome in female genital tuberculosis. Int J Gynecol Obstet 76:159–163
Dam P, Shirazee HH, Goswami SK, Ghosh S, Ganesh A, Chaudhury K, Chakravarty B (2006) Role of latent genital tuberculosis in repeated IVF failure in the Indian clinical setting. Gynecol Obstet Invest 61:223–227
Khan SM (1985) Incidence of genital tuberculosis in infertile women. J Pak Med Assoc 35:280–281
Chattopadhyay SK, Sengupta BS, Edrees YB, Al-Meshari AA (1986) The pattern of female genital tuberculosis in Riyadh, Saudi Arabia. Br J Obstet Gynaecol 93(4):367–371
Oosthuizen AP, Wessels PH, Hefer JN (1990) Tuberculosis of the female genital tract in patients attending an infertility clinic. S Afr Med J 77:562–564
De Vynck WE, Kruger TF, Joubert JJ, Scott F, Van der Merwe JP, Hulme VA, Swart Y (1990) Genital tuberculosis associated with female infertility in the western Cape. S Afr Med J 77:630–631
Marana R, Muzii L, Lucisano A, Ardito F, Muscatello P, Bilancioni E, Maniccia, Dell’Acqua S (1991) Incidence of genital tuberculosis in infertile patients submitted to diagnostic laparoscopy: recent experience in an Italian University Hospital. Int J Fertil 36(2):104–107
Haider P, Jafarey SN (1992) A histopathological study of endometrial tuberculosis in infertility. J Pak Med Assoc 42(11):269–270
Margolis K, Wranz PAB, Kruger TF, Joubert JJ, Odendaal HJ (1992) Genital tuberculosis at Tygerberg Hospital—prevalence, clinical presentation and diagnosis. S Afr Med J 81:12–15
Emembolu JO, Anyanwu DO, Ewa B (1993) Genital tuberculosis in infertile women in northern Nigeria. West Afr J Med 12:211–212
Gupta N, Sharma JB, Mittal S, Singh N, Misra R, Kukreja M (2007) Genital tuberculosis in Indian infertility patients. Int J Gynaecol Obstet 97(2):135–138
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Singh, N., Sumana, G. & Mittal, S. Genital tuberculosis: a leading cause for infertility in women seeking assisted conception in North India. Arch Gynecol Obstet 278, 325–327 (2008). https://doi.org/10.1007/s00404-008-0590-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-008-0590-y