Abstract
Previous studies have reported that genes relating to JAK-STAT pathway (IFIH1, TYK2 and IL-10) conferred the susceptibility to SLE. In this study, we performed a meta-analysis (including 43 studies) to evaluate the association between IFIH1 (9288 patients and 24,040 controls), TYK2 (4928 patients and 11,536 controls), IL-10 (3623 patients and 4907 controls) polymorphisms and systemic lupus erythematosus (SLE) in a comprehensive way. We found that IFIH1 rs1990760_T allele was associated with risk of SLE in overall population under three models (allelic: P = 2.56 × 10−11, OR 1.135, 95% CI 1.094–1.179, dominant: P = 1.8 × 10−8, OR 1.203, 95% CI 1.128–1.284, recessive: P = 2.6 × 10−7, OR 1.163, 95% CI 1.098–1.231). A strong association had been observed between TYK2 polymorphism rs2304256_C allele and SLE in Europeans (P = 5.82 × 10−5, OR 1.434, 95% CI 1.203–1.710). When coming to overall population, TYK2 rs2304256_C showed a significant association with SLE under recessive model (P = 8.05 × 10−3, OR 1.314, 95% CI 1.074–1.608). However, the other two SNPs (rs12720270, rs280519) of TYK2 were not significant. The results also indicated an association between IL-10 rs1800896_G allele and SLE in Asians under recessive model (P = 4.65 × 10−3, OR 2.623, 95% CI 1.346–5.115), while, IL-10 rs1800896_G had a trend of association with SLE in European population in dominant model (P = 1.21 × 10−2, OR 1.375, 95% CI 1.072–1.764). In addition, we found IL-10 rs1800896 GG homozygote might be associated with increased susceptibility to SLE (GG vs AA, P = 4.65 × 10−3, OR 1.539, 95% CI 1.142–2.072). We concluded that IFIH1 rs1990760_T and TYK2 rs2304256_C alleles were significantly associated with SLE, and IL-10 rs1800896 GG homozygote might have an enhancement effect on SLE risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Systemic lupus erythematosus (SLE) was a complex autoimmune disease characterized by pathogenic autoantibody production that could affect multiple organs [1]. The morbidity rate in SLE varied across different races, and it was considered that non-white racial groups were more frequently affected, for instance, 31–70/100,000 across China and 200/100,000 in African population, while it was 7–71/100,000 in Europeans [2,3,4]. Although the pathogenesis was not completely clear, it was generally known that genetic and environmental factors interacting with each other contribute to SLE risk [5]. Previous linkage analyses had identified some regions in genome for SLE, eg:1p13 [6], 1q25.1 [7], 4q24 [8], 19q13.2 [5]; however, linkage analysis could only identify large genomic regions harboring lots of susceptibility genes. The candidate gene association studies had identified some precise susceptibility genes related to SLE, involving PDCD1 [9], IRF-5 [1], FCGR2B [4], IL18 [10]. The genome-wide association studies (GWAS), which involved common variations through the entire genome, is a powerful tool to identify SLE-associated genes [7, 8, 11,12,13].
SLE-associated genes could be classified into three categories: B and T cell function-related genes [14], interferon (IFN) regulatory genes [15], and DNA repair genes [16]. A recent study had revealed that IFIH1 and TYK2 might induce the production of interferon [14].
The interferon-induced Helicase C domain 1 (IFIH1) gene, localized at chromosome 2p24.3, was a sensitive sensor of dsRNA that triggered IFN-α signaling pathway [14]. Elevated IFN-I was an obvious phenomenon in SLE patients, therefore, interferon regulatory genes were essential in the SLE pathological mechanism [17]. A recent study [18] indicated that IFIH1 rs1990760 was associated with an increased level of IFN-induced gene expression in SLE patients, in response to a given amount of serum IFN-α. IFIH1 had been identified to be associated with autoimmune diseases, such as, type I diabetes [19], Graves’ disease [20], and psoriasis [21]. Particularly, IFIH1 was identified as a susceptible gene for type I diabetes in a genome-wide association study [22].
TYK2 was located at chromosome 19p13.2, which was a part of JAK kinase, and phosphorylated and activated by combination of IFNAR and IFN-α [23] and then they signaled through the JAK-STAT (Janus kinase-signal transducer and activator of transcription) pathway to enhance expression of IFN-stimulated genes [24]. Several genetic studies were performed to analyze the relationship of TYK2 gene with SLE risk [1, 25,26,27,28,29], but the results were inconclusive. Lee et al. [30] found that TYK2 rs2304256 had a significant association with SLE in Europeans (P < 1 × 10−8), but not Asians. However, another study showed a significant association between SLE and TYK2 rs2304256 in Chinese (P = 1.85 × 10−5) [29].
IL-10 was not only a vital immunoregulatory cytokine produced by various immune cells, but also a gene related to B- and T-cells function [31]. IL-10 is located at the chromosome 1q31–1q32, which was a SLE linkage region [32]. The best-characterized signaling pathway of IL-10 was the JAK-STAT system, which could induce a series of immune responses using activated B- and T-cell [33]. Several studies have found an association between IL-10 and SLE in the past few years [31, 34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56], but the results were inconsistent.
A number of studies had tested the relationship between IFIH1, TYK2, IL-10 and SLE, but as we demonstrated above, the results were inconsistent. Therefore, we performed a comprehensive meta-analysis to evaluate the relationship of IFIH1 (rs1990760), TYK2 (rs2304256, rs280519, rs12720270), IL-10 (rs1800896, rs1800871, rs1800872) and SLE using different association models.
Materials and methods
Identification of eligible studies
To investigate the association between the three genes and SLE risk, we searched relevant articles in PubMed database and Web of Science and China National Knowledge Infrastructure (CNKI) as well as Cochrane and Embase before December 2017, using the following keywords: “TYK2”, “polymorphism”, “IFIH1” or “interferon-induced helicase C”, “IL-10” or “interleukin-10”, “SLE” or “systemic lupus erythematosus”.
Inclusion and exclusion criteria
The included studies were consistent with following conditions: (a) case/control study design; (b) providing SNP genotype distribution or allele frequency in the paper; (c) providing sample size in the paper; (d) patients were diagnosed through American College of Rheumatology criteria for SLE [57]. Accordingly, the exclusion criteria for the publications were as follows: (a) family study design; (b) repeated or overlapped publications; (c) literature reviews; (d) conference or meeting abstracts.
Data extraction
We collected information including authors, year of publishing, numbers of case and control, ethnicity, and numbers of genotype distribution. If there were no SNP genotype data, we calculated the numbers by the sample size and allele frequency.
Quality assessment
Study quality was evaluated systematically using the Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. The scale assigns a score of zero to nine stars to each article, whereby a greater number of stars indicate a higher quality study. Using this ‘star system’, each included study was judged on three broad perspectives: the selection of the study groups; the comparability of the groups; and the ascertainment of outcome of interest. Apart from that, Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement was an guideline for reporting observational studies, we also have applied it to observational studies that we have included in the present study.
Statistical analysis
Pooled ORs and 95% confidence intervals (CIs) were used to evaluate the strength of association between polymorphism and SLE risk for every eligible study. Hardy–Weinberg equilibrium (HWE) was tested in control using Chi square test [58] and it was considered as HWE deviation when P value was less than 0.05 [59]. We performed HWE test for all included studies, and removed studies that were deviated from HWE in controls. Cochran’s Q statistics was used to evaluate within- and between-study heterogeneities. And the effect of heterogenicity can be calculated with the following formula: I2 = 100% × (Q − df)/Q [60]. I2 statistic was used to quantify the extent of heterogenicity, which ranges from 0 to 100%. Mostly, if I2 < 25%, this indicated that each study was homogeneous, then the fixed model could be applied. When 25% < I2 < 75%, the heterogenicity between studies could not be ignored. If I2 > 75%, it evinced that there was high heterogenicity between studies. Apart from I2 statistic, the P value was also important for test of homogeneity. In our meta-analysis, when Pheterogeneity > 0.1, the fixed model would be chosen, otherwise the random model was applied. We carried out sensitivity analysis to evaluate the effect of an individual study on pooled OR. Egger’s and Begg’s test were used to evaluate the publication bias [61]. The software program STAT12.0 was used in data analysis.
Result
Studies inclusion and characteristics
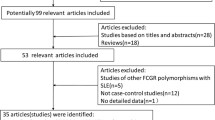
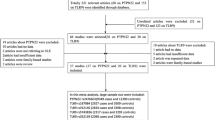
Figure 1 showed the literature searching process. 548 articles (15 for IFIH1, 26 for TYK2, 507 for IL-10) were found in PubMed database and CNKI, of which 500 studies were excluded by means of reading the title and abstract, therefore, 43 studies were included in our meta-analysis (7 for IFIH1, 7 for TYK2, 29 for IL-10). Characteristics of the included studies were summarized in Table 1. The Newcastle–Ottawa Scale (NOS) used for assessing the quality of studies was also shown in Table 1 and the scores ranged from 4 to 6. No article presented poor quality according to the Newcastle–Ottawa scale. The result of STROBE statement was presented in the TableS1. The STROBE checklist provided guidance on how to report observational research well, but not an instrument to evaluate the quality of observational research [62].
The association between IFIH1 gene polymorphism and SLE
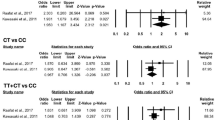
After testing the HWE deviation, 7 studies including 9288 patients and 24,040 controls were included in the meta-analysis of IFIH1 rs1990760 polymorphism and SLE. Test of heterogeneity in overall population was not significant (Pheterogeneity = 0.184), therefore, the fixed model was applied. In the allelic test, rs1990760 showed a significant association with SLE in overall population (T vs C, OR 1.135, 95% CI 1.094–1.179, P = 2.56 × 10−11, Table 2; Fig. 2a), which reached genome-wide level of significance (P < 5 × 10−8). Stratification analysis by ethnicity demonstrated an association between IFIH1 rs1990760 and SLE in Europeans (T vs. C, OR 1.148, 95% CI 1.071–1.230, P = 9.23 × 10−5, Table 2; Fig. 2a), but not Asians (T vs. C, OR 1.140, 95% CI 0.972–1.336, P = 0.107, Table 2; Fig. 2a). We also tested the recessive and dominant model for the T allele, and the result showed significance in both dominant model and recessive model in overall population (CT + TT vs CC, OR 1.203, 95% CI 1.128–1.284, P = 1.8 × 10−8, Table 2, Fig S1a; TT vs CT + CC, OR 1.163, 95% CI 1.098–1.231, P = 2.6 × 10−7, Table 2, Fig S1b) and in Europeans (CT + TT vs CC, OR 1.233, 95% CI 1.074–1.416, P = 2.88 × 10−3 Table 2, Fig S1a; TT vs CT + CC, OR 1.178, 95% CI 1.070–1.297, P = 8.38 × 10−4, Table 2, Fig S1b). In Brazilians, no association was between the rs1990760 and SLE under allelic model (T vs. C, OR 1.041, 95% CI 0.832–1.302, P = 0.723, Table 2; Fig. 2a).
a Forest plot for meta-analysis of IFIH1 rs1990760 and SLE risk (T vs. C). b Forest plot for meta-analysis of TYK2 rs2304256 and SLE risk (AC/CC vs. AA). c Forest plot for meta-analysis of IL-10 rs1800896 and SLE risk (GG vs. GA/AA). d Forest plot for meta-analysis of IL-10 rs1800896 and SLE risk (GG vs. AA)
The association between TYK2 gene polymorphisms and SLE
After testing the HWE deviation, there were 4058 patients and 5985 controls (6 studies). TYK2 rs2304256_C allele increased SLE risk in Europeans under three models (C vs. A, OR 1.434, 95% CI 1.203–1.710, P = 5.82 × 10−5, Table 3, Fig.S2a), (CC + AC vs. AA, OR 1.599, 95% CI 1.264–2.022, P = 8.85 × 10−5, Table 3; Fig. 2b; CC vs. AC + AA, OR 1.512, 95% CI 1.233–1.855, P = 7.19 × 10−5, Table 3, Fig.S2b). When coming to overall population, TYK2 rs2304256_C polymorphism showed a significant association with SLE under the recessive model (CC vs AC + AA, OR 1.314, 95% CI 1.074–1.608, P = 8.05 × 10−3, Table 3, Fig.S2b) and a marginal association under the allelic model (C vs A, OR 1.294, 95% CI 1.054–1.589, P = 0.014 Table 3, Fig.S2a). However, the C allele of rs2304256 did not confer a significant risk for the development of SLE in Asians under any models in this meta-analysis (Table 3).
Totally, 1380 patients and 3274 controls (3 studies), and 1608 patients and 8183 controls (3 studies) were recruited for rs12720270 and rs280519 after testing the HWE deviation, respectively. As shown in Table 3, there was no association between rs12720270 and rs280519 polymorphism and SLE under any models in overall population. Stratification analyses by ethnicity were not performed for the two SNPs, because all studies for rs12720270 were from Asian population considering the Hardy–Weinberg equilibrium, and for rs280519, there were only two articles done on Asians and one on Europeans.
The association between IL-10 gene polymorphism and SLE
SNP rs1800896, rs1800871, rs1800872 were regarded as tags of promoter of IL-10 gene [78, 79]. We recruited 25 studies for IL-10 rs1800896 polymorphism after testing the HWE deviation, including 3332 patients and 4612 controls. There was a slight association in overall population of three models with rs1800896 (allelic model: Table 4, Fig S3a; recessive model: Table 4; Fig. 2c; dominant model: Table 4, Fig S3b). Under recessive model, the result showed that rs1800896 had a marginal association with Asians (GG vs GA + AA, OR 2.623, 95% CI 1.346–5.115, P = 4.65 × 10−3, Table 4; Fig. 2c), but not Europeans. In the dominant model, we found an association between rs1800896 polymorphism and SLE in Europeans (GG + GA vs AA, OR 1.375, 95% CI 1.072–1.764, P = 1.21 × 10−2, Table 4, Fig S3b), but not in Asians.
We also calculated homozygous OR for genotypes (GG vs. AA) (overall: OR 1.539, 95% CI 1.142–2.072, P = 4.65 × 10−3, Europeans: OR 1.499, 95% CI 1.066–2.106, P = 1.98 × 10−2, Asians: OR 3.032, 95% CI 1.325–6.938, P = 8.54 × 10−3, Fig. 2d), which revealed that GG homozygote may increase the SLE risk. Furthermore, we analyzed the heterozygous OR for genotype GA vs. AA (overall: OR 1.229, 95% CI 0.980–1.541, P = 0.075, Europeans: OR 1.343, 95% CI 1.044–1.727, P = 2.2 × 10−2, Asians: OR 1.285, 95% CI 0.857–1.926, P = 0.226, Fig S3c).
With respect to IL-10 rs1800871, 18 articles involving 1685 patients and 2500 controls were included. We included 23 studies for IL-10 rs1800872, with a total of 2520 patients and 3870 controls. In our meta-analysis, rs1800871 and rs1800872 were not associated with SLE in overall population under any model (Table 4).
Allele frequency of the 3 SNPs in meta-analysis and in the 1000 Genomes Phase3 population
In Table 5, we presented a clear distinction of allele frequencies in different ethnicities in our meta-analysis and 1000 Genomes of the 3 SNPs. In consideration of the sample size and population, the allele frequencies of IL-10 rs1800896, and TYK2 rs2304256 in this meta-analysis were consistent with the allele frequencies in 1000 Genome project AMR (Ad Mixed American), EUR (European ancestry), EAS (East Asian ancestry), respectively; however, there was discrepancy between the allele frequencies of IFIH1 rs1990760 and 1000 Genomes Project (Table 4).
Publication bias and sensitivity analysis
Funnel plot and Bgger’s linear regression test has been used to detect the publication bias. We found no publication bias in our meta-analysis under allele genetic model (IFIH1 rs1990760, P = 0.858; TYK2 rs2304256, P = 0.260; TYK2 rs12720270, P = 0.296; TYK2 rs280519, P = 1; IL-10 rs1800896, P = 0.154; IL-10 rs1800871, P = 0.112; IL-10 rs1800872, P = 0.526, Fig.S4). We also performed sensitivity analysis to evaluate the influence of an individual study on pooled OR (Fig. S5), and the pooled OR was not substantially altered, when any one study was removed.
Discussion
JAK-STAT pathway was important for inflammatory conditions and autoimmune diseases including SLE [80], and the genes IFIH1, TYK2, IL-10 that were related to this pathway [17]. In the present meta-analysis, 43 studies were recruited to evaluate the association between IFIH1, TYK2, IL-10 and SLE risk. The result provided evidence that IFIH1 rs1990760, TYK2 rs2304256 and IL-10 rs1800896 were associated with SLE. In addition, ethnicity-specific meta-analysis indicated an association between the SNPs and SLE in Europeans but not in Asians; however, ethnicity-stratified results should be interpreted carefully.
As we all know, the progress of combination of IL-10 and its receptor could be divided into two steps. First, IL-10 binds to the IL-10R1. Then, the complex of IL-10/IL-10R1 changed the cytokine conformation through the molecular interaction. Under this condition, the complex could create a binding site which was used for combination of IL-10R2 [81,82,83]. Subsequently, two members of the Janus kinase family, Janus kinase 1 (on IL-10R1) and tyrosine kinase 2 (TYK2) (on IL-10R2) would bind with the IL-10/IL-10R complex, then creating docking sites for the transcription factor STAT3. Type-I IFN receptors which were found on all nucleated cells can be phosphorylated by TYK2, meanwhile, a report demonstrated that IFIH1 can increase IFN-α production [84].
IFIH1 rs1990760 was associated with increasing IFN-α level in SLE patients [14, 17]. And IFN-α binding to IFNAR would activate JAK-STAT pathway to induce corresponding gene transcription. There was one GWAS study [85] investigating SNP rs1990760 and SLE susceptibility in European, reaching the genome-wide significance (P = 4 × 10−8). Our study also illustrated that T allele of IFIH1 rs1990760 apparently increased the risk of SLE, but its effect was diverse in different ethnicities. We validated the association between rs1990760 and SLE in overall population and Europeans. These results were also consistent with the previous meta-analysis conducted by the Cen et al., which indicated that rs1990760 had a significant association with SLE risk in Europeans (overall: P = 3.18 × 10−5, European: P = 1.96 × 10−5) [86]. Simultaneously, it was worth mentioning that the study by Gateva et al. [34] was removed from our study due to inconsistency with Hardy–Weinberg equilibrium (P < 0.001), while it was included in the meta-analysis conducted by the Cen et al. [86]. In terms of the other meta-analysis produced by Silva [68], it also showed IFIH1 rs1990760 was associated with SLE (overall: P = 0.0266).
No association was found in our study performed on Asians; however, only two articles were included in the meta-analysis (1120 patients and 1246 controls), and further assessment is needed to clarify the relationship between rs1990760 polymorphism and SLE risk in Asians. Furthermore, the frequency of T allele is very different between Europeans and Asians in 1000 Genomes Phase3 (0.61 in European vs. 0.19 in Asians) (Table 5). Although the frequency of T allele was common in Asians, it was much lower than in Europeans. The discrepancy of T allele frequency might be the cause of the inconsistent result between the two populations.
Overproduction of the IL-10-receptor complex would lead to more autoantibodies that could damage organs and tissues [78]. Three SNPs (rs1800896, rs1800871, rs1800872) were found in the promoter region of IL-10 gene. An association was identified between IL-10 rs1800896 and SLE risk in overall population under allelic and recessive model. To be specific, the previous meta-analysis, including 1788 patients and 2673 controls by Zhou et al., found a trend of association between rs1800896 and SLE risk in the overall population under the allelic model (allelic: OR 1.125, P = 0.054) [32], after carefully comparing our study and Zhou et al., we found that we included four additional articles [70,71,72, 74] of Chinese dataset, and expanded the sample size by approximately 1.8 times, which might have had an effect on the results.
In the subgroup analysis, under the allelic model, we have indicated a suggestive association between rs1800896 and SLE risk in Europeans, but not in Asians. Our result was consistent with other studies [31, 41, 42, 47, 49, 56], which showed rs1800896_G allele did not confer the risk of SLE in Asian. For further exploring the relationship between the rs1800896 polymorphism and SLE risk in Asians, we assessed the association model. We suggested that GG homozygote might make a contribution to increasing the risk of SLE. Besides, it is noteworthy that the frequency of G allele has shown a distinct difference betweens Asian and Europeans in the 1000 Genomes Phase3 (0.052 in Asians vs. 0.453 in Europeans). The frequency of G allele in Asians was low, and a larger sample size was needed to investigate the association between rs1800896_G allele and SLE susceptibility in Asians.
In the previous studies, no association was found between the rs1800871 and SLE risk in Asians [41, 42, 47], which was consistent with our results. But, the study by Song et al. reported an trend of association between rs1800871 and SLE in Asians (P = 0.027) [87], after checking carefully, we found that two studies (Lu et al. [75] and Chong et al. [31]), that deviated from HWE, were excluded in our meta-analysis, furthermore, we included three newly published articles [48, 49, 56] in our analysis.
In the JAK-STAT pathway, the combination of IL-10 and IL-10R complex was very important, and it should be noted that TYK2 focused on the tetrameric IL-10 receptor, than creating docking sites for the transcription factor STAT3 [88]. We preformed a meta-analysis to identify the association between TYK2 rs2304256, rs12720270, rs280519 polymorphisms and SLE, respectively. In terms of TYK2 rs2304256, a genetic association between rs2304256 and SLE was significantly detected in Europeans [1, 25, 26, 28], but not in Asians [27, 69]. Simultaneously, the previous meta-analysis [30] also reported similar results. These phenomena were consistent with the recent GWAS study [85] which demonstrated a strong association between rs2304256 and SLE (P = 2.43 × 10−12) in Europeans. To identify the relationship between rs2304256 and SLE risk in different ethnicities, we conducted population stratification analyses (Europeans and Asians). A significant association was found in Europeans (P < 0.0001), but not in Asians. Though we found no association between the rs2304256 and SLE in Asians, the ethnicity-specific association should be interpreted cautiously because only three articles for Asian population were included in our study. According to the data from 1000 Genomes Phase3, the frequency of C allele was almost threefold than A allele in Europeans (C: 0.738, A: 0.262), while the frequency of the two alleles had no big difference in Asians. The discrepancy of frequency led to the difference of results; therefore, a more larger sample size is needed to investigate the relationship between rs2304256_C allele and SLE susceptibility in Asians. In our study, TYK2 rs12720270 and TKY2 rs280519 did not confer a significant risk for the development of SLE in any of the racial subgroups.
The current meta-analysis had some inevitable limitations to be taken into account. On the one hand, although our overall sample size was large, the participant number in the specific ethnic population was relatively small, with the smallest sample size of 738 patients and 2632 controls [43]. On the other hand, it was universally acknowledged that the mechanism of SLE was sophisticated. A more precise analysis could be performed because of potential confounding factors such as gene–gene and gene–environment interaction, and other life style factors.
In summary, IFIH1 rs1990760_T and TYK2 rs2304256_C alleles had a significant association with SLE susceptibility in Europeans, but not in Asians; however, the ethnicity-specific association should be interpreted cautiously because of the different sample sizes in different ethnicities. For IL-10 rs1800896, GG homozygous might contribute to SLE in Asians. Considering the limited samples in Africans and African-Americans in this analysis, further studies are still required in a larger number of samples and diverse ethnic populations.
References
Sigurdsson S, Nordmark G, Goring HH, Lindroos K, Wiman AC, Sturfelt G, Jonsen A, Rantapaa-Dahlqvist S, Moller B, Kere J, Koskenmies S, Widen E, Eloranta ML, Julkunen H, Kristjansdottir H, Steinsson K, Alm G, Ronnblom L, Syvanen AC (2005) Polymorphisms in the tyrosine kinase 2 and interferon regulatory factor 5 genes are associated with systemic lupus erythematosus. Am J Hum Genet 76:528–537
Chung SA, Taylor KE, Graham RR, Nititham J, Lee AT, Ortmann WA, Jacob CO, Alarcon-Riquelme ME, Tsao BP, Harley JB, Gaffney PM, Moser KL, Slegen, Petri M, Demirci FY, Kamboh MI, Manzi S, Gregersen PK, Langefeld CD, Behrens TW, Criswell LA (2011) Differential genetic associations for systemic lupus erythematosus based on anti-dsDNA autoantibody production. PLoS Genet 7:e1001323
Danchenko N, Satia JA, Anthony MS (2006) Epidemiology of systemic lupus erythematosus: a comparison of worldwide disease burden. Lupus 15:308–318
Zhu XW, Wang Y, Wei YH, Zhao PP, Wang XB, Rong JJ, Zhong WY, Zhang XW, Wang L, Zheng HF (2016) Comprehensive assessment of the association between FCGRs polymorphisms and the risk of systemic lupus erythematosus: evidence from a meta-analysis. Sci Rep 6:31617
Cui Y, Sheng Y, Zhang X (2013) Genetic susceptibility to SLE: recent progress from GWAS. J Autoimmun 41:25–33
Gateva V, Sandling JK, Hom G, Taylor KE, Chung SA, Sun X, Ortmann W, Kosoy R, Ferreira RC, Nordmark G (2009) A large-scale replication study identifies TNIP1, PRDM1, JAZF1, UHRF1BP1 and IL10 as risk loci for systemic lupus erythematosus. Nat Genet 41:1228–1233
International Consortium for Systemic Lupus Erythematosus Genetics (SLEGEN), Harley JB, Alarcón-Riquelme ME, Criswell LA, Jacob CO, Kimberly RP, Moser KL, Tsao BP, Vyse TJ, Langefeld CD, Nath SKGJ, Cobb BL, Mirel DB, Marion MC, Williams AH, Divers J, Wang W, Frank SG, Namjou B, Gabriel SB, Lee AT, Gregersen PK, Behrens TW, Taylor KE, Fernando M, Zidovetzki R, Gaffney PM, Edberg JC, Rioux JD, Ojwang JO, James JA, Merrill JT, Gilkeson GS, Seldin MF, Yin H, Baechler EC, Li QZ, Wakeland EK, Bruner GR, Kaufman KM (2008) Genome-wide association scan in women with systemic lupus erythematosus identifies susceptibility variants in ITGAM, PXK, KIAA1542 and other loci. Nat Genet 40:204–210
Kozyrev SV, Abelson AK, Wojcik J, Zaghlool A, Linga Reddy MV, Sanchez E, Gunnarsson I, Svenungsson E, Sturfelt G, Jonsen A, Truedsson L, Pons-Estel BA, Witte T, D’Alfonso S, Barizzone N, Danieli MG, Gutierrez C, Suarez A, Junker P, Laustrup H, Gonzalez-Escribano MF, Martin J, Abderrahim H, Alarcon-Riquelme ME (2008) Functional variants in the B-cell gene BANK1 are associated with systemic lupus erythematosus. Nat Genet 40:211–216
Prokunina L, Castillejo-López C, Öberg F, Gunnarsson I, Berg L, Magnusson V, Brookes AJ, Tentler D, Kristjansdóttir H, Gröndal G, Bolstad AI, Svenungsson E, Lundberg I, Sturfelt G, Jönssen A, Truedsson L, Lima G, Alcocer-Varela J, Jonsson R, Gyllensten UB, Harley JB, Alarcón-Segovia D, Steinsson K, Alarcón-Riquelme ME (2002) A regulatory polymorphism in PDCD1 is associated with susceptibility to systemic lupus erythematosus in humans. Nat Genet 32:666–669
Guo BR, Rong JJ, Wei YH, Zhong WY, Li CS, Liu M, Li W, Wang XB, Wang L, Zheng HF (2015) Ethnicity-stratified analysis of the association between IL-18 polymorphisms and systemic lupus erythematosus in a European population: a meta-analysis. Arch Dermatol Res 307:747–755
Han JW, Zheng HF, Cui Y, Sun LD, Ye DQ, Hu Z, Xu JH, Cai ZM, Huang W, Zhao GP, Xie HF, Fang H, Lu QJ, Xu JH, Li XP, Pan YF, Deng DQ, Zeng FQ, Ye ZZ, Zhang XY, Wang QW, Hao F, Ma L, Zuo XB, Zhou FS, Du WH, Cheng YL, Yang JQ, Shen SK, Li J, Sheng YJ, Zuo XX, Zhu WF, Gao F, Zhang PL, Guo Q, Li B, Gao M, Xiao FL, Quan C, Zhang C, Zhang Z, Zhu KJ, Li Y, Hu DY, Lu WS, Huang JL, Liu SX, Li H, Ren YQ, Wang ZX, Yang CJ, Wang PG, Zhou WM, Lv YM, Zhang AP, Zhang SQ, Lin D, Li Y, Low HQ, Shen M, Zhai ZF, Wang Y, Zhang FY, Yang S, Liu JJ, Zhang XJ (2009) Genome-wide association study in a Chinese Han population identifies nine new susceptibility loci for systemic lupus erythematosus. Nat Genet 41:1234–1237
Lee YH, Bae SC, Choi SJ, Ji JD, Song G (2012) Genome-wide pathway analysis of genome-wide association studies on systemic lupus erythematosus and rheumatoid arthritis. Mol Biol Rep 39:10627–10635
Yang W, Shen N, Ye DQ, Liu Q, Zhang Y, Qian XX, Hirankarn N, Ying D, Pan HF, Mok CC, Chan TM, Wong RW, Lee KW, Mok MY, Wong SN, Leung AM, Li XP, Avihingsanon Y, Wong CM, Lee TL, Ho MH, Lee PP, Chang YK, Li PH, Li RJ, Zhang L, Wong WH, Ng IO, Lau CS, Sham PC, Lau YL, Asian Lupus Genetics C (2010) Genome-wide association study in Asian populations identifies variants in ETS1 and WDFY4 associated with systemic lupus erythematosus. PLoS Genet 6:e1000841
Azevedo Silva JD, Addobbati C, Sandrin-Garcia P, Crovella S (2014) Systemic lupus erythematosus: old and new susceptibility genes versus clinical manifestations. Curr Genom 15:52–65
Kariuki SN, Ghodke-Puranik Y, Dorschner JM, Chrabot BS, Kelly JA, Tsao BP, Kimberly RP, Alarconriquelme ME, Jacob CO, Criswell LA (2015) Genetic analysis of the pathogenic molecular sub-phenotype interferon-alpha identifies multiple novel loci involved in systemic lupus erythematosus. Genes Immun 16:15–23
Davies RC, Pettijohn K, Fike F, Wang J, Nahas SA, Tunuguntla R, Hu H, Gatti RA, McCurdy D (2012) Defective DNA double-strand break repair in pediatric systemic lupus erythematosus. Arthritis Rheum 64:568–578
Crow MK, Olferiev M, Kirou KA (2015) Targeting of type I interferon in systemic autoimmune diseases. Transl Res 165:296–305
Robinson T, Kariuki SN, Franek BS, Kumabe M, Kumar AA, Badaracco M, Mikolaitis RA, Guerrero G, Utset TO, Drevlow BE, Zaacks LS, Grober JS, Cohen LM, Kirou KA, Crow MK, Jolly M, Niewold TB (2011) Autoimmune disease risk variant of IFIH1 is associated with increased sensitivity to IFN-alpha and serologic autoimmunity in lupus patients. J Immunol 187:1298–1303
de Azevedo Silva J, Tavares NA, Santos MM, Moura R, Guimaraes RL, Araujo J, Crovella S, Brandao LA (2015) Meta-analysis of STAT4 and IFIH1 polymorphisms in type 1 diabetes mellitus patients with autoimmune polyglandular syndrome type III. Genet Mol Res 14:17730–17738
Sutherland A, Davies J, Owen CJ, Vaikkakara S, Walker C, Cheetham TD, James RA, Perros P, Donaldson PT, Cordell HJ, Quinton R, Pearce SH (2007) Genomic polymorphism at the interferon-induced helicase (IFIH1) locus contributes to Graves’ disease susceptibility. J Clin Endocrinol Metab 92:3338–3341
Genetic Analysis of Psoriasis Consortium & the Wellcome Trust Case Control Consortium 2, Strange A, Capon F, Spencer CC, Knight J, Weale ME, Allen MH, Barton A, Band G, Bellenguez C, Bergboer JG, Blackwell JM, Bramon E, Bumpstead SJ, Casas JP, Cork MJ, Corvin A, Deloukas P, Dilthey A, Duncanson A, Edkins S, Estivill X, Fitzgerald O, Freeman C, Giardina E, Gray E, Hofer A, Huffmeier U, Hunt SE, Irvine AD, Jankowski J, Kirby B, Langford C, Lascorz J, Leman J, Leslie S, Mallbris L, Markus HS, Mathew CG, McLean WH, McManus R, Mossner R, Moutsianas L, Naluai AT, Nestle FO, Novelli G, Onoufriadis A, Palmer CN, Perricone C, Pirinen M, Plomin R, Potter SC, Pujol RM, Rautanen A, Riveira-Munoz E, Ryan AW, Salmhofer W, Samuelsson L, Sawcer SJ, Schalkwijk J, Smith CH, Stahle M, Su Z, Tazi-Ahnini R, Traupe H, Viswanathan AC, Warren RB, Weger W, Wolk K, Wood N, Worthington J, Young HS, Zeeuwen PL, Hayday A, Burden AD, Griffiths CE, Kere J, Reis A, McVean G, Evans DM, Brown MA, Barker JN, Peltonen L, Donnelly P, Trembath RC (2010) A genome-wide association study identifies new psoriasis susceptibility loci and an interaction between HLA-C and ERAP1. Nat Genet 42:985–990
Smyth DJ, Cooper JD, Bailey R, Field S, Burren O, Smink LJ, Guja C, Ionescu-Tirgoviste C, Widmer B, Dunger DB, Savage DA, Walker NM, Clayton DG, Todd JA (2006) A genome-wide association study of nonsynonymous SNPs identifies a type 1 diabetes locus in the interferon-induced helicase (IFIH1) region. Nat Genet 38:617–619
Cunninghame Graham DS, Akil M, Vyse TJ (2007) Association of polymorphisms across the tyrosine kinase gene, TYK2 in UK SLE families. Rheumatology 46:927–930
de Veer MJ, Holko M, Frevel M, Walker E, Der S, Paranjape JM, Silverman RH, Williams BR (2001) Functional classification of interferon-stimulated genes identified using microarrays. J Leukoc Biol 69:912–920
Cunninghame Graham DS, Morris DL, Bhangale TR, Criswell LA, Syvänen AC, Rönnblom L, Behrens TW, Graham RR, Vyse TJ (2011) Association of NCF2, IKZF1, IRF8, IFIH1, and TYK2 with systemic lupus erythematosus. PLoS Genet 7:e1002341
Hellquist A, Jarvinen TM, Koskenmies S, Zucchelli M, Orsmark-Pietras C, Berglind L, Panelius J, Hasan T, Julkunen H, D’Amato M, Saarialho-Kere U, Kere J (2009) Evidence for genetic association and interaction between the TYK2 and IRF5 genes in systemic lupus erythematosus. J Rheumatol 36:1631–1638
Kyogoku C, Morinobu A, Nishimura K, Sugiyama D, Hashimoto H, Tokano Y, Mimori T, Terao C, Matsuda F, Kuno T, Kumagai S (2009) Lack of association between tyrosine kinase 2 (TYK2) gene polymorphisms and susceptibility to SLE in a Japanese population. Mod Rheumatol 19:401–406
Suarez-Gestal M, Calaza M, Endreffy E, Pullmann R, Ordi-Ros J, Sebastiani GD, Ruzickova S, Jose Santos M, Papasteriades C, Marchini M, Skopouli FN, Suarez A, Blanco FJ, D’Alfonso S, Bijl M, Carreira P, Witte T, Migliaresi S, Gomez-Reino JJ, Gonzalez A, European Consortium of SLEDNAC (2009) Replication of recently identified systemic lupus erythematosus genetic associations: a case–control study. Arthritis Res Ther 11:R69
Tang L, Wan P, Wang Y, Pan J, Wang Y, B C (2015) Genetic association and interaction between the IRF5 and TYK2 genes and systemic lupus erythematosus in the Han Chinese population. Inflamm Res 64:817–824
Lee YH, Choi SJ, Ji JD, Song GG (2012) Associations between PXK and TYK2 polymorphisms and systemic lupus erythematosus: a meta-analysis. Inflamm Res 61:949–954
Chong WP, Ip WK, Wong WH, Lau CS, Chan TM, Lau YL (2004) Association of interleukin-10 promoter polymorphisms with systemic lupus erythematosus. Genes Immun 5:484–492
Zhou M, Ding L, Peng H, Wang B, Huang F, Xu WD, Li JH, Ye XR, Pan HF, Ye DQ (2013) Association of the interleukin-10 gene polymorphism (−1082A/G) with systemic lupus erythematosus: a meta-analysis. Lupus 22:128–135
Kawasaki M, Fujishiro M, Yamaguchi A, Nozawa K, Kaneko H, Takasaki Y, Takamori K, Ogawa H, Sekigawa I (2011) Possible role of the JAK/STAT pathways in the regulation of T cell-interferon related genes in systemic lupus erythematosus. Lupus 20:1231–1239
Crawley E, Woo P, Isenberg DA (1999) Single nucleotide polymorphic haplotypes of the interleukin-10 5′ flanking region are not associated with renal disease or serology in Caucasian patients with systemic lupus erythematosus. Arthritis Rheum 42:2017–2018
D’ Alfonso S, Giordano M, Mellai M, Lanceni M, Barizzone N, Marchini M, Scorza R, Danieli MG, Cappelli M, Rovere P, Sabbadini MG (2002) Association tests with systemic lupus erythematosus (SLE) of IL10 markers indicate a direct involvement of a CA repeat in the 5′ regulatory region. Genes Immun 3:454–463
da Silva HD, da Silva AP, da Silva HA, Asano NM, Maia Mde M, de Souza PR (2014) Interferon gamma and Interleukin 10 polymorphisms in Brazilian patients with systemic lupus erythematosus. Mol Biol Rep 41:2493–2500
Dijstelbloem HM, Hepkema BG, Kallenberg CG, van der Linden MW, Keijsers V, Huizinga TW, Jansen MD, van de Winkel JG (2002) The R-H polymorphism of FCγ receptor IIa as a risk factor for systemic lupus erythematosus is independent of single-nucleotide polymorphisms in the interleukin-10 gene promoter. Arthritis Rheum 46:1125–1126
Fei GZ, Svenungsson E, Frostegård J, Padyukov L (2004) The A-1087IL-10 allele is associated with cardiovascular disease in SLE. Atherosclerosis 177:409–414
Guarnizo-Zuccardi P, Lopez Y, Giraldo M, Garcia N, Rodriguez L, Ramirez L, Uribe O, Garcia L, Vasquez G (2007) Cytokine gene polymorphisms in Colombian patients with systemic lupus erythematosus. Tissue Antigens 70:376–382
Guzowski D, Chandrasekaran A, Gawel C, Palma J, Koenig J, Wang XP, Dosik M, Kaplan M, Chu CC, Chavan S, Furie R, Albesiano E, Chiorazzi N (2005) Analysis of single nucleotide polymorphisms in the promoter region of interleukin-10 by denaturing high-performance liquid chromatography. J Biomol Tech 16:154–166
Hee CS, Gun SC, Naidu R, Somnath SD, Radhakrishnan AK (2008) The relationship between single nucleotide polymorphisms of the interleukin-10 gene promoter in systemic lupus erythematosus patients in Malaysia: a pilot study. Int J Rheum Dis 11:148–154
Hirankarn N, Wongpiyabovorn J, Hanvivatvong O, Netsawang J, Akkasilpa S, Wongchinsri J, Hanvivadhanakul P, Korkit W, Avihingsanon A (2006) The synergistic effect of FC gamma receptor IIa and interleukin-10 genes on the risk to develop systemic lupus erythematosus in Thai population. Tissue Antigens 68:399–406
Hrycek A, Siekiera U, Cieślik P, Szkróbka W (2005) HLA-DRB1 and-DQB1 alleles and gene polymorphisms of selected cytokines in systemic lupus erythematosus. Rheumatol Int 26:1–6
Khoa PD, Sugiyama T, Yokochi T (2005) Polymorphism of interleukin-10 promoter and tumor necrosis factor receptor II in Vietnamese patients with systemic lupus erythematosus. Clin Rheumatol 24:11–13
Lazarus M, Hajeer AH, Turner D, Sinnott P, Worthington J, Ollier WE, Hutchinson IV (1997) Genetic variation in the interleukin 10 gene promoter and systemic lupus erythematosus. J Rheumatol 24:2314–2317
Lin YJ, Wan L, Huang CM, Sheu JJ, Chen SY, Lin TH, Chen DY, Hsueh KC, Lai CC, Tsai FJ (2010) IL-10 and TNF-alpha promoter polymorphisms in susceptibility to systemic lupus erythematosus in Taiwan. Clin Exp Rheumatol 28:318–324
Mok CC, Lanchbury JS, Chan DW, Lau CS (1998) Interleukin-10 promoter polymorphisms in Southern Chinese patients with systemic lupus erythematosus. Arthritis Rheum 41:1090–1095
Rezaei A, Ziaee V, Sharabian FT, Harsini S, Mahmoudi M, Soltani S, Sadr M, Moradinejad MH, Aghighi Y, Rezaei N (2015) Lack of association between interleukin-10, transforming growth factor-beta gene polymorphisms and juvenile-onset systemic lupus erythematosus. Clin Rheumatol 34:1059–1064
Rianthavorn P, Chokedeemeeboon C, Deekajorndech T, Suphapeetiporn K (2013) Interleukin-10 promoter polymorphisms and expression in Thai children with juvenile systemic lupus erythematosus. Lupus 22:721–726
Rood MJ, Keijsers V, van der Linden MW, Tong TQ, Borggreve SE, Verweij CL, Breedveld FC, Huizinga TW (1999) Neuropsychiatric systemic lupus erythematosus is associated with imbalance in interleukin 10 promoter haplotypes. Ann Rheum Dis 58:85–89
Rosado S, Rua-Figueroa I, Vargas JA, Garcia-Laorden MI, Losada-Fernandez I, Martin-Donaire T, Perez-Chacon G, Rodriguez-Gallego C, Naranjo-Hernandez A, Ojeda-Bruno S, Citores MJ (2008) Interleukin-10 promoter polymorphisms in patients with systemic lupus erythematosus from the Canary Islands. Int J Immunogenet 35:235–242
Sobkowiak A, Lianeri M, Wudarski M, Łącki JK, Jagodziński PP (2009) Genetic variation in the interleukin-10 gene promoter in Polish patients with systemic lupus erythematosus. Rheumatol Int 29:921–925
Suárez A, López P, Mozo L, Gutiérrez C (2005) Differential effect of IL10 and TNFα genotypes on determining susceptibility to discoid and systemic lupus erythematosus. Ann Rheum Dis 64:1605–1610
Talaat RM, Alrefaey SA, Bassyouni IH, Ashour ME, Raouf AA (2016) Genetic polymorphisms of interleukin 6 and interleukin 10 in Egyptian patients with systemic lupus erythematosus. Lupus 25:255–264
Van der Linden MW, Westendorp RG, Sturk A, Bergman W, Huizinga TW (2000) High interleukin-10 production in first-degree relatives of patients with generalized but not cutaneous lupus erythematosus. J Investig Med 48:327–334
Yu HH, Liu PH, Lin YC, Chen WJ, Lee JH, Wang LC, Yang YH, Chiang B (2010) Interleukin 4 and STAT6 gene polymorphisms are associated with systemic lupus erythematosus in Chinese patients. Lupus 19:1219–1228
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725
Thakkinstian A, McElduff P, D’Este C, Duffy D, Attia J (2005) A method for meta-analysis of molecular association studies. Stat Med 24:1291–1306
Liu P, Song J, Su H, Li L, Lu N, Yang R, Peng Z (2013) IL-10 gene polymorphisms and susceptibility to systemic lupus erythematosus: a meta-analysis. PLoS One 8:e69547
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M (2007) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Int J Surg 4:1500–1524
Molineros JE, Maiti AK, Sun C, Looger LL, Han S, Kim-Howard X, Glenn SAA, Kelly JA, Niewold TB, Gilkeson GS, Brown EE, Alarcón GS, Edberg JC, Petri M, Ramsey-Goldman R, Reveille JD, Vilá LM, Freedman BI, Tsao BP, Criswell LA, Jacob CO, Moore JH, Vyse TJ, Langefeld CL, Guthridge JM, Gaffney PM, Moser KL, Scofield RH, A-R BIOLUPUS Network, Williams SM, Merrill JTJ, Ames JA, Kaufman KM, Kimberly RP, Harley JB (2013) Admixture mapping in lupus identifies multiple functional variants within IFIH1 associated with apoptosis, inflammation, and autoantibody production. PLoS Genet 9:e1003222
Cen H, Leng RX, Wang W, Zhou M, Feng CC, Zhu Y, Yang XK, Yang M, Zhai Y, Li BZ, Liu J, Pan HF, Ye DQ (2013) Association study of IFIH1 rs1990760 polymorphism with systemic lupus erythematosus in a Chinese population. Inflammation 36:444–448
Wang C, Ahlford A, Laxman N, Nordmark G, Eloranta ML, Gunnarsson I, Svenungsson E, Padyukov L, Sturfelt G, Jönsen A, Bengtsson AA, Truedsson L, Rantapää-Dahlqvist S, Sjöwall C, Sandling JK, Rönnblom L, Syvänen AC (2013) Contribution of IKBKE and IFIH1 gene variants to SLE susceptibility. Genes Immun 14:217–222
Enevold C, Kjær L, Nielsen CH, Voss A, Jacobsen RS, Hermansen ML, Redder L, Oturai AB, Jensen PE, Bendtzen K, Jacobsen S (2014) Genetic polymorphisms of dsRNA ligating pattern recognition receptors TLR3, MDA5, and RIG-I. Association with systemic lupus erythematosus and clinical phenotypes. Rheumatol Int 34:1401–1408
Gono T, Kawaguchi Y, Sugiura T, Furuya T, Kawamoto M, Hanaoka M, Yamanaka H (2010) Interferon-induced helicase (IFIH1) polymorphism with systemic lupus erythematosus and dermatomyositis/polymyositis. Mod Rheumatol 20:466–470
Silva JA, Lima SC, Addobbati C, Moura R, Brandão LA, Pancoto JA, Donadi EA, Crovella S, Sandrin-Garcia P (2016) Association of interferon-induced helicase C domain (IFIH1) gene polymorphisms with systemic lupus erythematosus and a relevant updated meta-analysis. Genet Mol Res. https://doi.org/10.4238/gmr15048008
Li P, Chang YK, SHEK KW, Lau YL (2011) Lack of association of TYK2 gene polymorphisms in Chinese patients with systemic lupus erythematosus. J Rheumatol 38:177–178
Nan S (2003) Variations in the IL-10 promoter region confer susceptibility to systemic lupus erythematosus in Chinese population. [article in chinese]. Shanghai Yi Xue 26:452–459
Wang FY, Li GC, Xie HF, Luo QZ, Zha GZ, Ping Y (2007) Polymorphism and SLE in Chinese Han population of Hunan province [article in chinese]. Acta Laser Biol Sin 16:344–348
Lan Y, Qin J, Wu J, Tang XS, Qin JM (2007) Association between the polymorphism in interleukin-10 gene promoter and systematic lupus erythematosus in a Chinese Zhuang population in Guangxi Zhuang Nationality Autonomous Region (in chinese). Chin J Dermatol 40:555–557
Miteva L, Manolova I, Ivanova M, Stoilov R, Rashkov R (2010) Lack of association between promoter polymorphism – 1082A/G in interleukin-10 gene and genetic predisposition to systemic lupus erythematosus. Revmatologia 18(18):33–38 33–38.
Zhou H, Qu R, Tang ZH, Liu Z (2007) Investigation of the correlation between interleukin-10 promoter polymorphisms and systemic lupus erythematosus [article in chinese]. Chin J Dermatol Venereol 21:517–520
Lu LY, Cheng HH, Sung PK, Tai MH, Yeh JJ, Chen A (2005) Tumor necrosis factor-beta + 252A polymorphism is associated with systemic lupus erythematosus in Taiwan. J Formosan Med Assoc 104:563–570
Ren XY, Li Y, Ren LL, Wang L, Wang YK (2011) The research of genetic association of interleukin-10 polymorphisms with systemic lupus erythematosus [article in chinese]. Guide China Med 9:24–27
Lin PW, Huang CM, Huang CC, Tsai CH, Tsai JJ, Chang CP, Tsai FJ (2007) The association of -627 interleukin-10 promoter polymorphism in Chinese patients with systemic lupus erythematosus. Clin Rheumatol 26:298–301
Peng H, Wang W, Zhou M, Li R, Pan HF, Ye DQ (2013) Role of interleukin-10 and interleukin-10 receptor in systemic lupus erythematosus. Clin Rheumatol 32:1255–1266
Wang B, Zhu JM, Fan YG, Xu WD, Cen H, Pan HF, Ye DQ (2013) Association of the—1082G/A polymorphism in the interleukin-10 gene with systemic lupus erythematosus: a meta-analysis. Gene 519:209–216
Goropevšek A, Holcar M, Avčin T (2017) The role of STAT signaling pathways in the pathogenesis of systemic lupus erythematosus. Clin Rev Allergy Immunol 52:164–181
Reineke U, Schneider-Mergener J, Glaser RW, Stigler RD, Seifert M, Volk HD, Sabat R (1999) Evidence for conformationally different states of interleukin-10 binding of a neutralizing antibody enhances accessibility of a hidden epitope. J Mol Recognit 12:242–248
Wolk K, Witte E, Reineke U, Witte K, Friedrich M, Sterry W, Asadullah K, Volk HD, Sabat R (2005) Is there an interaction between interleukin-10 and interleukin-22? Genes Immun 6:8–18
Yoon SI, Logsdon NJ, Sheikh F, Donnelly RP, Walter MR (2006) Conformational changes mediate interleukin-10 receptor 2 (IL-10R2) binding to IL-10 and assembly of the signaling complex. J Biol Chem 281:35088–35096
Yoneyama M, Kikuchi M, Matsumoto K, Imaizumi T, Miyagishi M, Taira K, Foy E, Loo YM, Gale M, Akira S, Yonehara S, Kato A, Fujita T (2005) Shared and unique functions of the DExD/H-box helicases RIG-I, MDA5, and LGP2 in antiviral innate immunity. J Immunol 175:2851–2858
Bentham J, Morris DL, Graham DSC, Pinder CL, Tombleson P, Behrens TW, Martin J, Fairfax BP, Knight JC, Chen L, Replogle J, Syvanen AC, Ronnblom L, Graham RR, Wither JE, Rioux JD, Alarcon-Riquelme ME, Vyse TJ (2015) Genetic association analyses implicate aberrant regulation of innate and adaptive immunity genes in the pathogenesis of systemic lupus erythematosus. Nat Genet 47:1457–1464
Cen H, Wang W, Leng RX, Wang TY, Pan HF, Fan YG, Wang B, Ye DQ (2013) Association of IFIH1 rs1990760 polymorphism with susceptibility to autoimmune diseases: a meta-analysis. Autoimmunity 46:455–462
Song GG, Choi SJ, Ji JD, Lee YH (2013) Associations between interleukin-10 polymorphisms and susceptibility to systemic lupus erythematosus: a meta-analysis. Hum Immunol 74:364–370
Weber-Nordt RM, Riley JK, Greenlund AC, Moore KW, Darnell JE, Schreiber RD (1996) Stat3 recruitment by two distinct ligand-induced, tyrosine-phosphorylated docking sites in the interleukin-10 receptor intracellular domain. J Biol Chem 271:27954–27961
Acknowledgements
This study was supported by the National Natural Science Foundation of China (81501145, 81871831), the Zhejiang Provincial Natural Science Foundation for Distinguished Young Scholars of China (LR17H070001), the State Key Development Program for Basic Research of China (973 Program, 2014CB541701), the “Thousand Talents” Program, the HZNUARI-Pilot Research Grant and Guangdong Provincial Science and Technology Plan project (2014A020212434). The funding agencies had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. We thank the peer reviewers for their thorough and helpful review of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests that might be perceived to influence the results and/or discussion reported in this paper. This study re-analyzed the previous published data, therefore, this study did not involve origin human participants.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yin, Q., Wu, LC., Zheng, L. et al. Comprehensive assessment of the association between genes on JAK-STAT pathway (IFIH1, TYK2, IL-10) and systemic lupus erythematosus: a meta-analysis. Arch Dermatol Res 310, 711–728 (2018). https://doi.org/10.1007/s00403-018-1858-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-018-1858-0