Abstract
Purpose
Coronal tibiofemoral subluxation (CTFS) is considered a controversial and potential contraindication to unicompartmental knee arthroplasty (UKA) but is less discussed. The study aims to observe the CTFS in a cohort of patients before and after mobile-bearing UKA and to investigate the relationship between preoperative variables (preoperative CTFS and preoperative CTFS under valgus stress) and postoperative CTFS after mobile-bearing UKA.
Methods
The study retrospectively analyzed 181 patients (224 knees) undergoing mobile-bearing UKA from September 1 2019 to December 31 2021. By using hip-to-ankle anterior–posterior (AP) standing radiographs and valgus stress force radiographs, preoperative CTFS, preoperative CTFS under valgus stress, and postoperative CTFS were measured. CTFS was defined as the distance between the tangent line to the outermost joint edge of the lateral condyle of the femur and the tangent line of the lateral tibial plateau. All patients were divided into two groups based on postoperative CTFS, group A (postoperative CTFS ≤ 5 mm) and group B (postoperative CTFS > 5 mm). The Student’s t-test, one-way ANOVA together with Tukey’s post hoc test, the chi-square test, the Fisher’s exact test, Pearson correlation analysis, simple and multiple linear regression, and univariate and multiple logistic regression were used in the analyses.
Results
The means ± standard deviations (SD) of preoperative CTFS, preoperative CTFS under valgus stress, and postoperative CTFS were 4.96 ± 1.82 mm, 3.06 ± 1.37 mm, and 3.19 ± 1.27 mm. The difference between preoperative CTFS and postoperative CTFS was statistically significant (p < 0.001). The preoperative CTFS (6.35 ± 1.34 mm) in Group B (n = 22) was significantly higher than that (4.81 ± 1.82 mm) in Group A (n = 202) (p < 0.001), so was the variable-preoperative CTFS under valgus stress (5.41 ± 1.00 mm (Group B) > 2.80 ± 1.14 mm (Group A), p < 0.001). In Pearson correlation analysis, there was a correlation between preoperative CTFS and postoperative CTFS (r = 0.493, p < 0.001), while the correlation between preoperative CTFS under valgus stress and postoperative CTFS was stronger (r = 0.842, p < 0.001). In multiple linear regression analysis, preoperative CTFS under valgus stress (β = 0.798, 95% confidence interval (CI) = 0.714–0.883, p < 0.001) was significantly correlated with postoperative CTFS. In multiple logistic regression analysis, preoperative CTFS under valgus stress (OR = 12.412, 95% CI = 4.757–32.384, and p < 0.001) was expressed as the risk factor of postoperative CTFS (> 5 mm).
Conclusion
Preoperative CTFS can be improved significantly after mobile-bearing UKA. In addition, postoperative CTFS is correlated with preoperative CTFS under valgus stress and a higher preoperative CTFS under valgus stress will increase the risk of higher postoperative CTFS (> 5 mm).
Level of evidence
Level III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Knee osteoarthritis (OA), one of the most common orthopedic diseases, is a leading cause of pain and a huge burden on the healthcare system [1,2,3]. Unicompartmental knee arthroplasty (UKA) is a successful and reliable treatment option for end-stage OA of the knee (especially anteromedial osteoarthritis (AMOA)), which benefits patients' quality of life [4, 5]. So far, numerous studies have reported that patients with mobile-bearing UKA have good clinical outcomes and long-term survival [6,7,8,9,10].
Appropriate patient selection is critical to the success of UKA surgery. Medial UKA should be performed in patients with AMOA, correctable varus deformity, intact ligaments, and less than 15 degrees of flexion and varus deformity [11]. However, the indications and contraindications of UKA were still evolving. The classic UKA contraindications proposed by Kozinn and Scott [12] were constantly being expanded, and many studies had shown that good clinical outcomes were observed in obese patients, younger patients, extremely physically active patients, and patients with the patellofemoral joint disease [13,14,15,16,17].
Coronal tibiofemoral subluxation (CTFS), defined as the distance between the tangent line to the outermost joint edge of the lateral condyle of the femur and the tangent line of the lateral tibial plateau, is considered a controversial and potential contraindication to UKA but is less discussed [18, 19]. A few studies had reported that excessive CTFS could decrease postoperative patient report outcome measurements (PROMs) and increase the risk of lateral compartment OA in UKA patients [20, 21]. At the same time, some scholars believed that postoperative CTFS was related to the impingement of the medial part of the lateral femoral condyle and the tibial spine and was a potential cause of unexplained knee pain after UKA [22,23,24]. Therefore, CTFS is an important indicator to pay more attention to UKA surgery.
CTFS can be corrected to some extent by UKA. However, not all CTFS can be satisfactorily corrected by UKA, and excessive postoperative CTFS may have adverse effects on patient prognosis [20, 24, 25]. Therefore, predicting postoperative CTFS through preoperative indicators is particularly important for surgeons to select suitable patients. A previous study suggested that preoperative CTFS under valgus stress may be a predictor of postoperative CTFS in patients with fixed-bearing UKA [20]. However, no study explored the preoperative factors which were associated with postoperative CTFS in patients with mobile-bearing UKA.
We therefore asked: (1) Can preoperative CTFS be significantly improved after mobile-bearing UKA? (2) Do preoperative variables (preoperative CTFS and preoperative CTFS under valgus stress) correlate with postoperative CTFS after mobile-bearing UKA?
Methods
This retrospective study was conducted using patients undergoing UKA from September 1 2019 to December 31 2021. The indications for UKA were as follows: (1) patients with anteromedial osteoarthritis (AMOA); (2) patients with intact knee ligaments (anterior cruciate ligament (ACL) and medial collateral ligament (MCL)); (3) patients with flexion contracture < 15° and preserved knee range of motion; (4) patients with varus deformity < 15° and this kind of deformity is correctable [11]. The inclusion criteria were as follows: (1) patients undergoing UKA for varus knee with OA; (2) patients with anterior–posterior (AP) standing knee radiographs, lateral radiographs, hip-to-ankle AP standing radiographs, and AP valgus stress force radiographs before knee surgery; (3) patients with AP standing knee radiographs, lateral radiographs and hip-to-ankle AP standing radiographs after knee surgery. The exclusion criteria were as follows: (1) patients with poor radiographs which cannot be used for research, poor valgus stress force radiographs (excessive internal or external rotation, and the radiograph beam not parallel to the tibial plateau) especially; (2) patients with lateral CTFS; (3) patients with secondary OA; (4) patients with fractures around the knee. A total number of 181 patients (224 knees, treated as 224 patients in this study) were enrolled in this study. The flowchart is shown in Fig. 1. The study was approved by the institutional review board (approval number 2020–50-k28).
Radiographic assessments
Before surgery, all patients had AP standing knee radiographs, lateral radiographs, hip-to-ankle AP standing radiographs, and AP valgus stress force radiographs. With the patients in the supine position and the knee flexed at 20 degrees, valgus stress force radiographs were obtained by the junior physician manually applying a firm valgus force to the affected knee joint without anesthesia. The junior physician was experienced and applied valgus stress as homogeneously as possible each time. Neutral rotation and parallelism of the tibial plateau to the radiograph beam were required. Three days after surgery, the same set of radiographs (except the valgus stress force radiograph) was repeated for all patients.
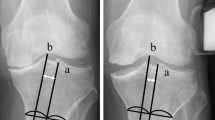
On the hip-to-ankle AP standing radiographs and valgus stress force radiographs, preoperative CTFS, preoperative CTFS under valgus stress, and postoperative CTFS were measured using the hospital's imaging system (picture archiving and communication system, PACS) (Fig. 2). CTFS was defined as the distance between the tangent line to the outermost joint edge of the lateral condyle of the femur and the tangent line of the lateral tibial plateau [18, 19]. Positive values represent medial coronal tibiofemoral subluxation, negative values represent lateral coronal tibiofemoral subluxation, and zero means no coronal tibiofemoral subluxation [24]. As lateral CTFS (CTFS < 0) was rare in UKA patients and such patients were not representative, patients with lateral subluxation on preoperative AP standing knee radiographs were excluded from the study. The subjects of this study were patients with medial CTFS (CTFS > 0) or no CTFS (CTFS = 0).
Measurement of coronal tibiofemoral subluxation (CTFS) (a–g). a The preoperative hip-to-ankle anterior–posterior (AP) standing radiograph; b partial magnification of the preoperative hip-to-ankle AP standing radiograph, and the preoperative CTFS (recorded as pre-CTFS in the figure) was measured; c the preoperative AP valgus stress force radiograph; d partial magnification of the preoperative AP valgus stress force radiograph, and the preoperative CTFS under valgus stress (recorded as pre-CTFS under valgus stress in the figure) was measured; e the postoperative hip-to-ankle AP standing radiograph; f partial magnification of the postoperative hip-to-ankle AP standing radiograph, and the postoperative CTFS (recorded as post-CTFS in the figure) was measured; g charts showing preoperative, preoperative (under valgus stress), and postoperative CTFS. The means ± standard deviations (SD) of preoperative CTFS, preoperative CTFS under valgus stress, and postoperative CTFS were 4.96 ± 1.82 mm, 3.06 ± 1.37 mm, and 3.19 ± 1.27 mm. The difference between preoperative CTFS and preoperative CTFS under valgus stress was statistically significant (p < 0.001), as was the difference between preoperative CTFS and postoperative CTFS (p < 0.001). However, no significant difference was found between preoperative CTFS under valgus stress and postoperative CTFS
Many previous studies used the CTFS value of 5 mm as the cutoff value [20, 26,27,28]. It has been shown that when the femoral prosthesis was placed at a horizontal distance of 5 mm from the center of the tibial prosthesis, there would be negative biomechanical effects [29]. Therefore, 5 mm was used as the cutoff value for this study. Patients were divided into two groups based on postoperative CTFS, group A (postoperative CTFS ≤ 5 mm) and group B (postoperative CTFS > 5 mm). In addition, patients could be divided into three groups based on preoperative and postoperative CTFS, group C (both preoperative and postoperative CTFS ≤ 5 mm), group D (preoperative CTFS > 5 mm and postoperative CTFS ≤ 5 mm), and group E (both preoperative and postoperative CTFS > 5 mm).
On the hip-to-ankle AP standing radiographs, preoperative and postoperative hip–knee–ankle angle (HKA), preoperative mechanical proximal tibial angle (mPTA), and preoperative mechanical lateral distal femoral angle (mLDFA) were measured using the hospital's imaging system (PACS) (Fig. 3). HKA was the angle between the tibial mechanical axis and femoral mechanical axis, mPTA was the angle between the tangent of the medial and lateral tibial plateau and the mechanical axis of the tibia, and mLDFA was the angle between the tangent of the medial and lateral femoral condyle and the mechanical axis of the femur [30,31,32].
Measurement of different alignment parameters on hip-to-ankle anterior–posterior (AP) standing radiographs (a–c). a The preoperative hip-to-ankle AP standing radiograph, and the preoperative hip–knee–ankle angle (HKA) (recorded as pre-HKA in the figure), mechanical lateral distal femoral angle (mLDFA), and mechanical proximal tibial angle (mPTA) were measured; b the postoperative hip-to-ankle AP standing radiograph, and the postoperative HKA (recorded as post-HKA in the figure) was measured; c charts showing preoperative and postoperative HKA. The mean ± standard deviation (SD) of preoperative HKA was 172.12 ± 3.85°, while the mean ± SD of postoperative HKA was 176.80 ± 2.30°, a difference between them was statistically significant (p < 0.001)
Two orthopedic surgeons made all measurements using the hospital's imaging system (PACS). Intra-class correlation coefficient (ICC) was used for continuous variables (preoperative HKA, preoperative mPTA, preoperative mLDFA, preoperative CTFS, preoperative CTFS under valgus stress, postoperative HKA, and postoperative CTFS) to test the interobserver reliability.
UKA procedures
All UKA operations were performed by the same surgeon using the mobile-bearing Oxford medial UKA (Zimmer-Biomet, Warsaw, Indiana) concerning the standard Oxford UKA protocol [33]. The surgeon exposed the knee joint through a small incision (an anteromedial incision along the medial border of the patella from the superior pole of the patella to the medial side of tibial tuberosity, approximately 8–10 cm) during the operation, preserving the quadriceps femoris without patella eversion. All medial osteophytes were completely removed using an osteotome. A femoral spherical mill was used to mill the distal femur condyle to balance the flexion and extension gap. After the balance of the extension and flexion gap, the tibia keel was prepared, and the prosthesis was fixed with bone cement. The ligaments were balanced in line with the polyethylene insert’s thickness. No medial release was performed during the operation.
Statistical analysis
The continuous variables (age, body mass index (BMI), preoperative HKA, postoperative HKA, preoperative mLDFA, preoperative mPTA, preoperative CTFS, preoperative CTFS under valgus stress, and postoperative CTFS) were presented as means and standard deviations (SD), while the categorical variables (sex, side, size of femoral component, size of tibial component, and size of polyethylene bearing) were given as frequencies and percentages (%).
The Student’s t-test was used to compare the differences between preoperative HKA and postoperative HKA, preoperative CTFS and preoperative CTFS under valgus stress, preoperative CTFS and postoperative CTFS, and preoperative CTFS under valgus stress and postoperative CTFS. The Student’s t-test or one-way ANOVA together with Tukey’s post hoc test (for continuous variables) and the chi-square test or Fisher’s exact test (for categorical variables) were used to compare the clinical variables between group A (postoperative CTFS ≤ 5 mm) and group B (postoperative CTFS > 5 mm) or among group C (both preoperative and postoperative CTFS ≤ 5 mm), group D (preoperative CTFS > 5 mm and postoperative CTFS ≤ 5 mm), and group E (both preoperative and postoperative CTFS > 5 mm). Pearson correlation analysis was performed among these variables, including preoperative CTFS, preoperative CTFS under valgus stress, postoperative CTFS, preoperative HKA, and postoperative HKA. Simple linear regression was carried out between the clinical variables (independent variables) and the postoperative CTFS (dependent variable). The variables (p < 0.10 in simple linear regression) were further analyzed in multiple linear regression. To assess the predictive variables of postoperative CTFS (> 5 mm), univariate and multiple logistic regression analyses (variables with p < 0.10 in univariate logistic regression) were carried out.
All analyses were performed using SPSS24.0 (IBM, New York, USA), and a p < 0.05 (two-sided) was considered statistically significant.
Results
Subject characteristics
A total of 181 patients (224 knees, treated as 224 patients in this study) were enrolled in the study. The mean ± SD (range) of age and BMI were 67.58 ± 7.51 years and 27.59 ± 3.44 kg/m2, respectively. Of all patients, 43 patients were male, and 181 patients were female; 112 patients had surgery on the left knee, while the others (112 patients) were on the right knee (Table 1). The mean ± SD of preoperative and postoperative radiographic measurements and prosthesis parameters are presented in Table 1. Excellent inter-observer reliabilities were shown in preoperative and postoperative radiographic measurements (Table 2).
The mean ± SD of preoperative CTFS, preoperative CTFS under valgus stress, and postoperative CTFS were 4.96 ± 1.82 mm, 3.06 ± 1.37 mm, and 3.19 ± 1.27 mm. The difference between preoperative CTFS and preoperative CTFS under valgus stress was statistically significant (p < 0.001), as was the difference between preoperative CTFS and postoperative CTFS (p < 0.001). However, there was no statistically significant difference between preoperative CTFS under valgus stress and postoperative CTFS (Fig. 2). The mean ± SD of preoperative HKA was 172.12 ± 3.85°, while the mean ± SD of postoperative HKA was 176.80 ± 2.30°, the difference between them was statistically significant (p < 0.001) (Fig. 3).
Comparison analysis
Of all patients, 202 patients were classified as Group A (postoperative CTFS ≤ 5 mm), while 22 patients were classified as Group B (postoperative CTFS > 5 mm). The preoperative CTFS in Group B was significantly higher than that in Group A (6.35 ± 1.34 mm vs 4.81 ± 1.82 mm, p < 0.001), so was the variable-preoperative CTFS under valgus stress (5.41 ± 1.00 mm vs 2.80 ± 1.14 mm, p < 0.001). No significant difference was found in other variables between Group A and Group B (Table 3).
Of all patients, 122 patients were classified as Group C (both preoperative and postoperative CTFS ≤ 5 mm), 80 patients were classified as Group D (preoperative CTFS > 5 mm and postoperative CTFS ≤ 5 mm), and 22 patients were classified as Group E (both preoperative and postoperative CTFS > 5 mm). The preoperative CTFS (p < 0.001) and preoperative CTFS under valgus stress (p < 0.001) differed significantly across the three groups, while no significant difference was found in other variables (Table 4).
Correlation analysis
In Pearson correlation analysis, preoperative HKA was positively related to postoperative HKA (r = 0.690, p < 0.001). There was also a correlation between preoperative CTFS and postoperative CTFS (r = 0.493, p < 0.001), and the correlation between preoperative CTFS under valgus stress and postoperative CTFS was stronger (r = 0.842, p < 0.001) (Table 5). No significant correlation was found between preoperative HKA and preoperative CTFS (r = 0.048) or preoperative CTFS under valgus stress (r = 0.033), nor between postoperative HKA and postoperative CTFS (r = – 0.033).
Simple and multiple linear regression analysis
In simple linear regression analysis, only preoperative CTFS (β = 0.344, 95%CI = 0.264–0.424, and p < 0.001) and preoperative CTFS under valgus stress (β = 0.783, 95%CI = 0.717–0.850, and p < 0.001) were significantly correlated with postoperative CTFS. In addition, the p values were 0.063 (p < 0.1) and 0.092 (p < 0.1) for preoperative mPTA and size of tibial component. For other variables, no significant correlations were found with postoperative CTFS (Table 6).
These variables (preoperative mPTA, preoperative CTFS, preoperative CTFS under valgus stress, and size of tibial component) with p < 0.1 in the simple linear regression analysis were further analyzed using multiple linear regression analysis, and only preoperative CTFS under valgus stress (β = 0.798, 95%CI = 0.714–0.883, p < 0.001) was significantly correlated with postoperative CTFS (Table 6).
Univariate and multivariate logistic regression analysis
In univariate analysis, significant correlations were found between preoperative CTFS (odds ratio (OR) = 1.642, 95%CI = 1.256–2.148, p < 0.001), preoperative CTFS under valgus stress (OR = 11.589, 95%CI = 4.773–28.138, p < 0.001) and postoperative CTFS (> 5 mm). In addition, p < 0.1 was shown in age (p = 0.055) and size of tibial component (p = 0.052). However, no significant correlations were found between other variables and postoperative CTFS (> 5 mm) (Table 7).
Variables (p < 0.1 in univariate analysis), including age, preoperative CTFS, preoperative CTFS under valgus stress, and size of the tibial component, were further analyzed using multiple logistic regression analysis. The variable-preoperative CTFS under valgus stress (OR = 12.412, 95%CI = 4.757–32.384, and p < 0.001) was expressed as the risk factor of postoperative CTFS (> 5 mm) in the multiple logistic regression analysis (Table 7).
Discussion
The main findings of this study were that preoperative CTFS could be improved significantly after mobile-bearing UKA, postoperative CTFS was correlated with preoperative CTFS under valgus stress, and a higher preoperative CTFS under valgus stress would increase the risk of higher postoperative CTFS (> 5 mm). It was worth mentioning that to our knowledge, this was the first study to quantitatively assess the effect of preoperative CTFS under valgus stress on postoperative CTFS in the mobile-bearing UKA (Oxford UKA).
CTFS has a variety of measurement methods [19, 34,35,36,37]. In this study, we measured CTFS as the distance between the tangent line to the outermost joint edge of the lateral condyle of the femur and the tangent line of the lateral tibial plateau concerning the method by Springer et al. [18]. The method had ICC values of 0.919 (preoperative CTFS), 0.908 (preoperative CTFS under valgus stress), and 0.847 (postoperative CTFS) in this study, and had an ICC value of 1.0 in the study of Springer et al. [18], indicating the high reproducibility of this measurement method. The value of preoperative CTFS in this study was 4.96 ± 1.82 mm (all patients had an intact ACL), similar to the results by Springer et al. [18], in which the preoperative CTFS value was 4.7 ± 1.4 mm (ACL functionally intact group, n = 68). Moreover, by using the measurement method, this study found that the difference between preoperative CTFS (4.96 ± 1.82 mm) and postoperative CTFS (3.19 ± 1.27 mm) was statistically significant (p < 0.001) (Table 1 and Fig. 2). Such a finding suggested that preoperative CTFS could be improved significantly with mobile-bearing UKA, which was similar to the results by Nam et al. [24] and Xi et al. [28].
CTFS is considered a controversial and potential contraindication to UKA, but it is less discussed [18, 19]. Some scholars believed that excessive postoperative CTFS may result in a mismatch in relative positioning between femoral and tibial components, which could lead to intercondylar notch impingement, component edge loading, polyethylene wear, lateral compartment OA, and poor PROMs after surgery [20,21,22,23,24,25, 38]. Kang et al. [29] reported that the femoral prosthesis placed at a horizontal distance of 5 mm from the center of the tibial prosthesis would increase the contact stress on the lateral compartment of the knee in UKA surgery. In addition, Kamenaga et al. found that UKA patients with postoperative CTFS > 5 mm (Group U: 6.5 ± 1.5 mm) had poorer PROMs 2 years after surgery than patients with postoperative CTFS < 5 mm (Group A: 3.0 ± 1.2 mm, and Group C: 3.2 ± 1.2 mm) [20] and that UKA patients with lateral osteoarthritis progression (mean follow-up: 80.8 ± 10.5 months) had higher postoperative CTFS than patients with no progression (6.6 ± 2.3 mm > 5 mm vs 4.6 ± 2.9 mm < 5 mm) [21]. Therefore, 5 mm was used as the cutoff value of postoperative CTFS, and patients were divided into two groups, group A (postoperative CTFS ≤ 5 mm) (n = 202) and group B (postoperative CTFS > 5 mm) (n = 22) in the study. The preoperative CTFS under valgus stress in Group B was significantly higher than that in Group A (5.41 ± 1.00 mm vs 2.80 ± 1.14 mm, p < 0.001) (Table 3), which was similar to the results by Kamenaga et al. [20] that the mean ± SD of postoperative CTFS was 6.5 ± 1.5 mm in Group U (patients with preoperative CTFS > 5 mm and preoperative CTFS under valgus stress > 5 mm), higher than that in Group A (patients with preoperative CTFS < 5 mm and preoperative CTFS under valgus stress < 5 mm, postoperative CTFS: 3.0 ± 1.2 mm) and Group C (patients with preoperative CTFS > 5 mm and preoperative CTFS under valgus stress < 5 mm, postoperative CTFS: 3.2 ± 1.2 mm). This might explain why we still have cases with postoperative CTFS > 5 mm after surgery and indicate that patients with high preoperative CTFS under valgus stress should be performed UKA with caution.
Preoperative valgus stress radiography has been widely used in predicting coronal alignment after UKA [39,40,41]. However, few studies have explored the relationship between preoperative valgus stress radiographs and postoperative CTFS [20, 21]. Some scholars believed that patients were suitable for UKA as long as CTFS was correctable on preoperative stress force radiographs [18, 42] and a previous study by Kamenaga et al. [20] suggested that preoperative CTFS under valgus stress might be a predictor of postoperative CTFS in patients with fixed-bearing UKA. To our knowledge, no study has explored the relationship between the preoperative CTFS under valgus stress and postoperative CTFS in patients with mobile-bearing UKA. This research first reported that preoperative CTFS under valgus stress was significantly correlated with postoperative CTFS (Table 5 and Table 6) and was shown as an independent risk factor for postoperative CTFS (> 5 mm) (Table 7) in patients undergoing mobile-bearing UKA. Such results provided a reference for clinicians in selecting suitable UKA patients, which could avoid excessive postoperative CTFS that affected the prognosis of patients undergoing mobile-bearing UKA.
In this study, there was no significant correlation between preoperative HKA and preoperative CTFS (r = 0.048) or preoperative CTFS under valgus stress (r = 0.033), nor between postoperative HKA and postoperative CTFS (r = – 0.033). Such results suggested that CTFS was a variable independent of overall mechanical alignment, which was similar to previous findings by Springer et al. [18] and Nam et al. [24]. This phenomenon might be related to the quality of the bone in the affected knee compartment. For example, a patient with medial knee OA is more likely to develop bone deformity with varus angulation than CTFS if the medial compartment has soft bone. Correspondingly, if the bone in the medial compartment is sclerotic, the patient is more likely to have CTFS with varus angulation [24, 43].
Limitations
This study had its limitations. Firstly, although the same protocol was used for each patient’s radiograph, some imaging measurements, including CTFS, were still affected by lower extremity rotation and osteophyte. Therefore, computer tomography (CT) evaluation may be a better choice for CTFS measurement. However, this study aimed to measure CTFS on readily available radiographs and the interobserver agreement for this measure was excellent, so CT was not used in the study. Secondly, the study was a retrospective analysis involving only one prosthesis (mobile-bearing medial UKA). Therefore, prospective studies using multiple types of prostheses (including fixed-bearing medial UKA) should be considered in the future. Thirdly, clinical follow-up of patients has not been performed in this study, and follow-up in the future is needed to confirm the clinical significance of CTSF (postoperative CTSF, > 5 mm vs ≤ 5 mm). However, some studies reported that excessive CTFS after UKA would lead to a decrease in PROMs and increase the risk of lateral compartment OA in patients following medial UKA [20, 21]. Fourthly, the magnitude of valgus stress of the valgus stress force radiographs in this study was not quantified using a machine such as a Telos device. However, the surgeon who performed the valgus stress force radiographs had a lot of experience and applied valgus stress as homogeneously as possible, and patients with poor quality of the valgus stress force radiographs (excessive internal or external rotation, and the radiograph beam not parallel to the tibial plateau) were excluded in the study. Finally, the cutoff value of the preoperative CTFS under valgus stress had not been calculated in this study. However, our results in the study have suggested that postoperative CTFS was correlated with preoperative CTFS under valgus stress and a higher preoperative CTFS under valgus stress would increase the risk of higher postoperative CTFS (> 5 mm), which had served the purpose of this study and was clinically meaningful.
Conclusion
Preoperative CTFS can be improved significantly after mobile-bearing UKA. In addition, postoperative CTFS is correlated with preoperative CTFS under valgus stress and a higher preoperative CTFS under valgus stress will increase the risk of higher postoperative CTFS (> 5 mm).
Availability of data and materials
All of the data are available in contact with the correspondence author.
References
Glyn-Jones S, Palmer AJR, Agricola R, Price AJ, Vincent TL, Weinans H, Carr AJ (2015) Osteoarthritis. Lancet 386(9991):376–387. https://doi.org/10.1016/s0140-6736(14)60802-3
Salaffi F, Carotti M, Stancati A, Grassi W (2005) Health-related quality of life in older adults with symptomatic hip and knee osteoarthritis: a comparison with matched healthy controls. Aging Clin Exp Res 17(4):255–263. https://doi.org/10.1007/bf03324607
Vos T, Flaxman AD, Naghavi M et al (2012) Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2163–2196. https://doi.org/10.1016/s0140-6736(12)61729-2
Seng CS, Ho DC, Chong HC, Chia SL, Chin PL, Lo NN, Yeo SJ (2017) Outcomes and survivorship of unicondylar knee arthroplasty in patients with severe deformity. Knee Surg Sports Traumatol Arthrosc 25(3):639–644. https://doi.org/10.1007/s00167-014-3464-9
Mortazavi SMJ, Vosoughi F (2022) Association of alignment variables, posteromedial tibial cartilage wear and anterior cruciate ligament insufficiency in participants with varus knee osteoarthritis: a cross-sectional study. Int Orthop. https://doi.org/10.1007/s00264-022-05358-5
Liddle AD, Judge A, Pandit H, Murray DW (2014) Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet 384(9952):1437–1445. https://doi.org/10.1016/s0140-6736(14)60419-0
Ma J, Yan Y, Wang W, Wang B, Yue D, Guo W (2021) Lower early revision rates after uncemented Oxford Unicompartmental Knee Arthroplasty (UKA) than cemented Oxford UKA: A meta-analysis. Orthop Traumatol Surg Res 107(3):102802. https://doi.org/10.1016/j.otsr.2021.102802
Mohammad HR, Mellon S, Judge A, Dodd C, Murray D (2021) The effect of body mass index on the outcomes of cementless medial mobile-bearing unicompartmental knee replacements. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06549-0
Moore DM, Sheridan GA, Welch-Phillips A, O’Byrne JM, Kenny P (2021) Good mid- to long-term results of the cemented oxford phase 3 unicompartmental knee arthroplasty in a non-designer centre. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06665-x
Pongcharoen B, Timjang J (2020) The outcomes of mobile bearing unicompartmental knee arthroplasty and total knee arthroplasty on anteromedial osteoarthritis of the knee in the same patient. Arch Orthop Trauma Surg 140(11):1783–1790. https://doi.org/10.1007/s00402-020-03527-y
Crawford DA, Berend KR, Thienpont E (2020) Unicompartmental knee arthroplasty: US and Global Perspectives. Orthop Clin North Am 51(2):147–159. https://doi.org/10.1016/j.ocl.2019.11.010
Kozinn SC, Scott R (1989) Unicondylar knee arthroplasty. J Bone Joint Surg Am 71(1):145–150
Affatato S, Caputo D, Bordini B (2019) Does the body mass index influence the long-term survival of unicompartmental knee prostheses? Retrosp Multi Centre Study Int Orthop 43(6):1365–1370. https://doi.org/10.1007/s00264-018-4217-z
Greco NJ, Lombardi AV Jr, Price AJ, Berend ME, Berend KR (2018) Medial mobile-bearing unicompartmental knee arthroplasty in young patients aged less than or equal to 50 years. J Arthroplasty 33(8):2435–2439. https://doi.org/10.1016/j.arth.2018.03.069
Berend KR, Lombardi AV Jr, Morris MJ, Hurst JM, Kavolus JJ (2011) Does preoperative patellofemoral joint state affect medial unicompartmental arthroplasty survival? Orthopedics 34(9):e494-496. https://doi.org/10.3928/01477447-20110714-39
Crawford DA, Adams JB, Lombardi AV Jr, Berend KR (2019) Activity level does not affect survivorship of unicondylar knee arthroplasty at 5 year minimum follow-up. J Arthroplasty 34(7):1364–1368. https://doi.org/10.1016/j.arth.2019.03.038
Pandit H, Jenkins C, Gill HS, Smith G, Price AJ, Dodd CA, Murray DW (2011) Unnecessary contraindications for mobile-bearing unicompartmental knee replacement. J Bone Joint Surg Br 93(5):622–628. https://doi.org/10.1302/0301-620x.93b5.26214
Springer B, Waldstein W, Bechler U, Jungwirth-Weinberger A, Windhager R, Boettner F (2021) The functional status of the ACL in varus OA of the knee: The Association With Varus Deformity and Coronal Tibiofemoral Subluxation. J Arthroplasty 36(2):501–506. https://doi.org/10.1016/j.arth.2020.08.049
Greif DN, Epstein AL, Hodgens BH, Jose J, Baraga MG (2021) Current measurement strategies of coronal tibiofemoral subluxation: a systematic review of literature. AJR Am J Roentgenol 216(5):1183–1192. https://doi.org/10.2214/ajr.20.23503
Kamenaga T, Nakano N, Ishida K, Tsubosaka M, Kuroda Y, Hayashi S, Matsushita T, Niikura T, Kuroda R, Matsumoto T (2021) Preoperative uncorrectable tibiofemoral subluxation can worsen clinical outcomes after fixed-bearing unicompartmental knee arthroplasty: a retrospective analysis. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-04157-8
Kamenaga T, Hiranaka T, Hida Y, Nakano N, Kuroda Y, Tsubosaka M, Hayashi S, Kuroda R, Matsumoto T (2021) Lateral osteoarthritis progression is associated with a postoperative residual tibiofemoral subluxation in Oxford UKA. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06729-y
Berger RA, Della Valle CJ (2010) Unicompartmental knee arthroplasty: indications, techniques, and results. Instr Course Lect 59:47–56
Boettner F, Springer B, Windhager R, Waldstein W (2020) The tibial spine sign does not indicate cartilage damage in the central area of the distal lateral femoral condyle. Knee Surg Sports Traumatol Arthrosc 28(8):2592–2597. https://doi.org/10.1007/s00167-020-05881-1
Nam D, Khamaisy S, Gladnick BP, Paul S, Pearle AD (2013) Is tibiofemoral subluxation correctable in unicompartmental knee arthroplasty? J Arthroplasty 28(9):1575–1579. https://doi.org/10.1016/j.arth.2013.03.001
Kamenaga T, Takayama K, Ishida K, Hayashi S, Kuroda R, Matsumoto T (2020) Central implantation of the femoral component relative to the tibial insert improves clinical outcomes in fixed-bearing unicompartmental knee arthroplasty. J Arthroplasty 35(11):3108–3116. https://doi.org/10.1016/j.arth.2020.05.071
Kim YT, Choi JY, Lee JK, Lee YM, Kim JI (2019) Coronal tibiofemoral subluxation is a risk factor for postoperative overcorrection in high tibial osteotomy. Knee 26(4):832–837. https://doi.org/10.1016/j.knee.2019.05.011
Buyukkuscu MO, Misir A, Kirat A, Albayrak K, Sencan K, Camurcu IY, Gursu SS (2021) Tibiofemoral subluxation in the coronal plane does not affect WOMAC and KOOS after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 29(3):914–920. https://doi.org/10.1007/s00167-020-06047-9
Xi G, Wang HH, Li H, Zhang M (2022) Short-term outcomes of Oxford unicompartmental knee arthroplasty with coronal subluxation of the knee: a retrospective case-control study. J Orthop Traumatol 23(1):6. https://doi.org/10.1186/s10195-022-00626-x
Kang KT, Son J, Koh YG, Kwon OR, Kwon SK, Lee YJ, Park KK (2018) Effect of femoral component position on biomechanical outcomes of unicompartmental knee arthroplasty. Knee 25(3):491–498. https://doi.org/10.1016/j.knee.2018.03.003
Hazratwala K, O’Callaghan WB, Dhariwal S, Wilkinson MPR (2021) Wide variation in tibial slopes and trochlear angles in the arthritic knee: a CT evaluation of 4116 pre-operative knees. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06725-2
Gielis WP, Rayegan H, Arbabi V, Ahmadi Brooghani SY, Lindner C, Cootes TF, de Jong PA, Weinans H, Custers RJH (2020) Predicting the mechanical hip-knee-ankle angle accurately from standard knee radiographs: a cross-validation experiment in 100 patients. Acta Orthop 91(6):732–737. https://doi.org/10.1080/17453674.2020.1779516
Wang JH, Weinberg DS, Amakoutou K, Cooperman DR, Liu RW (2021) The distal femur trochlear groove appears to compensate for tibial deformity but not femoral deformity in an investigation of five-hundred and seventy-nine cadaveric skeletons. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-03998-7
Murray D, Goodfellow J, O’Connor J, Dodd C (1999) Oxford Unicompartmental knee: manual of the surgical technique. Biomet UK Ltd, Bridgend, pp. 1–40
Schadler P, Kasparek M, Boettner F, Sgroi M, Faschingbauer M (2017) Coronal tibiofemoral subluxation is not an independent risk factor for total knee arthroplasty in patients with moderate to severe varus-osteoarthritis: data from the “Osteoarthritis Initiative.” Arch Orthop Trauma Surg 137(10):1423–1428. https://doi.org/10.1007/s00402-017-2777-9
Ogawa H, Matsumoto K, Akiyama H (2018) Coronal tibiofemoral subluxation is correlated to correction angle in medial opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 26(11):3482–3490. https://doi.org/10.1007/s00167-018-4948-9
Khamaisy S, Zuiderbaan HA, Thein R, Nawabi DH, Joskowicz L, Pearle AD (2014) Coronal tibiofemoral subluxation: a new measurement method. Knee 21(6):1069–1071. https://doi.org/10.1016/j.knee.2014.07.013
Khamaisy S, Zuiderbaan HA, Thein R, Gladnick BP, Pearle AD (2016) Coronal tibiofemoral subluxation in knee osteoarthritis. Skeletal Radiol 45(1):57–61. https://doi.org/10.1007/s00256-015-2244-z
Pandit H, Spiegelberg B, Clavé A, McGrath C, Liddle AD, Murray DW (2016) Aetiology of lateral progression of arthritis following Oxford medial unicompartmental knee replacement: a case-control study. Musculoskelet Surg 100(2):97–102. https://doi.org/10.1007/s12306-015-0394-8
Tashiro Y, Matsuda S, Okazaki K, Mizu-Uchi H, Kuwashima U, Iwamoto Y (2014) The coronal alignment after medial unicompartmental knee arthroplasty can be predicted: usefulness of full-length valgus stress radiography for evaluating correctability. Knee Surg Sports Traumatol Arthrosc 22(12):3142–3149. https://doi.org/10.1007/s00167-014-3248-2
Ishibashi K, Sasaki E, Otsuka H, Kazushige K, Yamamoto Y, Ishibashi Y (2020) Valgus correctability and meniscal extrusion were associated with alignment after unicompartmental knee arthroplasty. Clin Orthop Relat Res 478(7):1636–1644. https://doi.org/10.1097/corr.0000000000001260
Zhang Q, Yue J, Wang W, Chen Y, Zhao Q, Guo W (2018) FTFA change under valgus stress force radiography is useful for evaluating the correctability of intra-articular varus deformity in UKA. Arch Orthop Trauma Surg 138(7):1003–1009. https://doi.org/10.1007/s00402-018-2945-6
Costa CR, Johnson AJ, Mont MA, Bonutti PM (2011) Unicompartmental and total knee arthroplasty in the same patient. J Knee Surg 24(4):273–278. https://doi.org/10.1055/s-0031-1280970
Khamaisy S, Nam D, Thein R, Rivkin G, Liebergall M, Pearle A (2015) Limb alignment, subluxation, and bone density relationship in the osteoarthritic varus knee. J Knee Surg 28(3):207–212. https://doi.org/10.1055/s-0034-1376327
Funding
This study was funded by the Capital Health Research and Development of Special (grant number 2020-2-4067), National Natural Science Foundation of China (grant number 82072494, 81972130), and Elite Medical Professionals Project of China-Japan Friendship Hospital (NO.ZRJY2021-GG08).
Author information
Authors and Affiliations
Contributions
CQL, QDZ and WSG designed the study. CQL, JCG and XWS did the data collection. CQL, JCG and CH did the data analysis. CQL wrote the article. QDZ and WSG revised the article. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the institutional review board of China-Japan Friendship Hospital (approval number 2020–50-k28).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent to publish
All authors had consented to the submission of the article to the journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, C., Ge, J., Sun, X. et al. Coronal tibiofemoral subluxation under valgus stress force radiography is useful for evaluating postoperative coronal tibiofemoral subluxation in mobile-bearing UKA. Arch Orthop Trauma Surg 143, 4349–4361 (2023). https://doi.org/10.1007/s00402-022-04666-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04666-0