Abstract
Purpose Patients with severe deformity beyond the standard indications for unicompartmental knee arthroplasty (UKA) may be suitable and benefit from UKA. This study investigated their outcomes to determine whether good function and quality of life (QOL) can be achieved.
Materials and methods
Fifty-three patients with severe deformity (40 patients with FFD ≥15° and 13 patients with varus deformity ≥15°, Group A) were matched with 53 patients with less severe deformities who underwent UKA (Group B/controls) in terms of age, sex, BMI and duration of follow-up. Their flexion range, Knee Society scores (KSS), Oxford knee scores (OKS) and SF-36 QOL scores were analysed pre-operatively and at 2 years.
Results
Group A patients were largely similar to Group B patients pre-operatively in terms of maximum flexion angle, OKS and SF-36 scores except for knee score and mental health component of SF-36. At 2 years, Group A reported largely similar results compared with Group B in all outcome scores (OKS, KSS, SF-36) and flexion angle. Post-operative mechanical alignment was better for the control group though it is not statistically significant. There were no revisions in the patients with severe pre-operative deformity at 5 years post-operatively. (Survivorship 100 % at 5 years).
Conclusion
Selected patients with severe deformity can achieve good function and QOL with UKA if satisfactory mechanical alignment is restored. This study supports a broadening of the indications of UKA; however, further follow-up is needed to assess the longer-term durability of the operation.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The classical indications for UKA were first described by Kozinn and Scott in 1989 [5, 11, 18] and have remained largely unchallenged over the next 15 years. However, in the past 5 years, these selection criteria have come under renewed scrutiny. Good results have been reported with the Oxford unicondylar knee replacement even in patients with clinical and radiological evidence of patellofemoral disease [1, 2]. Younger patients below the age of 60 will also benefit from UKA [8, 21, 23], though data from the Australian and Swedish joint registries suggest that the risk of revision surgery is higher in younger patients, particularly those below 55 years of age [7]. Careful selection of patients is the key for a successful UKA. In addition, improved surgical techniques and advancements in UKA implant designs in recent years have lead to excellent survivorship of up to 95 % at 15 years [3, 16, 24, 26]. Conservation of bone stock, retention of both cruciate ligaments and sparing of the majority articulating joint surfaces of the knee help to preserve normal joint kinematics [3, 4, 6, 10, 13, 14, 22, 27]. This theory is proven in clinical practice: Boyd et al. [3] reported that UKA is at least equivalent to HTO in terms of functional improvement and return to recreational activities, and Walton et al. [27] reported that more UKA patients return to sport and work compared with TKA patients.
The standard caveats regarding coronal and sagittal deformity may not be valid today, given the improvements in surgical technique and implant design. Till date, no concrete study has been done to review the outcomes of UKA in patients with severe deformity beyond the standard indications. It is not known nor proven that patients with severe deformity who underwent UKA will have significantly poorer outcomes or require early revision surgery.
This study’s hypothesis was that patients with more severe angular deformities would still be able to achieve satisfactory functional and quality-of-life outcomes with UKA, provided that limited but adequate soft tissue releases as well as complete osteophyte excision were performed to supplement the bone cuts for restoration of the neutral mechanical axis.
Materials and methods
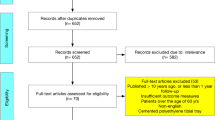
From 2004 to 2007, 53 patients with severe deformity (Group A) who underwent UKA were matched with 53 patients with less severe deformity (Group B/control) in terms of age, sex, BMI and duration of follow-up. Of these 53 patients with severe deformity, there were 40 patients with fixed flexion deformity (FFD) ≥15° and 13 patients with varus deformity ≥15°. There were no patients with both FFD ≥15° and varus deformity ≥15° in the same knee. All data were prospectively collected at a centralised diagnostic centre and managed by an institutional joint registry with the requisite data protection and integrity protocols.
The UKA implants used in this study are the Preservation UKA (DePuy Int., Leeds UK) and Miller-Gallante UKA (Zimmer, Warsaw, USA). Implant choice was based on surgeon preference. Both implants are cemented fixed-bearing designs.
Although the pre-operative deformities of these patients were beyond the classical indications, the pre-operative radiographs demonstrated predominant medial compartment disease; hence, these patients were chosen to undergo UKA.
Patients with positive anterior drawer test suggesting anterior cruciate ligament deficiency, and further confirmed with a lateral radiograph when the weight-bearing area was more posterior, as well as osteoarthritis involving the patella–femoral joint and lateral compartment were not considered for UKA.
All functional assessments were performed by trained physiotherapists who were blinded to implant type. All patients were assessed at 2 weeks prior to surgery, then at 6 and 24 months after surgery. Knee of motion was measured passively with a standard goniometer. General quality-of-life outcome was evaluated using the Short Form-36 questionnaire, and disease-specific outcomes were quantified using Knee Society (KSS) as well as Oxford knee (OKS) scores. In addition, the patients were reviewed again at 5 years post-operatively to assess the survivorship of the implant.
All study patients were operated on by the senior authors over a period from 2004 to 2007, each of whom had at least 5 years experience in this surgical procedure. The surgical approach used was the minimally invasive mid-vastus medial parapatellar approach. Intra-operatively, the anterior cruciate ligament was carefully inspected and UKA was performed only if it was intact. Complete medial osteophyte excision was performed for all cases, and medial release was titrated intra-operatively to achieve adequate correction of the deformity. Thereafter, estimated alignment of the knee intra-operatively was assessed by utilisation of the mechanical axis from the hip joint (two finger-breaths medial to the anterior superior iliac spine) to the centre of the knee to the centre of the ankle joint. Post-operative weight-bearing long-leg films of the patient were used to measure the mechanical alignment of the knee with computerised radiological measurement. Mechanical alignment was considered satisfactory if the knee was corrected within 0°–3° of varus.
All study patients were managed on the institution’s standardised knee arthroplasty pathway and underwent the same physiotherapy regimen. IRB (institution review board) approval was obtained prior to commencement of the study.
Statistical analysis
The mean range of motion and mean functional scores was evaluated nonparametrically using the Mann–Whitney U test, and the level of statistical significance was taken to be P < 0.05. All calculations were performed using SPSS version 12.
Results
Both groups were well matched in terms of age, sex, BMI, site of surgery and type of implants (Table 1).
The pre-operative FFD of patients in the severe deformity group (Group A) ranged from 15° to 50°. Twenty-eight patients had FFD between 15° and 20°; ten patients had FFD between 21° and 30°, and two patients had FFD between 31° and 50°. The improvement in FFD in Group A patients post-operatively ranged from 0° to 20°. The 28 patients whose FFD ranged from 15° to 20° had improvement post-operatively as follows: FFD 20° (1 patient), FFD 10° (5 patients), neutral (22 patients). The ten patients whose FFD ranged from 20° to 30° had improvement as follows: FFD 10° (five patients) and neutral (five patients). Both the two patients whose FFD ranged from 30° to 50° had improvement to neutral alignment post-operatively.
There were nine patients whose varus deformity ranged from 15° to 17° and four patients whose varus deformity ranged from 18° to 20° in the severe deformity group. Post-operatively, coronal knee alignment using the mechanical axis for these patients improved. The control group had better correction, though it is not statistically significant (Table 2).
Pre-operatively, Group A patients had poorer knee score and OKS compared with controls (Group B) (Table 3). In addition, Group A patients scored poorer in the mental health component of SF-36 scores, whereas the rest of SF-36 scores was comparable (Fig. 1). Post-operatively, Group A patients were comparable to Group B in maximum flexion angle, KSS, OKS and SF-36 scores (Table 3; Fig. 1).
There were no revisions in the patients with severe deformity (Group A) at 5 years post-operatively (100 % Survivorship at 5 years). There were also no revisions in the control group.
Discussion
The most important finding of the present study was that UKA was effective in correcting the coronal deformity, with a post-operative mean mechanical alignment of 2.8° varus. The correction of coronal deformity was possible in these patients because in addition to bone resections for placement of the prosthesis, medial osteophyte excision and titrated soft tissue releases were performed in order to achieve as close to neutral mechanical alignment as possible. This is to prevent overloading of the tibial component, which will lead to earlier implant failure due to medial tibia collapse. In fact, neutral correction or slight under correction has been recommended for UKA because overcorrection may increase the risk of degeneration in the opposite compartment, whereas under correction may accelerate polyethylene wear and recurrence of deformity [9, 12, 15, 25].
As early as 1987, Kennedy et al. [15] have concluded that superior results were obtained when the post-operative mechanical axis is neutral or in slight varus. Kim et al. [17] also concluded that a post-operative tibiofemoral angle of 4°–6° valgus (anatomic valgus) is associated with the highest survival rate of UKA implants in his study of 246 cases of UKA. The mean mechanical alignment of the severe deformity patients after UKA was at 2.8°, and this was similar to that recommended by Kenney et al. and Kim et al. In fact, this correlated to satisfactory outcomes scores for the severe deformity group that was comparable to that of the control group.
Complete medial osteophyte excision was first performed for all cases and usually sufficient to allow full component range of motion and restoration of alignment. If alignment was still not satisfactory, soft tissue releases were performed and titrated cautiously. Special note was taken not to excessively release the medial collateral ligament in order to correct the coronal alignment, thus preventing excessive ligament balancing and improper ligament tensioning.
Only one patient has tibia vara in the severe deformity group. Post-operatively, the patient had a mechanical axis alignment of 6.9° varus. It must be noted that UKA does not correct the inherent tibia vara and only aims to restore the alignment of the limb to its pre-diseased state. The majority of the patients did not have any significant extra articular tibia deformity. Intra-operatively, it was confirmed that the varus deformity was large due to intra-articular arthritic changes and medial compartment wear.
Generally Group A patients had slightly poorer maximum flexion angle when compared with Group B at pre-operatively and at 2 years post-operatively (Table 3). However, this is not statistically significant and unlikely to be clinically significant as studies have shown that 83° of flexion is required for stair climbing; 93° for rising from a seated position; and 106° for shoelace tying [19].
Patients with severe fixed flexion deformity had FFD correction from 15°–50° pre-operatively to 0°–20° post-operatively. These results indicated that UKA can improve FFD in patients with severe FFD pre-operative and increase post-operative range of motion (ROM).
Patients with severe FFD were penalised heavily in the KSS. This is a biased scoring system that does not reflect the true clinical scenario. This limitation of the scoring system reduces its validity in the assessment of these patients. These patients also had poorer OKS compared with the control group pre-operatively. However, at 2-year follow-up, the knee and function score components of the KSS and OKS had improved for this group of patients and were comparable to that of the control group. The severe deformity group had comparable SF-36 scores to that of the control group, in particular, the physical function, general health and vitality scores were similar between both groups at 2-year follow-up. The physical function, general health and vitality scores are the most precise amongst the 8 scales comprising the SF-36 [20] and also define the widest range of health states (hence usually producing the least skewed score distributions). As such, these results indicate that UKA yields comparable results in terms of QOL benefits for the patients with severe deformity when compared with the control group.
Two different implants were utilised for this study. The choice of implant was surgeon dependent. The senior surgeons who operated on the patients were trained, respectively, and familiar with either the MG UKA or the Preservation UKA implant. These two implants were chosen as both are fixed-bearing femur condylar with unconstrained tibial insert. There was a combination of metal backed and all-poly tibial component, and the choice was dependent on the age of the patient as well as cost consideration.
All the 53 patients with severe deformity completed the 5-year follow-up.
Notably, none of the patients with severe fixed flexion deformity and varus deformity pre-operatively needed a revision arthroplasty at a minimum of 5 years post-operatively. The reason for no revisions in the severe deformity group could be attributed to the fact that the sample size is small in 53 patients (40 FFD and 13 varus). It is a long-standing belief that severe varus and fixed flexion deformity were contraindications to unicondylar knee arthroplasty as they lead to poorer clinical outcomes post-operatively and eventually result in a revision arthroplasty [5, 11, 18]. With such promising results and the advent of newer implants, perhaps these contraindications may no longer hold true. This study proposes that if the patient has predominantly medial compartment osteoarthritis and in addition more severe coronal and sagittal deformity beyond the classical indications for UKA as proposed by Kozin and Scott, he could still be considered for UKA if there was adequate restoration of the mechanical alignment to close to neutral with the help of osteophyte excisions and titrated soft tissue releases.
The 5-year survivorship for both the severe deformity group and control group is 100 %. This compares favourably to the average survivorship of 95 % in a few centres reported in recent years [3, 16, 24, 26]. Nonetheless, there is justification for a larger study comparing the outcomes of UKA patients and TKA patients with severe deformity. The outcomes between these two groups of patients will invariably shed more light on the reliability of UKA as an alternative to TKA in this group of patients.
This is a cohort study comparing the outcomes of UKA in patients with classical indications versus patients with severe deformity. Data were collected from the hospital joint registry, and hence, this was not a randomised control trial. As such, this study did not compare against patients with severe deformity who underwent total knee arthroplasty. The number of patients with severe deformity who underwent UKA is relatively small in 53 patients. However, this is not surprising as most of the patients with severe deformity would have been considered for total knee replacement instead.
This study had a few limitations. There was only a small group of patients with severe varus deformity, and this small sample size may have resulted in an inaccurate representation of outcomes for this group.
Another shortcoming is the relatively short clinical scores assessment and follow-up at 2 years and the implant survival review at 5 years. A longer follow-up of patients would be necessary before the use of UKA as an alternative to TKA for the management of osteoarthritis can be confidently advocated.
Lastly, there was no comparison group of patients with severe deformity who underwent TKA instead of UKA. This might have determined whether the improved functional results from UKA are comparable to that of TKA, and whether TKA would correct the deformities more satisfactorily.
However, the clinical relevance of this study was to demonstrate that patients with severe deformity could undergo a successful UKA with satisfactory outcomes and may not be resigned to total knee arthroplasty as the only viable option. If good mechanical alignment was achieved after UKA, these patients could enjoy improved QOL and function.
Conclusion
This study is one of the first to demonstrate that carefully selected patients with severe deformity beyond the standard indications for UKA can still achieve good function and QOL with UKA, if satisfactory mechanical alignment is restored. There were no revisions in this group at a minimum of 5 years. This study supports a broadening of the indications for UKA, and further follow-up is needed to assess the durability at longer-term follow-up.
References
Beard DJ, Pandit H, Gill HS et al (2007) The influence of the presence and severity of pre-existing patellofemoral degenerative changes on the outcome of the Oxford medial unicompartmental knee replacement. J Bone Joint Surg [Br] 89-B:1597–1601
Beard DJ, Pandit H, Ostlere S et al (2007) Pre-operative clinical and radiological assessment of the patellofemoral joint in unicompartmental knee replacement and its influence on outcome. J Bone Joint Surg [Br] 89-B:1602–1607
Boyd Joel L, Kurtenbach Chad A, Sikka Robby S (2014) Patient-specific instrumentation and return to activities after unicondylar knee arthroplasty. Clin Sports Med 33(1):133–148
Bradbury N, Borton D, Spoo G, Cross MJ (1998) Participation in sports after total knee replacement. Am J Sports Med 26(4):530–535
Cartier P, Sanouiller JL, Grelsamer RP (1996) Unicompartmental knee arthroplasty surgery. 10-year minimum follow-up period. J Arthroplasty 11:782
Chatterji U, Ashworth MJ, Lewis PL, Dobson PJ (2005) Effect of total knee arthroplasty on recreational and sporting activity. ANZ J Surg 75(6):405–408
Dahl AW, Robertsson O, Lidgren L, Miller L, Davidson D, Graves S (2010) Unicompartmental knee arthroplasty in patients aged less than 65. Acta Orthop 81(1):90–94
Emerson RH Jr, Higgins LL (2008) Unicompartmental knee arthroplasty with the oxford prosthesis in patients with medial compartment arthritis. J Bone Joint Surg [Am] 90(1):118–122
Fisher DA, Watts M, Davis KE (2003) Implant position in knee surgery: a comparison of minimally invasive, open unicompartmental, and total knee arthroplasty. J Arthroplasty 18(7 Suppl 1):2–8
Fisher N, Agarwal M, Reuben SF, Johnson DS, Turner PG (2006) Sporting and physical activity following Oxford medial unicompartmental knee arthroplasty. Knee 13(4):296–300
Goodfellow JW, Kershaw CJ, Benson MK, O’Connor JJ (1998) The Oxford knee for unicompartmental osteoarthritis. The first 103 cases. J Bone Joint Surg [Br] 70:692–701
Hernigou P, Deschamps G (2004) Alignment influences wear in the knee after medial unicompartmental arthroplasty. Clin Orthop Relat Res 423:161–165
Huch K, Muller KA, Sturmer T, Brenner H, Puhl W, Gunther KP (2005) Sports activities 5 years after total knee or hip arthroplasty: the Ulm Osteoarthritis Study. Ann Rheum Dis 64(12):1715–1720
Jahromi I, Walton NP, Dobson PJ, Lewis PL, Campbell DG (2004) Patient-perceived outcome measures following unicompartmental knee arthroplasty with mini incision. Int Orthop 28(5):286–289
Kennedy WR, White RP (1987) Unicompartmental arthroplasty of the knee. Post-operative alignment and its influence on overall results. Clin Orthop Relat Res 221:278–285
Keys GW, Ul-Abiddin Z, Toh EM (2004) Analysis of first forty Oxford medial unicompartmental knee replacement from a small district hospital in UK. Knee 11(5):375–377
Kim KT, Lee S, Kim TW, Lee JS, Boo KH (2012) The influence of post-operative tibiofemoral alignment on the clinical results of unicompartmental knee arthroplasty. Knee Surg Relat Res 24(2):85–90
Kozinn SC, Scott R (1989) Current concepts review unicondylar knee arthroplasty. J Bone Joint Surg [Am] 71:145–150
Laubenthal KN (1972) A quantitative analysis of knee motion during activities of daily living. Phys Ther 52:34
McHorney CA, Ware JE, Rogers W, Raczek A, Lu JFR (1992) The validity and relative precision of MOS short- and long-form health status scales and Dartmouth COOP charts: results from the Medical Outcomes Study. Med Care 30(Suppl 15):MS253–MS265
Mullaji AB, Sharma A, Marawar S (2007) Unicompartmental knee arthroplasty: functional recovery and radiographic results with a minimally invasive technique. J Arthroplasty 22(4 Suppl 1):7–11
Naal FD, Fischer M, Preuss A, Goldhahn J, von Knoch F, Preiss S et al (2007) Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med 35(10):1688–1695
Pennington DW, Swienckowski JJ, Lutes WB, Drake GN (2003) Unicompartmental knee arthroplasty in patients 60 years of age or younger. J Bone Joint Surg [Am] 85:1968–1973
Rajasekhar C, Das S, Smith A (2004) Unicompartmental knee arthroplasty 2- to 12-year results in a community hospital. J Bone Joint Surg [Br] 86(7):983–985
Ridgeway SR, McAuley JP, Ammeen DJ, Engh GA (2002) The effect of alignment of the knee on the outcome of unicompartmental knee replacement. J Bone Joint Surg [Br] 84:351–355
Svard UC, Price AJ (2001) Oxford medial unicompartmental knee arthroplasty a survival analysis of an independent series. J Bone Joint Surg [Br] 83(2):191–194
Walton NP, Jahromi I, Lewis PL, Dobson PJ, Angel KR, Campbell DG (2006) Patient perceived outcomes and return to sport and work: TKA versus mini-incision unicompartmental knee arthroplasty. J Knee Surg 19(2):112–116
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seng, C.S., Ho, D.C., Chong, H.C. et al. Outcomes and survivorship of unicondylar knee arthroplasty in patients with severe deformity. Knee Surg Sports Traumatol Arthrosc 25, 639–644 (2017). https://doi.org/10.1007/s00167-014-3464-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3464-9