Abstract
Introduction
When active robotic technologies for Total Knee Arthroplasty (TKA) were introduced over 20 years ago, broad usage of robotic technology was not felt to be needed as early data suggested no clear improvement in clinical outcomes compared to conventional techniques of implantation. Only recently has there been renewed enthusiasm for use of robotic technologies for implantation.
Materials and methods
Active robotic technology specifically refers to the use of a robot for planning and executing the surgical procedure—with surgeon guidance and control. The physical work of bone preparation is performed by a milling tool, following a cut path defined by a CT-based preoperative plan. This manuscript describes the IDE experience of the only active robotic system (ARoS) available in the US, which took place from February 2017 through December 2018.
Results
115 patients were enrolled in an IDE study to evaluate the safety and efficacy of an ARoS for TKA. No previously described safety issues for TKA occurred. Three-dimensional accuracy of component placement used the preoperative CT plan compared to the 3-months postoperative CT scan to demonstrate accuracy of all autonomous resections to within 1.5 mm and/or 1.5 degrees. Surgical planning and execution to restore alignment along kinematic principles were used in 40 procedures and to achieve mechanical alignment in 75 procedures.
Conclusions
This FDA study of an active robotic approach for TKA represented the first multicenter trial and first US experience with this technology. Results demonstrated an excellent safety profile and high degree of accuracy. Advantages of this approach relate to standardization of the technique, multiple device options in the implant library, an excellent safety and accuracy profile, and consistency of results. Active robotics for TKA represents a viable and safe technique for primary TKA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Active robotic technologies for Total Knee Arthroplasty (TKA) were introduced over 20 years ago. Surgical robots classified as “active” perform part of the procedure autonomously. For TKA, a robotic arm equipped with a cutting tool accurately prepares the bony surfaces for implantation without the need for cutting blocks. The surgeon does not guide the robotic arm during cutting. It moves based on preoperative three-dimensional planning done by the surgeon. Initially, there were two active robotic systems (ARoS) that could be used for TKA.
The ARoS called ROBODOC (Integrated Surgical Systems, Sacramento, CA) was first utilized for TKA by Professor Martin Börner starting in 2000 [1]. He attained a postoperative anatomical axis of 0 degrees in 99 out of 100 knees and reported improvements in Knee Society Scores through the first 12 months but did not compare those results with a control group. Around that same time, Siebert et al. reported on a series of 70 TKAs done using the CASPAR active robot (U.R.S.-Ortho, Rastatt, Germany) [2]. They showed significantly better mean postoperative tibiofemoral alignment, 0 ± 1 degree, in the robotic group compared to a historical control group of 50 manually operated TKAs where the mean postoperative tibiofemoral alignment was 2.6 ± 2.2 degrees. However, they did not report any clinical results for comparison between groups.
At that time, broad usage of robotic technology was not felt to be needed as there was no data to suggest a clear improvement in clinical outcomes when compared to conventional techniques of implantation. Only recently has there has been renewed physician and commercial enthusiasm for use of robotic technologies for implantation. There are now several robotic systems available that can be used to assist surgeons during the TKA procedure. The TKA process from planning through implantation for one of these robotic systems, along with results from its initial use in the United States (US), is described in this report.
Materials and methods—active robotics for primary TKA
Patient selection/indications
The ARoS studied through an Investigational Device Exemption (IDE) to obtain clearance for use in the US was the TSolution One® active robotic platform (THINK Surgical, Inc., Freemont, CA) (Fig. 1), which is based off of the ROBODOC platform. When purchased by THINK Surgical, the ROBODOC hardware and software were both updated resulting in a more modernized and streamlined ARoS. The IDE study period for this ARoS was from February 2017 through December 2018. Minimum follow-up for this safety study was 6 months. For this study, indications for use were limited to patients with unilateral osteoarthritis (OA) of the knee, OA severity of Kellgren–Lawrence Grade 3 or higher, no history of prior open knee surgery, BMI ≤ 40 kg/m3, coronal plane deformity < 20 degrees or sagittal flexion deformity < 15 degrees.
Technique
The technique for using the active robotic platform involves three steps after identification of the appropriate patient for robotic TKA: acquisition, planning and implantation.
Acquisition
A computed tomography (CT) scan of the operative limb from the pelvis to the foot is obtained according to a propriety acquisition protocol incorporating a calibration rod. Recommended slice size is 1.25 mm, with average number of CT slices being 800–950, varying with the length of the limb. The manufacturer-provided segmentation and subsequent model generation allow for preoperative planning. The implants included in this study were the Persona® Knee (Zimmer Biomet, Warsaw, IN) and the Unity Knee™ (Corin Group, Tampa, FL) which could both be used in either CR or PS configuration.
Planning
The preliminary plan developed by the robot manufacturer using the default preferences of the surgeon investigator, was sent to the surgeon/surgical team for final review and signature. The plan provided to the surgeon included the exact sizes of femoral and tibial implants, the preferred implant configuration (PCL retaining or PS implant), their precise position on their respective bones (depth, coronal and sagittal angles, desired alignment, including rotation, and planned thickness of tibial inserts). The system allows for planning that matches a surgeon’s philosophy of alignment, presently kinematic (Fig. 2) or mechanical axis (Fig. 3) restoration. The surgeon’s role at this step is to confirm that the style, size and position of the implant in three planes meets with her/his desire for that particular patient’s knee, and achieves the goal of overall limb alignment and component position that she/he wishes. Even though all surgeon planning for implant positioning and sizing is completed at this step, the surgeon must recognize that additional balancing steps may be required intraoperatively that will not be guided by the robot. He/she may wish to adjust the plan accordingly. Once satisfied with the plan, the technique requires the surgeon to formally accept the plan and to commit the plan to the transfer media. The planning steps include:
-
1.
Review segmentation quality
-
2.
Confirm bone landmarks are properly identified
-
3.
Plan size, position, depth and alignment (including rotational alignment) of femoral component
-
4.
Plan size, position, depth and coronal and sagittal alignment of the tibial component. Tibial rotation can be planned and executed by the robot as well and is considered an optional “finishing step” in the plan
-
5.
Determine order of resection and select finishing steps for femur and/or tibia
-
6.
Accept operative plan and save to transfer media (CD or USB flash drive)
The transfer media is inserted in the robot and informs the robot of the cut path necessary for the robotically driven milling tool that prepares the bone surfaces for the desired implant. The surgeon and operating team will know the precise sizes of the implants to be used prior to entering the operating room. Making two digital copies of the plan are recommended.
Implantation
This active robotic approach requires the surgeon to determine an appropriate patient specific plan prior to the operative intervention. The goal at the time of the operation is to use the robotic milling tool to execute the operative plan safely, efficiently and accurately. This procedure involves at least one operative assistant, and it requires the use of a leg holder. Exposure is performed to stabilize and ensure a clear pathway for the robot to work. The registration procedure is a precise surface digitization process that allows the robot to match the operative knee with the internal virtual model developed from the CT data, to ensure proper orientation of the cut paths, and safety of the cutting procedure. There are approximately 36 femoral surface points and 35 tibial surface points captured during registration. If registration points are not accurately collected the robot will reject the registration and require some or all the point digitization to be repeated. One aspect of the learning curve is to accurately register points efficiently. The cutting procedure is performed by the milling tool along a predetermined cut path, with the surgical teams’ role being to ensure adequate exposure to allow unobstructed milling to proceed, to monitor the cutting process at all times, to protect the soft tissues, to remove bone remnants that can decrease efficiency of the milling tool, and to safely remove the robotic arm and associated monitoring pins once the milling has been completed. The steps of the procedure are the following:
-
1.
Expose the knee joint with removal of the patellar surface
-
2.
Excision of medial/lateral menisci, and ACL (PCL if PS knee planned)
-
3.
Placement of stabilization pins into lateral femur, anterolateral tibia, and placement of registration markers: slider pins and tacks in both femur and tibia in appropriate position
-
4.
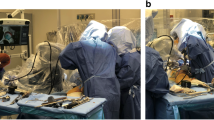
Dock Robot to patient at prescribed distance to allow full robot arm access to the diseased knee (Fig. 4)
-
5.
Place bone motion monitoring probes into tibia/femur to allow robot to monitor for any motion during cutting procedure
-
6.
Registration of the knee through a precise digitization process using the robotic arm digitizer
-
7.
Workspace check by robotic arm to confirm its ability to accomplish milling procedure for femur and tibia
-
8.
Initiation of cutting procedure of femur: during this step, the surgeon/surgical team are clearing bone remnants, removing overhanging cut surfaces, and applying irrigation/suction to surgical field
-
9.
Once femoral preparation is completed, the robot will repeat the workspace check prior to proceeding with tibial milling
-
10.
With completion of milling the robotic arm retracts into the robot base and all monitoring probes, registrations pins/tacks and fixation pins are removed; the robot is removed from the surgical field
-
11.
Implant trials are placed on the femoral, tibial and patellar surfaces and trial reduction is performed; if not performed by the robot, finishing steps for trials (lug holes or box-cut on femur, tibial peg preparation on tibia, peg holes for patella) are done at this stage
-
12.
True implants are implanted
-
13.
Wound closure per surgeon’s technique
Results
A US clinical trial (www.clinicaltrails.gov—NCT03017261) was required for FDA clearance of the device to allow its use in total knee replacement in the United States (510(K) Number: K191369). Some case examples from this US clinical trial have now been published [3] to highlight methods for optimizing the surgical technique. Prior to this study, only isolated experiences of expert surgeons outside of the US have been reported [4]. These studies demonstrated the ability to use an active robot for TKA, and to document placement and alignment of knee components with an accuracy of limb alignment restoration to within ± 3 degrees approaching 99%. What was not clear from these studies was whether this technology could be equally accurate across multiple sites and with surgeons with varying degrees of surgical comfort with robotic technologies.
Ethics approval was obtained from the Western Institutional Review Board and, from February 2017 to December 2018, 115 patients were enrolled in a multicenter 6-month trial to evaluate the safety and efficacy of this robotic platform. This trial was performed at five sites with eight investigators, with the majority of implantations at four sites with four investigators. Surgeon experience ranged from broad experience with Navigation and robotic techniques, to no prior experience. None of the participating surgeons had used this device for TKA surgery prior to this study as all training was performed in cadaver labs. 115 patients were enrolled of whom 107 had a complete robotic procedure. Of the eight that were not fully robotic (6.9%), three procedures had no robotic intervention (one accidental shut-off, two failures to clear work space checks), while five had varying degrees of robotic activity after successful milling of the femur: three required complete manual resection of the tibia, and two required manual completion of a partial tibial robotic resection. In addition to the safety measures that are internal to the robot (milling stops if motion is detected, refusal to proceed if workspace is not adequate), the study demonstrated 0% adverse events commonly reported with manual instrumentation. There were no MCL, extensor mechanism, vascular or neural deficits, no periprosthetic fractures or quadriceps tendon disruptions, and no patella-femoral or tibiofemoral dislocations.
Accuracy was based upon CT-to-CT assessment with postoperative CT at 3 months compared to CT planned implant placement preoperatively for all patients. The mean planned hip–knee–ankle (HKA) angle was 179.3 degrees and the mean postoperative HKA angle differed from the plan by 0.8 ± 1.7 degrees. Preoperative CT to postoperative comparison of planned-to-achieved component position demonstrated that all robot-controlled positions evaluated at 3 months were less than 1.5 mm or 1.5 degrees from planned positions using a previously reported technique [5]. The mean planned tibial slope was 5.3 degrees and the mean postoperative tibial slope differed from the plan by 0.2 ± 1.3 degrees. The mean planned femoral joint line alignment angle (FJLA) was 90.9 degrees and the mean postoperative FJLA angle differed by − 0.6 ± 1.0 degrees. The mean planned tibial joint line alignment angle (TJLA) was 88.9 degrees and the mean postoperative TJLA angle differed by 0.2 ± 1.3 degrees. Greatest variation occurred with tibial rotation, which was manually performed for some patients (several participating surgeons preferred judging tibial rotation intraoperatively (usually for a PS TKA). The learning curve identified for this procedure, 10–20 cases, is the subject of a recently published manuscript [6], where it was reported that coronal alignment accuracy did not differ between the early (learning curve) and late cases.
Discussion
The active robotic platform studied in this FDA required IDE evaluation is that of a system based upon prior experiences with the ROBODOC active robotic system first introduced in 2000 by Professor Martin Börner of Frankfurt, Germany. His initial report of this system detailed the technique and results of his first 100 cases, 76 of which were placed in uncemented fashion. This system had continued use in Asia, with particular interest in South Korea, Japan and Singapore. A number of single center experiences of this system have been reported and demonstrate a high degree of accuracy [7,8,9,10]. These authors have demonstrated significant reduction in radiographic outliers but have failed to show identifiable differences in clinical outcome. A recent report from Liow et al. [11] suggests that with newer outcome tools focused on patient quality of life, slightly better results can be demonstrated using this robotic approach when compared to conventional TKA.
There are several specific advantages unique to an open platform active robotic approach. The open platform robot can be used with any TKA system that is present in the robot’s library. These implants are present in the library because of specific relationships established between the implant and the robotic manufacturers. At present, there are five primary TKA systems in the library of devices available for use with this robot (Table 1). This number is expected to grow as use of this active robot becomes more widespread. Being present in the library means that the appropriate internal dimensions of each implant has been provided to allow development of a cut path that is specific for that implant. The implants for the plan are located in the planning library, and are accessed according to the surgeon preference at the time of planning. The surgeon can choose an implant system as the “default” system for the manufacturer’s plan, but can also choose to independently evaluate available systems’ designs for sizing and fit. An open platform approach also allows the surgeon and/or hospital to address implant pricing variation and negotiate implant costs (for example, our present robotic implant choice has saved approximately $400/implant for our health care system). Additional cost savings can be achieved by decreasing inventory and instruments needed to accurately size and position implants intraoperatively. One tray is required for robot related instruments, but the number of implant specific trays is reduced. Potential benefits have yet to be studied with an active robotic approach.
An open platform technology may also facilitate a number of scientific evaluations. These could include investigations related to implant performance by standardizing implantation technique. In addition, using the same implant, differing alignment and work flow improvements could be evaluated as variation in surgical technique is minimized. Our initial US experience included approaches that used both mechanical and kinematic alignment. Further investigation into variation in alignment philosophy for individualized implant positioning based upon preoperative deformity and implant choice would seem to be appropriate.
At a broader level, there is also the possibility that health care environments might benefit and prefer active robotic approaches to TKA as it would facilitate standardization of the operative process. Standardization improves communication with assisting OR personnel, implant provider and nursing staff. It allows the team to achieve operational efficiencies and increase productivity. Efficient utilization of ancillary personnel might decrease surgeon work requirements per knee replacement. This potential to provide a consistent surgical outcome for a health care system could, at least in theory, accommodate and perhaps accelerate volume growth.
There are also a number of potential disadvantages of this approach as well. The high degree of precision and accuracy of this robotic approach requires that the limb be held rigid—for registration and milling. Decisions regarding ligament release are made after completion of resections and removal of the robotic tool from the operative field. As a result, decisions related to ligament balancing are not assisted by the robot, which provides no feedback as to ligament tension.
Other potential disadvantages to the active robotic approach in its present form include its inability to be used if surgical hardware is in the limb to be operated upon, because the CT image quality is reduced by metal artifacts and cannot be used to create the preoperative plan. Also, the study of active robotics to date has been confined to mild to moderate angular deformities and contractures. Additional advantages and disadvantages to the active robotic approach may appear with more widespread use.
Conclusions
The results of a multicenter US trial demonstrated that an active robotic approach to TKA can be performed safely by surgeons with varying degrees of robotic experience, and can result in highly predictable and precise positioning of total knee components. Resection accuracy and precision previously identified in multiple studies outside of the US were confirmed in the US study, and demonstrated consistency over multiple sites using a similar protocol and technique.
References
Borner M, Wiesel U, Ditzen W (2004) Clinical experience with ROBODOC and the Duracon Total Knee. In: Stiehl J, Konermann W, Haaker R (eds) Navigation and robotics in total joint and spine surgery. Springer-Verlag, Berlin, pp 362–366
Siebert W, Mai S, Kober R, Heeckt PF (2002) Technique and first clinical results of robot-assisted total knee replacement. Knee 9:173–180
Chan J, Auld TS, Long WJ, Kreuzer S, Campanelli V, Liebelt R et al (2020) Active robotic Total Knee Arthroplasty (TKA): initial experience with the TSolution One ® TKA system. Surg Technol Int 37:299–305
Ren Y, Cao S, Wu J, Weng X, Feng B (2019) Efficacy and reliability of active robotic-assisted Total Knee Arthroplasty compared with conventional Total Knee Arthroplasty: a systematic review and meta-analysis. Postgrad Med J 95:125–133. https://doi.org/10.1136/postgradmedj-2018-136190
Campanelli V, Lozano R, Akhlaghpour H, Brar AS, Maislin D, Nedopil AJ et al (2020) Implant placement accuracy in total knee arthroplasty: validation of a CT-based measurement technique. Quant Imaging Med Surg 10:475–484. https://doi.org/10.21037/qims.2020.01.02
Mahure SA, Teo GM, Kissin YD, Stulberg BN, Kreuzer S, Long WJ (2021) Learning curve for active robotic Total Knee Arthroplasty. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06452-8
Jeon S-W, Kim K-I, Song SJ (2019) Robot-assisted Total Knee Arthroplasty does not improve long-term clinical and radiologic outcomes. J Arthroplasty 34:1656–1661. https://doi.org/10.1016/j.arth.2019.04.007
Song E-K, Seon J-K, Park S-J, Jung WB, Park H-W, Lee GW (2011) Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surg Sport Traumatol Arthrosc 19:1069–1076. https://doi.org/10.1007/s00167-011-1400-9
Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL (2013) Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res 471:118–126. https://doi.org/10.1007/s11999-012-2407-3
Cho K-J, Seon J-K, Jang W-Y, Park C-G, Song E-K (2019) Robotic versus conventional primary Total Knee Arthroplasty: clinical and radiological long-term results with a minimum follow-up of ten years. Int Orthop 43:1345–1354. https://doi.org/10.1007/S00264-018-4231-1
Liow MHL, Goh GS-H, Wong MK, Chin PL, Tay DK-J, Yeo S-J (2017) Robotic-assisted Total Knee Arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 25:2942–2951. https://doi.org/10.1007/s00167-016-4076-3
Funding
Funding was provided by THINK to conduct the IDE study to receive FDA approval of the TSolution One active robotic system.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Stulberg received research support from THINK as a PI for the IDE study. He is also a paid consultant/speaker for THINK and has stock or stock options in THINK. Mr. Zadzilka received research support from THINK as a research coordinator.
Ethical approval
The study received ethical approval from the Western Institutional Review Board.
Informed consent
The written informed consent was obtained from all patients prior to their participation in study activities.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stulberg, B.N., Zadzilka, J.D. Active robotic technologies for total knee arthroplasty. Arch Orthop Trauma Surg 141, 2069–2075 (2021). https://doi.org/10.1007/s00402-021-04044-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04044-2