Abstract
Synovial fluid caused by repeated effusions may replete the gastrocnemius-semimembranosus bursa (GSB) communicating with the knee joint. Fluid trapped inside the GSB through an alleged unidirectional valve-like mechanism forms a so-called Baker’s cyst. Since a significant association of Baker’s cysts with knee joint disorders has been reported, treatment should primarily address articular lesions causing recurrent effusions. Arthroscopic surgery provides an effective treatment in that both the cyst and associated joint disorders can be optimally visualized and accordingly treated. In the present paper an all-inside arthroscopic technique for suturing the gateway to the GSB through an anterolateral viewing portal and a posteromedial working portal is proposed. The rationale underlying this technique is that no conclusive evidences exist that the one-way valve-like mechanism is purely anatomical. A retrospective study was conducted on 22 patients (9 males and 13 females, mean age 56 ± 10 SD years) affected by a symptomatic Baker’s cyst associated to knee joint disorders. Pre- and post-operative evaluation at 2 year follow-up consisted of clinical assessment by Rauschning and Lindgren criteria and magnetic resonance imaging (MRI). The results showed that 96% of patients showed clinical improvement. Baker’s cyst disappeared in 64% of patients, reduced in 27% and persisted in 9% on MRI. All patients with cyst reduction exhibited clinical amelioration. Our results suggest the all-inside arthroscopic suture technique would improve Baker’s cyst-related symptoms by either disappearance or reduction of the cyst. We believe the availability of multiple arthroscopic techniques to treat symptomatic Baker’s cysts could broaden the therapeutic armamentarium of knee arthroscopists.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The gastrocnemius-semimembranosus bursa (GSB), which is located in the popliteal region between the medial head of the gastrocnemius and a capsular reflection of the semimebranosus named oblique popliteal ligament, may communicate with the knee joint. When such a communication exists, knee joint effusions may replete the GSB with synovial fluid and if the fluid outflow is hindered by a unidirectional valve-like mechanism, the GSB enlarges giving rise to a pseudocystic cavity referred to as Baker’s cyst [1]. Treatment of Baker’s cysts by open resection is characterized by a high recurrence rate [2]. Since Baker’s cysts are frequently associated with joint disorders causing chronic synovitis and recurrent effusions [1, 3], arthroscopic surgery of Baker’s cysts would provide a more effective treatment in that not only the cyst is addressed by the surgical procedure but associated knee joint disorders can be visualized and treated.
In this paper we present the results of a retrospective observational study assessing the effectiveness of an arthroscopic technique of all-inside suture of the gateway between the knee joint and the GSB in preventing recurrence of symptomatic Baker’s cysts associated to meniscal tears and/or chondral defects treated during the same arthroscopic procedure. The rationale underlying our surgical technique and a comparison of our experience with other techniques and relevant outcomes reported in the literature are also discussed.
Materials and methods
A retrospective observational study was conducted on patients affected by a symptomatic Baker’s cyst admitted for arthroscopic treatment to our department, which is a high-volume knee surgery referral centre. All surgical procedures had been performed by the senior author (V.C.) of this study and an informed consent was signed up by all patients before surgery. Patients had unsuccessfully followed a 12 month course of conservative treatment consisting of activity level modification, non-steroidal anti-inflammatory drugs and physical therapy prior to undergoing surgery. A computer-based search of our database was carried out to retrieve patients satisfying the inclusion/exclusion criteria that were set before commencing data collection. Inclusion criteria were a symptomatic Baker’s cyst communicating with the joint space with or without concomitant meniscal tears and/or chondral lesions and a minimum follow-up of 2 years since surgery. Exclusion criteria were knee joint instability, previous open or arthroscopic knee surgery and patients affected by systemic or local infectious, neoplastic and rheumatic diseases. The inclusion/exclusion criteria aimed at selecting a study sample with a restricted variety of joint disorders as it was thought this would limit the number of disease-related variables making outcome interpretation more difficult. Neoplastic and rheumatic diseases as well as systemic (e.g., viral hepatitis) and local (e.g., urinary tract) infections were excluded because they would add to such unwanted variability owing to their potential of maintaining a systemic inflammation. Patients undergoing previous knee surgery were excluded to limit surgery-related variables (surgical failure, other surgeons’ indications for surgery on which we might have not agreed in the first place).
Clinical history and physical examination of the knee had been conducted by a senior resident in Orthopeadic and Trauma Surgery the day before index surgery. The following pre-operative information was retrieved from the clinical charts for the purposes of the present study: duration of symptoms; relationship of symptoms to rest and to activity level; range of motion (ROM) as measured by arthrogoniometer; swelling in the popliteal fossa assessed by palpation; joint line pain elicited by palpation and by provocative tests for meniscal tears (McMurray test, Steinman test and walking duck test). A Baker’s cyst was regarded as symptomatic and accordingly treated by the technique described in the relevant section of this paper when patients referred pain in the posterior aspect of the knee at rest or during activity and when physical examination showed painful swelling at palpation of the posterior aspect of the knee and/or tension in the popliteal fossa limiting flexion-extension to a variable degree. As far as the clinical evaluation of Baker’s cyst-related symptoms and physical findings is concerned, we adhered to the criteria proposed by Rauschning and Lindgren [5], which have also been used by Sansone and De Ponti [6]. This classification system includes four grades: grade 0 (no swelling and pain, no ROM limitation); grade 1 (light swelling and/or tension in the popliteal fossa following intense activity, minimal ROM reduction); grade 2 (swelling and pain following normal activity, ROM reduction <20°); grade 3 (swelling and pain at rest, ROM limitation >20°).
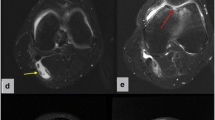
All patients had undergone a magnetic resonance imaging (MRI) scan (Siemens, 1.5 T). Fat-suppression gradient-echo T 1- and T 2-weighted images in the coronal plane and spin-echo T 1- and T 2-weighted images in the sagittal and transverse plane were obtained. The MRI scan was used to confirm the clinical diagnosis of a Baker’s cyst and establish whether the cyst communicated with the joint space, which is a prerequisite for the suture technique herein presented. Conversely, cysts not communicating with the joint would be amenable to percutaneous decompression only. However, cyst communication with the joint is not always detectable on MRI scans, in which case confirmation of an existing communication ultimately relies on arthroscopic inspection.
A thorough arthroscopic inspection preceded suture of the Baker’s cyst and treatment of joint lesions in all patients. A number of pertinent information was retrieved from the intra-operative notes: type of anesthesia; duration of surgery; use of tourniquet; location and type of meniscal tears; location and Outerbridge’s degree of chondral lesions; number of stitches used for suturing the gateway to the GSB; intra-operative complications; type of surgical technique used to address meniscal tears and chondral lesions. In our practice selective meniscectomy aiming at leaving as much of a stable meniscal residual as possible is performed for unrepairable meniscal tears. Full-thickness chondral defects are treated by microfracture chondroplasty according to Steadman technique and criteria [7] (defects less than 400 mm2 wide in patients younger than 65 years with no varus-valgus malalignment >5°). Joint débridement [8] is carried out for chondral lesions not amenable to microfracture chondroplasty.
Antibiotic prophylaxis (2 g cephazolin by intravenous route) was administered 30 min before surgery. Patients underwent spinal anesthesia with 1% hyperbaric marcaine and a tourniquet was always used during surgery. Anti-thromboembolic prophylaxis was administered by subcutaneous injection of 4,000 IU enoxaparin started at 8 pm on the day of surgery and continued for 1 or 6 weeks, respectively, when full and touch-down weight-bearing were recommended. No suction drains were used. Cold therapy was administered for 7 days post-operatively. Analgesics were administered on demand.
Isometric strength exercises were commenced on the day of surgery and crutch-assisted walking was allowed on first post-operative day in all patients. In patients who had not been treated by chondroplasty full weight-bearing as tolerated was immediately allowed and active-passive motion started 3 days after surgery. Conversely, touch-down weight-bearing and continuous passive motion (6 h a day) were recommended for 6 weeks when microfractures had been performed. Skin stitches were removed 10 days after surgery and a follow-up visit was scheduled 1 month after surgery to evaluate knee conditions and patients’ general health. Although no additional follow-up visit was scheduled, patients were advised to refer to our department for any impending problem related to their operated knee.
Patients were contacted 2 years after surgery and invited to attend a follow-up visit and undergo a repeat MRI scan of their knee. Patients unable to reach our department were enquired about their availability to a telephone interview. The follow-up visit was conducted by an orthopaedic surgeon not involved in the study. The clinical outcome related to treatment of Baker’cyst was assessed according to Rauschning and Lindgren criteria, regardless of the outcome of treatment of any other associated joint lesion at the time of surgery. T 2-weighted MRI scans in the sagittal and transverse planes at 2 year follow-up were compared with pre-operative ones by two senior radiologists in order to evaluate the persistence or the disappearance of the cyst. In the event of persistence, it was qualitatively assessed by informal consensus method between the two radiologists whether the cyst showed a reduction compared to its baseline dimensions. Consensus between radiologists was also used to evaluate whether post-operative MRI scans showed any distinctive difference at the level of the gateway to the GSB potentially accounting for cyst disappearance and cyst persistence. Moreover, MRI scans were reviewed to evaluate the presence of knee joint effusion at 2 year follow-up. Finally, the association between clinical improvement, cyst disappearance/persistence and knee joint effusion was analyzed by contingency tables. Since no validated criteria exist to classify clinical improvement according to the system by Rauschning and Lindgren, improvement of at least one grade was used to define clinical amelioration in our study.
All-inside surgical technique of cyst suture
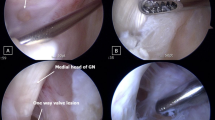
Patients are placed in the supine position after exanguination of the lower limb and application of a tourniquet. The affected knee is set in a leg-holder and hangs free at 90° of flexion. The contralateral lower limb is abducted and slightly flexed to ease maneuvers during suturing. A high anterolateral portal [4] is established and a diagnostic arthroscopy of the knee joint is carried out. The anteromedial portal is placed with the aid of a trial needle in relation to the knee structure(s) to be addressed. Once any other surgical procedure is performed, we proceed to evacuate the Baker’s cyst by a needle inserted percutaneously until the synovial fluid, which is often quite dense and may require squeezing of the cyst, oozes out. The arthroscope inserted through the high anterolateral portal is gently pushed between the medial femoral condyle and the posterior cruciate ligament until it crosses the intercondylar notch and reaches the posteromedial compartment of the knee. The high anterolateral portal is particularly advantageous for the visualization of the gateway to the GSB in that the orifice opens cranially. The more vertical direction of the arthroscope imposed by the high placement of the anterolateral portal eases the visualization of the entry to and the inside of the GSB. Examination is usually performed by a 30° optic. A 70° optic is preferred when the entry to the GSB extends far medially or cranially in the posteromedial compartment. A posteromedial portal is subsequently established under direct visualization and with the aid of a trial needle. The trial needle is also used to inspect and palpate the gateway to the GSB. A clear understanding of the shape and topography of the gateway to the GSB is instrumental to an effective placement of the stitches. Once the location of the posteromedial portal has been determined, we make a stab wound incision that we enlarge with a forceps. A disposable 8 mm threaded arthroscopic cannula (Smith and Nephew, Andover, MA, USA) mounted on a blunt switching rod is then advanced into the joint. The switching rod is removed and a motorized shaver inserted through the cannula. It is very important that the anterior and posterior kissing walls of the entry to the GSB are freshened to obtain two bleeding surfaces, which creates the conditions for first-intention healing after suturing. The blade of the motorized shaver should be oriented posteriorly and medially during wall freshening so as to avert potential damage to the more laterally located neurovascular bundle. A 45° curved cannulated hook of appropriate curvature direction (Linvatec, Largo, FL, USA) is introduced via the threaded cannula and the posterior and anterior kissing walls of the entry to the GSB are purchased (Fig. 1). Since the suture is performed with the knee bent at 90°, both walls should be purchased as caudally as possible. This helps prevent the stitches from cutting across the soft-tissues during knee extension. A # 2 PDS resorbable suture thread is advanced through the cannulated hook and the intraarticular end is retrieved and shuttled outside the joint (Fig. 2). A sliding fisherman’s knot is advanced into the joint by a knot pusher and tied according to an all-inside technique. The free ends are eventually cut flush by a cutter. The number of stitches to be applied depends on the transverse extension of the gateway to the GSB, two stitches generally sufficing to seal the entry to the GSB. Sometimes up to four stitches are required to seal the entry (Fig. 3). The stitches are tied with the knee bent at 90°, so it is mandatory to check that the suture is stable by extending and flexing the knee several times.
Arthroscopic view of the of the posteromedial compartment of a left knee. A cannulated hook of appropriate curvature loaded with a # 2 PDS resorbable suture thread is introduced into the posteromedial compartment of the knee. The hook is maneuvered so as to purchase the posterior and anterior kissing walls of the entry to the Baker’s cyst. After purchasing both cyst walls, the # 2 PDS resorbable suture thread is advanced into the knee joint. The suture of the cyst is performed with the knee bent at 90° so attention should be paid to purchase both walls as caudally as possible in order to prevent the stitches from cutting across soft-tissues during extension
Arthroscopic view of the same left knee as in Fig. 1. The # 2 PDS resorbable suture thread has been advanced into the knee joint and the free end is being retrieved and shuttled through the threaded cannula outside the joint
Arthroscopic view of the same left knee as in Fig. 1. Four suture stitches have been placed to seal the entry to the cyst
Statistics
Wilcoxon’s matched-pairs signed-ranks test was used to analyze pre- and post-operative changes of categorical variables. Clinical improvement was related as dichotomous variable to post-operative cyst condition (categorical variable: cyst disappearance, cyst persisting with unchanged volume and cyst persisting with reduced-volume) by r × c Fisher’s exact test. Association between clinical improvement and absence/presence of knee joint effusion was analysed by 2 × 2 Fisher’s exact test. Two-sided significance level was preset at P < 0.05. Statistical analysis was performed using a dedicated software (StatsDirect, version 2,5,7, StatsDirect Ltd, Cheshire, UK)
Results
Twenty-four patients affected by a symptomatic Baker’s cyst underwent arthroscopic surgery from January 2004 to February 2005. Two out of these 24 patients (8%) were unavailable for a follow-up visit. One patient could not be contacted while the other agreed to a telephone interview and reported his operated knee was symptom-free and functioning well.
Thus a total of 22 patients (9 males and 13 females, mean age 56 ± 10 SD years, age range 30–75 years) were available for physical examination and MRI scan at 2 year follow-up and represent the study sample. The popliteal cyst was unilateral in all cases and the right knee was affected in 10 cases and the left knee in the remaining 12. Median duration of symptoms prior to the 1 year course of conservative treatment was 14 months.
Patients’ pre-operative stratification according to Rauschning and Lindgren criteria was as follows: 2 patients were grade 1 (9%), 15 patients were grade 2 (68%) and 5 patients were grade 3 (23%). Baker’s cyst was associated to an isolated meniscal tear in 7 patients (32%), to isolated chondral defects in 1 patient (4%) and to combined meniscal and chondral lesions in 14 patients (64%). Aspecific synovitis was apparent in all cases during arthroscopic inspection. The type, location and distribution of the associated meniscal and/or chondral lesions are detailed in Table 1.
Meniscal tears were treated by selective meniscectomy. Full-thickness chondral defects were treated by microfracture chondroplasty in three patients (14%) while joint débridement was carried out in the remaining 19 patients (86%). The number of PDS stitches used for cyst suture was 1 in 1 patient, 2 in 11 patients, 3 in 8 patients and 4 in 2 patients. Mean duration of surgery from inflation to deflation of tourniquet was 38 ± 21 SD minutes. No intra-operative complication were recorded.
At 2 year follow-up the following distribution of patients in relation to Rauschning and Lindgren classification was observed: 14 patients were grade 0 (64%), 5 patients were grade 1 (23%), 2 patients were grade 2 (9%) and 1 patient was grade 3 (4%). Post-operative clinical changes from baseline were significant (P < 0.0001). The repeat MRI scan showed that the cyst had disappeared in 14 patients (64%) (Fig. 4), had dimensionally reduced in 6 patients (27%) (Fig. 5) and persisted in 2 patients (9%). The clinical and MRI scan changes following surgery are summarized in Table 2. In one of the two patients in whom cyst persistence was observed, the examination of a ultrasonography scan performed elsewhere owing to tension in the popliteal fossa 4 months before our visit suggested that suture stitches might have partially cut across the soft-tissue ultimately causing suture loosening (Fig. 6).
Ultrasonographic scan of the posterior aspect of the knee in the transverse plane showing persistence of the cyst at 2 year follow-up. The anechogenic linear strip extending to the free edge of the semimembranosus tendon is suggestive of a suture stitch possibly cutting across the tendon. This may have caused suture loosening and cyst recurrence
All 14 patients classified as Rasuchning and Lindgren grade 0 showed cyst disappearance on MRI. Out of the 6 patients who showed cyst reduction on post-operative MRI, 5 patients were grade 2 and 1 patient was grade 3 pre-operatively. Post-operatively, 5 patients were grade1 and 1 patient was grade 2. One patient showing persistence of the cyst on MRI was grade 3 pre-operatively and remained grade 3 at 2 year follow-up, while the other (for whom stitch loosening was suspected based on ultrasonography interpretation) changed from grade 3 to grade 2.
Comparison of MRI scans between cysts that disappeared and cysts that persisted did not enable us to detect any distinct morphological pattern at the level of the gateway to the GSB. Knee joint effusion was detected in 1 out of the 14 patients showing cyst disappearance and in 5 out of the 8 patients in whom the cyst persisted (2 patient having persistence with unchanged volume and 3 patients showing cyst persistence with a reduced volume compared to baseline).
Clinical improvement was significantly associated to post-operative cyst condition (disappearance or persistence with unchanged-reduced volume) (χ2 test, P = 0.0053). Conversely, clinical improvement was not significantly related to the presence or absence of joint effusion (P = 0.23).
Discussion
The prevalence of a communication of the GSB with the knee joint in adults varies in relation to the type of study, the reported figures being 30–50% in cadaveric dissections, 55% in open surgical excision, 37% in knee diagnostic arthroscopies and 50% in arthrograms from normal knees [9]. When the communication exists, a chronic synovitis sustained by intraarticular disorders may cause recurrent effusions filling the GSB with fluid that becomes trapped inside the GSB, which progressively enlarges and forms a pseudocystic cavity. At this stage the term Baker’s cyst should be preferred [1]. Epidemiological studies showed that Baker’s cysts are often associated with knee joint disorders [1, 3, 10]. This association has been observed in our study as well as in the case series published by Sansone and De Ponti [6]. In the presence of an anatomical connection the advocated pathogenesis of a Baker’s cyst would be a one-way valve-like mechanism and the interplay of differential pressures between the GSB and the knee joint during kinematics [9]. It has been reported that the intraarticular pressure in knee joints with effusions is around 33 mm Hg at rest reaching peaks up to 1,300 mm Hg under given conditions [9]. When such high pressures occur, the opening of the gateway to the GSB taking place during flexion may represent a conduit through which synovial fluid is pumped into the bursa, whose entry conversely closes during extension. If the fluid trapped and stagnating inside the GSB becomes denser, as is often the case in chronic Baker’s cysts, the increased viscosity may hinder a retrograde outflow. In other words, the alleged unidirectional valve-like mechanism may be functional and not anatomical in some instances.
Although symptomatic Baker’s cysts are reported to respond to conservative treatment [9], surgery may be required if symptoms related to the cyst persist and limit patients’ knee function.
We believe that the first step in treating a symptomatic Baker’s cysts is performing a meticulous diagnostic arthroscopy followed by treatment of those disorders provoking chronic synovitis. However, not all disorders may be definitively treated, for example diffuse chondral lesions and secondary hypertrophy of the synovial membrane in middle-aged patients. In such cases the knee is predisposed to recurrent effusions and the cyst may eventually recur.
Takahashi and Nagano [2] advocated an arthroscopic technique consisting of disruption of a slit-like structure at the entry to the GSM as the most pathologically suitable method to treat Baker’s cysts. The authors’ statement relies on their hypothesis that capsulosynovial folds consituting the slit-like structure may act as a one-way valve hindering synovial fluid outflow from the cyst.
The study by Sansone and De Ponti [6] recommended removal of anatomical structures (meniscal flaps and/or a fibrous septum) that would cause a one-way passage of fluid from the joint into the cyst by obstructing an oval orifice located between the body and the posterior horn of the medial meniscus. The authors emphasized that treatment of associated joint disorders is a key factor to prevent recurrent effusion and consequently potential persistence of the cyst. The clinical and ultrasonographic findings derived from their case series of 30 patients with a reported rate of 95% optimal or good results at mean 32 months of follow-up would support the use of this arthroscopic technique. An extensive meniscal resection would seem to be required to gain access to the oval orifice described as the access to the cyst. In our experience not all lesions of the medial meniscus, even in the case of complex tears, reach the coronary ligament. A broad meniscectomy in the presence of chondral defects located in weight-bearing areas might unfavourably affect knee function in the long term. Furthermore, Baker’s cysts are not invariably associated to tears of the medial meniscus and it is unclear whether the fibrous septum covering the oval orifice can be easily accessed if the posterior horn of the medial meniscus is intact.
The all-inside arthroscopic suture technique we have described reappraises the concept, previously advocated by other authors [11], of closing the gateway to the GSB to treat Baker’s cysts. The rationale underlying our technique stems from our view that disruption or removal of anatomical structures to re-establish a bidirectional communication ultimately relies on the assumption that the unidirectional valve-like mechanism is purely anatomical. However, there are no conclusive evidences to date this may be the only mechanism at play. We accordingly propose an arthroscopic technique aiming at sealing the entrance to the GSB by placing an appropriate number of stitches to obliterate the virtual capsular opening between the oblique popliteal ligament and the tendinous origin of the medial head of the gastrocnemius. We agree with Sansone and De Ponti that any other associated joint disorder should be surgically addressed in order to minimize the risk of recurrent effusions. However, it should also be acknowledged that broad and full-thickness chondral defects in elderly patients are not amenable to definitive treatment, which accounts for the potential of recurrent effusions.
The results obtained in our study suggest that the all-inside arthroscopic technique would be effective in improving Baker’s cyst-related symptoms. Only one patient (a 62-year-old male farmer) with extensive Outerbridge grade IV chondral defects in the lateral compartment of the knee who was classified as grade 3 according to Rauschning and Lindgren before surgery remained grade 3 at 2 year follow-up. The remaining 21 patients (96%) improved at least one grade in the Rauschning and Lindgren scale at 2 years from surgery. The results of the MRI scan analysis are more disappointing in that cyst disappearance was observed in 64% of cases at 2 year follow-up. A dimensional reduction of the cyst was noted in 27% of patients, all of them showing clinical improvement compared to baseline. The Baker’s cyst persisted in a 62-year-old farmer who continued to be engaged in heavy manual labor and did not improve clinically either. Cyst persistence was also observed in another patient, who clinically improved from grade 3 to grade 2, apparently exhibiting stitch loosening on a ultrasonography scan, which might be interpreted as a potential technique-related complication. Some Authors have in fact questioned the capacity of the sutured capsule to durably resist the high pressure exerted by joint fluid during flexion-extension [6]. Since this finding was a matter of concern to us after its accidental discovery, patients showing cyst reduction on MRI were also subjected to a ultrasonography scan. No sign suggestive of stitch loosening was found in any of the six patients. No difference was detectable at the level of the gateway to the GSB on MRI scans between cysts that disappeared and those that persisted. Thus we are currently unable to definitively establish whether cyst persistence is due to suture failure in all cases. Johnson et al. [1] reported that popliteal bursae showed synovitis if there was synovitis in the knee joint, so it could be speculated that in some cases persistent inflammation of the cyst’s synovial layer may also account for repeated effusions causing cyst recurrence once the gateway to the GSB is sealed by suturing. Should this hypothesis be confirmed in future studies, alternative arthroscopic techniques reported in the literature [2, 6] might be preferred to prevent cyst recurrence in such cases.
One potential limitation underlying the use of this technique is that the access to the posteromedial region of the knee may be hindered in those patients presenting a constitutionally or acquired narrow intercondylar notch, although this has never been the case in our series.
We believe the all-inside technique should be approached by experienced arthroscopists undergoing an adequate learning curve. Potential intro-operative complications may in fact arise from inadvertent injury to the neurovascular structures lying in the popliteal fossa during hook maneuvers. We have not observed any neurovascular complication to date.
A similar technique has been advocated by Kim and Kim [12] to treat chronic capsular defects following open cystectomy using a trans-septal viewing portal and two posterolateral working portals. The authors also recommended their technique should be used by experienced arthroscopists considering the potential for neurovascular damage related to the trans-septal access.
Our study presents a number of limitations. Firstly, the absence of a control group undergoing conservative treatment cannot rule out the possibility that the cysts would have resolved without surgery in the long-term. However, in our series patients had been suffering from cyst-related symptoms for a median of 14 months at the time of their initial presentation to the senior author (V.C.) outpatient practice and they followed a 1 year conservative treatment before surgery. Thus we believe that an adequate amount of time may have elapsed before recommending surgery.
Secondly, it could be advocated that treating the underlying pathology without suturing the cyst might as well lead to cyst disappearance in the long-term. Until randomised controlled trials provide conclusive evidences, however, we have opted for treating symptomatic cysts in combination with associated meniscal tear and/or chondral defects. Our therapeutical attitude would seem to be supported by the significant association found in the present study between clinical improvement and post-operative cyst condition. Performing the all-inside suture does not exceed 10–15 min of added arthroscopic time and has not caused any technique-related complications to date.
Thirdly, the lack of pre-operative ultrasonography scans did not allow us to quantitatively assess cyst volume change from baseline to follow-up. Only pre-operative MRI scans were available for imaging evaluation and the retrospective design of the study could not make up for this limitation. We think that imaging assessment by informal consensus method between two independent observers may have identified cyst dimensional reduction without introducing bias, although we recognize this type of evaluation is only qualitative when compared to formal methods of consensus [13]. Last, the small sample did not allow to conduct a more sophisticated statistical analysis aiming at identifying outcome predictors, if any, that could help refine the indications to the use of the all-inside technique. It could be speculated that the availability of multiple arthroscopic surgical techniques to treat Baker’s cysts would help knee arthroscopic surgeons choose the fittest one to obtain the best outcome if such predictors were identified.
In conclusion the arthroscopic treatment of Baker’s cysts should be preferred to open resection because they would represent an epiphenomenon of a knee joint derangement that is best addressed by arthroscopic surgery. Treatment of associated joint disorders aiming at minimizing the risk of recurrent effusions is crucial to prevent relapsing of the cyst. In this perspective the all-inside suture of the gateway to the GSB combined with arthroscopic treatment of associated meniscal tears and/or chondral defects stands as a technical option that could be effective at improving Baker’s cyst-related symptoms.
References
Johnson LL, van Dyk GE, Johnson CA, Bays BM, Gully SM (1997) The popliteal bursa (Baker’s cyst): an arthroscopic perspective and the epidemiology. Arthroscopy 13:66–72
Takahashi M, Nagano A (2005) Arthroscopic treatment of popliteal cysts and visualization of its cavity through the posterior portal of the knee. Arthroscopy 21:638.e1–638.e4
Rupp S, Seil R, Jochum P, Kohn D (2002) Popliteal cysts in adults. Prevalence, associated intraarticular lesions, and results after arthroscopic treatment. Am J Sports Med 30:112–115
Kim SJ, Kim HJ (2001) High portal: practical philosophy for positioning portals in knee arthroscopy. Arthroscopy 17:333–337
Rauschning W, Lindgren PG (1979) Popliteal cysts (Baker’s cysts) in adults. I: Clinical and roentgenorogical results of operative excision. Acta Orthop Scand 50(5):583–591
Sansone V, De Ponti A (1999) Arthroscopic treatment of popliteal cysts and associated intraarticular knee disorders in adults. Arthroscopy 15:368–372
Steadman JR, Rodkey WG, Briggs KK (2003) Microfracture chondroplasty: indications, techniques and outcomes. Sports Med Arthrosc Rev 11:236–244
Timmermann SA, Kelly MA (2003) Arthroscopic treatment of degenerative joint disease. In: Callaghan JJ, Rosenberg AG, Rubash HE, Simonian PT, Wickiewicz TL (eds) The adult knee, Lippincott Williams & Wilkins, Philadelphia, pp 973–983
Handy JR (2001). Popliteal cysts in adults: a review. Semin Arthritis Rheum 31:108–118
Trecco F, De Paulis F, Masciocchi C, Bonanni G, Beomonte Zobel B, Calvisi V, Romanini L, Passariello L (1984) Clinical interpretation of cysts in the popliteal space using computerised tomography. Ital J Orthop Traumatol 10:109–120
Hughston JC, Baker CL, Mello W (1991) Popliteal cyst: a surgical approach. Orthopedics 14:147–150
Kim SJ, Kim HJ (2004) Arthroscopic repair of chronic capsular defect after popliteal cystectomy. Knee 11:331–334
Murphy MK, Black NA, Lamping DL, McKee CM, Sanderson CFB, Ashkam J et al (1998) Consensus development methods and their use in clinical guideline development. Health Technol Assess 2(3):1–87
Acknowledgments
The authors of the present study wish to thank Dr. Alessandro Guidotti and Dr. Francesca Di Fabio for assessing MRI scans at follow-up.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Calvisi, V., Lupparelli, S. & Giuliani, P. Arthroscopic all-inside suture of symptomatic Baker’s cysts: a technical option for surgical treatment in adults. Knee Surg Sports Traumatol Arthr 15, 1452–1460 (2007). https://doi.org/10.1007/s00167-007-0383-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-007-0383-z