Abstract
Introduction
Proximal femur fractures are associated with an increased mortality rate in the elderly. Early weight-bearing presents as a modifiable factor that may reduce negative postoperative outcomes and complications. As such, we aimed to compare non-weight-bearing, partial-weight-bearing and full weight-bearing cohorts, in terms of risk factors and postoperative outcomes and complications.
Methods
We retrospectively reviewed our database to identify the three cohorts based on the postoperative weight-bearing status the day of surgery from 2003 to 20014. We collected data on numerous risk factors, including age, cerebrovascular accident (CVA), pulmonary embolism (PE), surgical fixation method and diagnosis type. We also collected data on postoperative outcomes, including the number of days of hospitalization, pain levels, and mortality rate. We performed a univariate and multivariate analysis; P < 0.05 was the significant threshold.
Results
There were 186 patients in the non-weight-bearing group, 127 patients in the partial-weight-bearing group and 1791 patients in the full weight-bearing group. We found a significant difference in the type of diagnosis between cohorts (P < 0.001 in univariate, P < 0.001 in multivariate), but not in fixation type (P < 0.001 in univariate, but P = 0.76 in multivariate). The full weight-bearing group was diagnosed most with pertrochanteric fracture, 48.0%, and used Richard’s nailing predominantly. Finally, we found that age was not a significant determinant of mortality rate but only weight-bearing cohort (P = 0.13 vs. P < 0.001, respectively).
Conclusion
We recommend early weight-bearing, which may act to decrease the mortality rate compared to non-weight-bearing and partial weight-bearing. In addition, appropriate expectations and standardizations should be set since age and type of diagnosis act as significant predictors of weight-bearing status.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The annual number of hip fractures worldwide is expected to rise to 4.50 million by the year 2050 [1]. Hip fractures are associated with significant mortality, morbidity, financial burden, and decreased quality of life [2]. In elderly patients’ post-hip fracture, the average one-year mortality rate is between 18 and 33% compared to 3% for the normal population in this age group [3, 4]. Factors that can influence the quality of life after surgery include several comorbidities, rehabilitations options, and postoperative complications.
Of note, early weight-bearing postoperatively is an essential modifiable factor for bone healing and may limit further complications, such as morbidity and mortality. Weight-bearing status can be divided into (i) non-weight-bearing, in which no weight is placed on the limb, (ii) partial weight-bearing, in which weight loading on the limb (30–50%) is progressively increased over time, and (iii) full weight-bearing, in which there is no restriction (100%) to weight-bearing [5]. It has been shown that weight-bearing restrictions may contribute to decreased postoperative mobility and diminished functional levels. At the same time, factors, such as dependent functional health status and dyspnea may predispose patients to an inferior weight-bearing status [6]. However, the relationship between weight-bearing status and postoperative outcomes in proximal femur fractures remains unclear in the literature.
In this study, we aimed to compare three weight-bearing statuses in patients after proximal femur fractures: non-weight-bearing, partial weight-bearing, and full weight-bearing. We examined risk factors (demographic, lifestyle, and surgical) and postoperative outcomes that may influence or affect weight-bearing status. We hypothesized that (i) there would be no difference in risk factors between the weight-bearing groups and (ii) non-weight-bearing status would be most indicative of poor post-operative outcomes compared to the other two weight-bearing groups.
Methods
Between 2003 and 2014, a retrospective review of prospectively collected data was performed in our database to identify three cohorts: non-weight-bearing status, partial weight-bearing status, and full weight-bearing status. A minimum follow-up of 24 months was required. Inclusion criteria included: (1) diagnosis of proximal femur fracture who underwent surgery and (2) adherence to the postoperative protocol as advised by the surgeon and rehabilitation team. Exclusion criteria included: (1) non-operative hip fracture and (2) lack of weight-bearing status classification.
Postoperative protocol
All patients underwent venous thromboembolic disease prophylaxis in the form of 40 mg of Enoxaparin injected intramuscularly at least 12 h after surgery. Normally, our institution recommends progressive weight-bearing as tolerated, including remaining orthostatic and walking as early as possible, until full-weight bearing is possible postoperatively (Fig. 1). If internal fixation is performed, partial weight-bearing for 4–6 weeks is recommended depending on radiological follow-up. In addition, we recommend patients avoid impact activities for at least 6 weeks postoperatively and avoid straight leg raise for 4 weeks postoperatively. Patients are also recommended to partake in rehabilitation, which involves the guidance of a physical therapist who aids in strengthening exercises, balance, and proprioceptive objectives at six weeks postoperatively.
Weight-bearing assessment
Patients were assessed for weight-bearing status on the day of the surgery by the physician. Depending on the outcome, patients were placed into the non-weight bearing group, partial weight-bearing group, or the full-weight bearing group. The non-weight bearing group was selected based on (i) abnormal preoperative function, including bed ridden patients, assisted walking devices prior to surgery, and dementia (ii) no anatomic reduction or shattered bone intraoperatively, or (iii) no recommendation from the physical therapist to bear weight based on the high level of disability or pain. The partial weight-bearing group was chosen based on (i) abnormal preoperative function, (ii) fragile bone, or (iii) physical therapist advising the physician of patient coping issues. The full weight-bearing group was chosen based on (i) normal preoperative function, (ii) no bone quality issues, or (iii) recommendation from the physical therapist.
Risk factors
We collected data on numerous risk factors that could potentially influence the type of weight-bearing group. The risk factors were obtained by the physician at the patients’ preoperative visit before electing for surgery. The risk factors included anticoagulant use (Warfarin), cerebrovascular accident (CVA), pulmonary embolism (PE), diabetes mellitus (DM), and hypertension (HTN).
Postoperative outcomes
Postoperative outcomes were collected by the physician at the patients’ respective follow-up visit (6 weeks, 3 months, 6 months, 1 year, and each subsequent year). The average follow-up in our clinic was 3.5 years (range: 2–5). These measurements included cerebrovascular accident (CVA), pulmonary embolism (PE), deep vein thrombosis (DVT), number of hospitalization days, and pain levels postoperatively.
Statistical analysis
Statistical analysis was performed by IBM SPSS 21 (IBM, Armonk, New York, 2016). Normally distributed continuous data was compared using the Students t test data. A P-value of < 0.05 was used as statistically significant. All variables with a P value < 0.05 from the univariate analysis were included in a multivariable logistic regression model and renamed, adjusted P-value, for which the significance remained at P value < 0.05.
Results
There were 2104 eligible patients who underwent proximal femur fracture surgery by a single surgeon from 2003 to 2014. 186 patients in the non-weight-bearing group, 127 patients in the partial-weight-bearing group and 1791 patients in the full weight-bearing group. In terms of demographics, we found a significant difference between age and BMI > 30. The average age was 83.07 in the non-weight-bearing group, 79.48 in the partial-weight-bearing group, and 78.82 in the full weight-bearing group. The P-value was < 0.0001 in the univariate analysis and 0.02 in the adjusted P-value multivariate analysis. The percent of patients with a BMI > 30, classified as obese, was 6.5% in the non-weight bearing group, 9,4% in the partial weight-bearing group, and 3.4% in the full weight-bearing group. The P-value was 0.001 in the univariate analysis but 0.36 in the multivariate analysis (Table 1).
Fixation type and fracture type
We found a significant difference in terms of diagnosis between cohorts (P < 0.001 in univariate, P < 0.001 in multivariate), but not in fixation type (P < 0.001 in univariate, but P = 0.76 in multivariate). The non-weight bearing group was diagnosed most with subcapital fracture, 57.5%. and used cannulated screw fixation, 38.2%. The partial-weight-bearing group was diagnosed most with subcapital fracture, 48.0%, and used proximal femoral nail fixation. The full weight-bearing group was diagnosed most with pertrochanteric fracture, 48.0%, and used Richard’s nailing predominantly (Tables 2, 3). Also, there was a significant difference in terms of risk factors between the cohorts for anticoagulant use and hypertension, P = 0.03 and P < 0.001, respectively. However, these did not hold for the multivariable analysis (P = 0.99 for anticoagulant use and P = 0.97 for the hypertension) (Table 4).
Postoperative outcomes
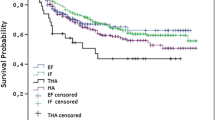
The postoperative outcomes were similar in all the cohorts, including cerebrovascular accident (P = 0.55), pulmonary embolism (P = 0.69, deep vein thrombosis (P = 0.07), and pain levels (P = 0.62). Hospitalization in days differed between the cohorts (P < 0.0001), with the non-weight-bearing cohort spending the fewest number of days in the hospital (7.5 days) and the partial weight-bearing cohort spending the most days in the hospital (9.5 days). In addition, rehabilitation use postoperatively differed between cohorts (P < 0.001). Mortality rate also significantly differed between the cohorts. The non-weight bearing group had the highest mortality rate at 64.7% and the full-weight bearing group had the lowest mortality rate at 38.9% (P < 0.01) at an average follow-up of 5 years. Surprisingly, non-weight bearing group utilized rehabilitation the least, 17.7%, and partial-weight-bearing group utilized rehabilitation the most, 48.8% (Table 5). Finally, we found that age was not a significant determinant of mortality rate but rather weight-bearing cohort (P = 0.13 vs. P < 0.01, respectively) (Table 6).
Discussion
The major findings include the determination that age and preoperative diagnosis are the most relevant risk factors for placement in a specific weight-bearing group. In addition, in terms of postoperative outcomes, the mortality rate at an average follow-up of 3.5 years significantly differed between the cohorts, favoring the full-weight bearing group (38.9%) and disfavoring the non-weight bearing group (64.7%). An interesting finding was that age was not a significant determinant of mortality rate but weight-bearing status instead (Table 6). We found support for our hypothesis in finding the mortality rate was most detrimental to the non-weight bearing group but we did not find support in finding the impact of age and preoperative diagnosis on weight-bearing group. The literature shows supports for the value of early full-weight bearing after proximal femur fractures but is limited in the inclusivity of relevant risk factors for weight-bearing status postoperatively and the role of weight-bearing groups, including a partial weight-bearing group on mortality rate [6, 7]. One systematic review that included 11 studies found improved early postoperative rehabilitation after total knee arthroplasty using biofeedback devices that improved activity level, gait symmetry, and reduced pain postoperatively at a short follow-up (1 to 26 weeks) [8].
The inverse relationship between age and weight-bearing status has been described in the literature. Hagino et al. [9] found that as patients got older after hip fractures, they showed poorer walking ability and poorer recovery of walking ability. Additionally, Thorngren et al. [10] found age to be an important discriminating factor after hip fractures in the elderly in negatively influencing rehabilitation options. Arinzon et al. found that patients over 65–74 years were less functional-dependent after hip fracture. These findings are consistent with our finding that the highest average age of patients in a cohort, 83.07 years, was predictive of placement in the non-weight bearing cohort and the lowest average age, 78.82 years, was predictive of placement in the full-weight bearing cohort.
Type of diagnosis in proximal femur fracture has a close relationship to age in determining weight-bearing group [11]. Louizou et al. [12] found that the subcapital fracture, often seen in femoral neck fractures in the elderly, is mostly dependent on age, amount of fracture displacement, and configuration of fracture fixation. This is consistent with most diagnoses in the non-weight bearing groups and subcapital fractures were most prevalent in the partial-weight bearing group as they were the groups with the highest average age. Meanwhile, the basicervical fracture, which is more vertically oriented and more biochemically unstable, presents in younger adults [13]. Pfeufer et al. [14, 15] found that patients who were diagnosed with pertrochanteric fractures following fracture fixation showed an average load of 62.70%, which is above the average of 51% reported at one week. Additionally, a recent study found that hemiarthroplasty resulted in improving walking postoperatively and a lower rate of reoperation compared to internal fixation at 79 months follow-up [16]. In our study, we found most patients in the full-weight group suffered from pertrochanteric fractures, which is consistent with the positive outcomes of Baccarani et al. [17] after he studied the same diagnosis.
Risk factors for weight-bearing outcomes have been explored throughout the literature. Malik et al. [7] performed a similar analysis but did not include a partial weight-bearing group. They did find several risk factors, such as dependent functional health status, dyspnea with moderate exertion, ventilator dependency, and preoperative dementia that significantly predicted full weight-bearing on the first postoperative day. Partial weight-bearing is used in our institution at an earlier time point (4–6 weeks) than full weight-bearing (8–10 weeks) and acts as another form of a control in this study. The comparison of partial and full weight-bearing has been explored in total hip arthroplasty, showing similar functional outcomes, but remains more novel as a distinct category in femoral neck fractures [18]. Foss et al. and Gdalevich et al. [19, 20] identified anemia, delirium, prolonged surgical time, (greater than 90 min), and delays to surgery may negatively impact postoperative mobility. Many of these factors could be a result of dealing with elder patients, who require more care and involvement of hospital personnel. However, standardization of weight-bearing guidelines, including the outcomes of a partial weight-bearing group may help equilibrate the mobility of patients postoperatively. One study implemented a management system based on a “plan-to-do-check-act” philosophy that standardized aspects of care including, postoperative and early geriatric rehabilitation. They found that patients undergoing surgery for proximal femoral fracture had a reduction in surgical complications in the first two years without a significant difference in mortality, internal complications, or postoperative delirium [21].
Early weight-bearing after proximal femur fractures is associated with positive postoperative outcomes throughout the literature, including decreased mortality rate, functional outcomes, and improved bone healing [22,23,24]. This may be attributed to the early recommendation of weight-bearing at our institution, inclusion of a partial weight-bearing group that has been neglected historically in terms of postoperative protocols, or even rehabilitation process that benefits the non-weight bearing and partial weight-bearing cohorts by providing full, around-the-clock access to physiotherapists for assistance. It would be useful to stratify the postoperative outcomes at each follow-up visit in the future. However, we did find a significant difference in terms of mortality rate between the cohorts. Warren et al. and Siu et al. [10, 25] found that prolonged immobility was associated with higher mortality rates at three months and six months, respectively. Kilci et al. [26] showed that at 3-year follow-up, the cumulative mortality rate was 36.67%, which is consistent with the value of 38.9% in the full-weight bearing group. Ariza-Vega et al. noted that age was independent of mortality rate in older people with hip fractures in a 1-year mortality analysis as we found in our analysis (Table 6) at 3.5-years. The study did not use weight-bearing status as a predictor in their study but found change of residence to be the only potentially modifiable risk factor that influenced the mortality rate [27].
We note limitations in the study. A randomized, prospective study would best demonstrate the study results but due to constraints, we performed a retrospective study. Also, we would expect a multicenter design to show similar results but this approach could be beneficial in making the findings more generalizable. In addition, we did not use any comorbidities scales in order predict mortality rate since we were looking to specifically examine the predictive value of weight-bearing status. A future analysis could compare weight-bearing status to a comorbidity scale to substantiate the role in the analysis. It would also be useful to include postoperative mobility level to compare the weight-bearing group to the patients mobility level. We did maintain a large sample size, and included another control group (partial weight-bearing) that is lacking in the literature. Also, with a follow-up of 3.5 years, we were unable to report on postoperative outcomes at 6-weeks or long-term. Stratifying the outcomes at different time points could be helpful in providing appropriate expectations to physicians and patients alike. However, such a design, allowed us to show that at 3.5 years, patients obtain similar functional and postoperative complication levels without having a similar mortality rate. While we did not include revision rates between the cohorts, we found similar postoperative complications that mitigate this concern. Including more risk factors would be beneficial in a future study [5, 28] in order to see the impact of modifiable risk factors on three weight-bearing cohorts. In addition, finding other factors that predict mortality rate other than weight-bearing group would help substantiate the claim but for the time being, we value the study’s findings.
Conclusion
Early weight-bearing may play a significant role in influencing the mortality rate. In addition, age and type of surgical fixation significantly affect the weight-bearing status of the patient postoperatively. Given these findings, surgeons should set expectations for patients based on age and type of surgical fixation. In addition, early weight-bearing or partial-weight is recommended in patients who are suitable for inclusion in this group.
References
Veronese N, Maggi S (2018) Epidemiology and social costs of hip fracture. Injury 49(8):1458–1460
Royi B et al (2018) The epidemiology and economic burden of hip fractures in Israel. Israel J Health Policy Res 7(1):38
Downey C, Kelly M, Quinlan JF (2019) Changing trends in the mortality rate at 1-year post hip fracture-a systematic review. World J Orthopedics 10(3):166
Scott S et al (2010) The 1-year mortality of patients treated in a hip fracture program for elders. Geriatric Orthop Surg Rehabilit 1(1):6–14
Westerman RW et al (2008) The physiological cost of restricted weight bearing. Injury 39(7):725–727
Malik AT et al (2019) Incidence, risk factors and clinical impact of postoperative delirium following open reduction and internal fixation (ORIF) for hip fractures: an analysis of 7859 patients from the ACS-NSQIP hip fracture procedure targeted database.”. Eur J Orthop Surg Traumatol 29(2):435–446
Kim JW, Byun SE, Chang JS (2014) The clinical outcomes of early internal fixation for undisplaced femoral neck fractures and early full weight-bearing in elderly patients. Arch Orthop Trauma Surg 134(7):941–946
Pfeufer D et al (2019) Training with biofeedback devices improves clinical outcome compared to usual care in patients with unilateral TKA: a systematic review. Knee Surg Sports Traumatol Arthrosc 27(5):1611–1620
Hagino T et al (2008) Comparison of the prognosis among different age groups in elderly patients with hip fracture. Indian J Orthop 42(1):29
Thorngren K-G et al (2005) Influence of age, sex, fracture type and pre-fracture living on rehabilitation pattern after hip fracture in the elderly. Disabil Rehabil 27(18-19):1091–1097
Anderson DE, Madigan ML (2013) Effects of age-related differences in femoral loading and bone mineral density on strains in the proximal femur during controlled walking. J Appl Biomech 29(5):505–516
Loizou CL, Parker MJ (2009) Avascular necrosis after internal fixation of intracapsular hip fractures; a study of the outcome for 1023 patients. Injury 40(11):1143–1146
Hollensteiner M et al (2019) Biomechanics of osteoporotic fracture fixation. Curr Osteoporos Rep 6:1–12
Pfeufer D et al (2019) Weight bearing in patients with femoral neck fractures compared to pertrochanteric fractures: a postoperative gait analysis. Injury 50(7):1324–1328
Koval KJ et al (1998) Postoperative weight-bearing after a fracture of the femoral neck or an intertrochanteric fracture. JBJS 80(3):352–356
Kim J-W et al (2020) Reoperation rate, mortality and ambulatory ability after internal fixation versus hemiarthroplasty for unstable intertrochanteric fractures in elderly patients: a study on Korean Hip Fracture Registry. Arch Orthop Trauma Surg 53:1–8
Baccarani G, Battaglia L, Ceruti A (1979) Rigid fixation and early weight bearing in the treatment of pertrochanteric fractures of the femur. Ital J Orthop Traumatol 5(3):273–283
Tian P et al (2017) Partial versus early full weight bearing after uncemented total hip arthroplasty: a meta-analysis. J Orthop Surg Res 12(1):31
Foss NB, Kehlet H (2006) Hidden blood loss after surgery for hip fracture. J Bone Joint Surg 88(8):1053–1059
Gdalevich M et al (2004) Morbidity and mortality after hip fracture: the impact of operative delay. Arch Orthop Trauma Surg 124(5):334–340
Roll C et al (2019) Continuous improvement process: ortho-geriatric co-management of proximal femoral fractures. Arch Orthop Trauma Surg 139(3):347–354
Warren J et al (2019) The association between weight-bearing status and early complications in hip fractures. Eur J Orthop Surg Traumatol 29(7):1419–1427
Handoll HH, Sherrington C, Mak JC (2011) Interventions for improving mobility after hip fracture surgery in adults. Cochrane Database Syst Rev 3:89
Consigliere P et al (2019) Early versus delayed weight bearing after surgical fixation of distal femur fractures: a non-randomized comparative study. Eur J Orthop Surg Traumatol 29(8):1789–1794
Siu AL et al (2006) Early ambulation after hip fracture: effects on function and mortality. Arch Internal Med 166(7):766–771
Kilci O et al (2016) Postoperative mortality after hip fracture surgery: a 3 years follow up. PLoS One 11(10):16
Ariza-Vega P et al (2015) Predictors of long-term mortality in older people with hip fracture. Arch Phys Med Rehabil 96(7):1215–1221
Atzmon R et al (2018) Cerebrovascular accidents associated with hip fractures: morbidity and mortality—5-year survival. J Orthop Surg Res 13(1345):161
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest in this study.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Atzmon, R., Drexler, M., Ohana, N. et al. The effect of postoperative weight-bearing status on mortality rate following proximal femoral fractures surgery. Arch Orthop Trauma Surg 142, 947–953 (2022). https://doi.org/10.1007/s00402-020-03721-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03721-y