Abstract
Introduction
We aimed to quantify perioperative hidden blood loss (HBL) and investigate its influencing factors in elderly patients with intertrochanteric fractures (IFs) undergoing intramedullary fixation surgery.
Materials and methods
We prospectively collected the clinical data of 200 elderly patients with IFs treated with intramedullary fixation surgery in our hospital between December 1, 2014 and August 31, 2018. The intraoperative visible blood loss, blood transfusion rate, and pre- and postoperative hemoglobin (Hb) levels as well as the general characteristics of the enrolled patients were recorded. A multiple linear regression analysis model (stepwise) was used to identify independent factors affecting perioperative HBL.
Results
The mean perioperative HBL was 614.72 ± 368.14 mL, which accounted for 84.05% of the mean total perioperative blood loss (731.37 ± 391.50 mL). The mean preoperative HBL was 368.33 ± 325.57 mL, which accounted for 50.36% of the mean total perioperative blood loss. Patients with fracture types AO/OTA 31-A2.2 to A3.3 had more severe preoperative HBL (median 580.10 mL), and most of them developed mild-to-moderate anemia before the operation, and 27.63% of them received preoperative blood transfusion. Compared with patients operated within 5 days after injury, patients operated over 5 days had lower Hb value at admission (101.56 ± 19.49 vs. 107.28 ± 16.53; P = 0.026) and higher preoperative transfusion rate (25.84% vs. 9.01%; P = 0.001). Multiple linear regression analysis revealed that fracture types AO/OTA 31-A2.2 to A3.3, male sex, right-sided injury, and operation time > 60 min were independently associated with increased perioperative HBL. Tranexamic acid treatment was negatively correlated with perioperative HBL.
Conclusion
IFs in elderly patients undergoing intramedullary fixation surgery were associated with significant perioperative HBL and anemia. Persistent HBL occurred before the operation and on the first few postoperative days. Surgeons should pay more attention to preoperative HBL in patients with fracture types AO/OTA 31-A2.2 to A3.3 and regularly measure Hb levels preoperatively to avoid anemia. Shortening preoperative time may helps to reduce preoperative blood loss.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With the aging of the population, the incidence of fragility hip fractures in the elderly is increasing. Intertrochanteric fractures (IFs) comprise approximately 50% of all fragility hip fractures in elderly patients [1]. Conservative treatment of these fractures requires long-term bed rest and puts these patients at risk for complications such as pneumonia, bedsores, and urinary tract infection, leading to increased mortality and disability rates. To reduce mortality, preserve joint function, and improve the quality of life of these patients, the current consensus among orthopedic surgeons is that IFs in elderly patients must be treated surgically.
Intramedullary fixation with a proximal femoral nail anti-rotation (PFNA) system is widely used to treat IFs in the elderly because it offers the advantages of short operation time, less blood loss, and reliable fixation. However, many patients who receive this treatment go on to develop postoperative anemia, and up to 41.6% of patients require allogeneic blood transfusion to replace the lost blood [2]. There is a contradiction between the postoperative anemia and the small amount of visible blood loss during this operation. To explain this, Sehat et al. [3] put forward the concept of hidden blood loss (HBL) in 2000, and since then, HBL has become an important factor to be considered in orthopedic surgery. In recent years, some authors have reported that fixation with a PFNA system is associated with significant HBL, as much as 673.2 ± 97.5 mL [4] and 734.2 ± 455.7 mL [2].
Foss et al. [5] prospectively studied 546 patients with hip fractures; they found that the HBL after hip fracture surgery varied from 547 to 1473 mL, and that HBL was significantly associated with medical complications and prolonged hospital stay. Perioperative anemia has also been associated with in-hospital mortality and poor joint function and health-related quality of life after hip fracture surgery [6, 7]. Patient blood-management programs have improved outcomes by decreasing clinical complications, mortality, and delirium, and improving functional recovery in transfused patients [8]. Therefore, quantifying blood loss in the perioperative period and exploring the factors that influence blood loss may help optimize patient blood management and improve the quality of life and prognosis of these patients.
This study was designed to prospectively quantify and investigate influencing factors of perioperative HBL in elderly patients with IFs undergoing intramedullary fixation surgery.
Materials and methods
Patients
We prospectively enrolled consecutive patients who were treated for IF in our hospital between December 1, 2014 and August 31, 2018. The inclusion criteria were age ≥ 60 years, closed fracture with low-impact damage, and extra capsular IF of AO/OTA types 31-A1 to 31-A3 treated using a PFNA system. The exclusion criteria were time from injury to operation > 3 weeks, pathological fracture, contraindications to anticoagulation therapy, multiple fractures with the other fracture(s) requiring surgical treatment, changes to the fixation method intraoperatively, and no postoperative test results.
The study was approved by the medical ethics committee of our institute. All participants or their relatives provided written informed consent.
Data collection
The general characteristics of the enrolled patients were prospectively recorded, including gender, age, height, weight, side of injury (right or left), time from injury to operation, operation time, comorbidity, anesthesia, reduction method, coagulation function, and American Society of Anesthesiologists (ASA) classification [9]. Hemoglobin (Hb) and hematocrit (Hct) were measured on the day of admission, 1 day before the operation, and on postoperative days 1, 2, 3, and 6. Intraoperative visible blood loss was estimated by measuring the blood in the suction apparatus plus the weight of blood in the blood-soaked gauze. In addition, the amount of allogeneic blood transfusion was recorded in each patient. The American Academy of Orthopedic Surgeons recommends postoperative blood transfusion in hip fracture patients when the Hb level is < 80 g/L, even if symptoms are not present [10]. Therefore, in our study, patients were transfused if their Hb level was < 80 g/L or if their Hb level was ≥ 80 g/L, but they had symptoms of excessive blood loss such as tachypnea, tachycardia, or hemodynamic instability.
Surgical procedure
Two experienced orthopedic surgeons performed all the operations. Antibiotics were administered 30–60 min before the operation. Each patient was positioned supine on the fracture traction table after the induction of spinal or general anesthesia, and closed reduction was performed under C-arm fluoroscopy. A minimally invasive technique was used to insert the PFNA system. A guide needle was inserted into the femoral medullary cavity, and an intramedullary nail was placed along the guide needle. C -arm fluoroscopy confirmed that the spiral blade was located in the center of the femoral head and neck in the lateral view, and in lower half or the center of the femoral head and neck in the anteroposterior view; the depth was 5–10 mm under the subchondral bone of the femoral head. One or two static locking screws were inserted into the distal locking hole of the intramedullary nail using the aiming device. No postoperative drainage was used.
Postoperative management
Antibiotics were routinely administered for 48 h after the operation to prevent infection. Low-molecular-weight heparin was routinely administered every 24 h for 2 weeks to prevent thromboembolism after the operation. The amount of fluid infusion required was determined by the surgeon according to the patient’s blood pressure and dietary intake. Patients were encouraged to perform active functional exercises from postoperative day 1. All patients began continuous passive motion on postoperative day 2. Patients with stable fractures with satisfactory reduction and internal fixation began partial weight-bearing with a walker at 1 week postoperatively, while patients with unstable fractures began partial weight-bearing at 2–3 weeks after the operation.
Estimation of blood loss
The total perioperative blood loss was calculated based on the estimated blood volume and the change in Hct between the admission day and postoperative day 3. The following formulas were used to calculate the total perioperative blood loss:
-
1.
Patient’s blood volume = height (m)3 × 0.3669 + weight (kg) × 0.03219 + 0.6041 (for men), and
Patient’s blood volume = eight (m)3 × 0.3561 + weight (kg) × 0.03308 + 0.1833 (for women) [11].
-
2.
Estimated blood loss = patient’s blood volume × (Hctadm − Hctpod3)/Hctav [12].
-
3.
Total perioperative blood loss (mL) = estimated blood loss + blood transfusion.
-
4.
Perioperative HBL (mL) = total perioperative blood loss − intraoperative visible blood loss.
-
5.
Preoperative HBL(mL) = patient’s blood volume × (Hctadm − Hctpre-op)/Hctav1 + blood transfused preoperation.
-
6.
HBL on postoperative day 1 (mL) = patient’s blood volume × (Hctpre-op − Hctpod1)/Hctav2 + blood transfused on operative day.
-
7.
HBL on postoperative days 1–3 (mL) = patient’s blood volume × (Hctpod1 − Hctpod3)/Hctav3 + blood transfused on postoperative days 1 and 2.
Hctadm, Hctpre-op, Hctpod1, and Hctpod3 are the Hct values on the day of admission, 1 day before surgery, and on postoperative days 1 and 3, respectively. Hctav is the average of Hctadm and Hctpod3, Hctav1 is the average of Hctadm and Hctpre-op, Hctav2 is the average of Hctpre-op and Hctpod1, while Hctav3 is the average of Hctpod1 and Hctpod3. If patients received blood transfusion, 1 unit of concentrated red blood cells (CRBCs) was considered equivalent to 200 mL whole blood. For patients without body weight information, the following formula was used: body weight (kg) = [height (cm) × 0.65] − 48.7 (for men), and body weight (kg) = [height (cm) × 0.56] − 33.4 (for women) [2].
Statistical analysis
Categorical variables were reported as frequency and percentage. Continuous variables were reported as mean ± standard deviation or median and interquartile range. The Kolmogorov–Smirnov test was used to assess the normality of distribution of continuous variables. Significant differences between normally distributed continuous variables were detected using the independent-samples t test. One-way analysis of variance was used to compare the means of multiple groups. The least significant difference test was used to compare two groups when the variance was homogeneous, and the Dunnett test was used when the variance was not homogeneous. Pearson correlation analysis was used to test the correlation of various clinical factors with perioperative HBL. Categorical variables were tested using the Pearson’s chi-square test. The association of categorical variables with perioperative HBL was evaluated using univariate analysis. A multiple linear regression analysis model (stepwise) was used to identify independent factors affecting perioperative HBL. P < 0.05 was considered statistically significant. Statistical analyses were performed using IBM SPSS Statistics for Windows, version 20.0. (IBM Corp., Armonk, NY, USA).
Results
General information
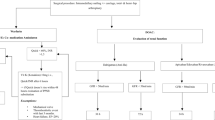
Between December 1, 2014 and August 31, 2018, a total of 208 consecutive elderly patients with IFs were treated with PFNA systems at our hospital. Of these, 204 eligible patients were enrolled in the study. Four patients were excluded because of the following reasons: time from injury to operation > 3 weeks, pathological fracture, and multiple fractures. No patients were lost to follow-up. Another 4 patients with incomplete postoperative data were excluded from the final analysis. Thus, 200 patients were included in the present study (Fig. 1). The clinical characteristics of these patients have been summarized in Table 1.
Perioperative blood loss
The perioperative Hb values, blood loss, and transfusion data are presented in Table 2. The changes in Hb levels at different time points are shown in Fig. 2. The mean Hb level on admission day (104.74 ± 18.08 g/L) was significantly higher than the values 1 day before the surgery and after the surgery (p < 0.01). Although 33 (16.5%) patients received preoperative CRBC transfusion, the mean Hb value 1 day before the surgery (98.70 ± 16.22 g/L) was significantly lower than that on admission day, implying that significant bleeding occurred at the fracture site before the operation. The mean preoperative HBL was 368.33 ± 325.57 mL, which accounted for 50.36% of the mean total perioperative blood loss. Patients with fracture types AO/OTA 31-A2.2 to A3.3 had more severe preoperative HBL (median 580.10 mL), and most of them developed mild-to-moderate anemia before the operation, and 27.63% received preoperative blood transfusion (Table 3). Compared with patients operated within 5 days after injury, patients operated over 5 days had lower Hb value at admission (101.56 ± 19.49 vs. 107.28 ± 16.53; P = 0.026) and higher preoperative transfusion rate (25.84% vs. 9.01%; P = 0.001).
The mean Hb level on postoperative day 2 (87.13 ± 12.41 g/L) was significantly lower than that on postoperative day 1 (92.671 ± 15.08 g/L, P = 0.025). Furthermore, despite the fact that 50 (25%) patients received CRBC transfusion on postoperative days 1 and 2, the mean Hb level on postoperative day 3 was only 90.41 ± 14.67 g/L, indicating that persistent HBL occurred on the first 2 days after the operation. The mean perioperative HBL was 614.72 ± 368.14 mL, which accounted for 84.05% of the total perioperative blood loss (731.37 ± 391.50 mL).
Factors influencing perioperative blood loss
Linear correlation analysis showed that gender, height, weight, injury side (right vs. left), fracture type, and tranexamic acid treatment were correlated with perioperative HBL (Table 4). Univariate analysis of categorical variables revealed that gender, injury side, operation time, fracture type, and tranexamic acid treatment influenced perioperative HBL (Table 5). The results of the multiple linear regression are shown in Table 6. The model was verified using the F test (F = 8.563, P = 0.000). The D–W value was approximately 2, indicating that the model had no autocorrelation, and that there was no correlation between the sample data. In the multiple linear regression analysis, variables that were independently associated with increased HBL were fracture types AO/OTA 31-A2.2 to A3.3, male sex, operation time > 60 min, and injury of right limb. Tranexamic acid had a negative impact on the amount of perioperative HBL.
Discussion
Many studies have demonstrated that PFNA treatment for frail, elderly patients with IFs has the advantages of minimally invasive surgery and decreased intraoperative blood loss [13, 14]. However, as the amount of HBL is very large, postoperative anemia occurs in many patients. Postoperative anemia will aggravate the original disease, and affect postoperative functional recovery and mortality [15,16,17]. Therefore, it is important to detect all types of blood loss and to take timely measures so that patients may survive the operation and recover quickly.
In the present study, we found that IFs in elderly patients undergoing intramedullary fixation surgery were associated with significant perioperative HBL. The mean perioperative HBL was 614.72 ± 368.14 mL, which accounted for 84.05% of the total perioperative blood loss (731.37 ± 391.50 mL). These results are in agreement with those reported in recently published articles. Li et al. [18] retrospectively quantified the perioperative blood loss in elderly patients with IFs treated using unreamed PFNA systems. They found that the cumulative total blood loss from admission to postoperative day 3 was 863.8 ± 429.9 mL, of which the mean HBL was 772.3 ± 424.7 (89.4%), and the mean preoperative HBL was 375.5 ± 242.0 mL. Yang et al. [19] retrospectively investigated perioperative HBL in elderly patients with unstable IFs treated with different intramedullary fixation devices. They found that in the PFNA group, the mean total blood loss was 892.6 ± 234.8 mL, and the mean HBL was 787.7 ± 250.9 mL. The amount of blood loss in their study was slightly higher than that in our study because their patients were taller and heavier than our patients. Cai et al. [20] conducted a prospective randomized controlled trial comparing perioperative HBL in elderly patients with stable IFs treated using intramedullary and extramedullary fixation. In their study, total blood loss (859.43 ± 411.07 mL) and HBL (720.51 ± 408.91 mL) were higher in the intramedullary group than in the extramedullary (P = 0.001).
In clinical practice, surgeons tend to focus on intra- and postoperative blood loss, without taking preoperative bleeding into account. Physical examinations in clinical practice often show that large ecchymoses appear on the thighs and perineum and are gradually aggravated days after sustaining an IF, indicating that sustained fracture-site bleeding occurs after the injury. Consistent with this, we found that the mean preoperative HBL (368.33 ± 325.57 mL) accounted for 50.36% of the mean total perioperative blood loss. Furthermore, the mean Hb level 1 day before the surgery (98.70 ± 16.22 g/L) was significantly lower than that on admission day (104.74 ± 18.08 g/L). Although 16.5% patients received preoperative CRBC transfusion, the incidence of preoperative anemia was 85.9%. Smith et al. [21] conducted a retrospective study, and found that the mean decrease in Hb prior to surgery for extracapsular fractures was 20.2 g/L (range 0–49 g/L). These findings confirmed that patients with IFs had persistent internal bleeding before the operation. This could prove to be dangerous for many patients, especially, if the blood loss remains unidentified. Thus, we believe that clinicians should carefully assess preoperative anemia in this patient group, even if the Hb level is normal at admission. We recommend that all such patients have a repeat Hb level detection prior to surgery.
We also found that Hb levels were lower on postoperative day 2 than on postoperative day 1, indicating that postoperative blood loss occurred not only on the day of the operation but also on the next day. The mean HBL on postoperative days 1–3 was 220.377 ± 256.30 mL. In our study sample, the anemia rate was 94.4% on postoperative day 3, and 55.0% of patients had moderate anemia (Hb < 90 g/L). These results imply that the Hb level should be reexamined not only on postoperative day 1 but also postoperative days 2 and 3 to accurately determine the degree of postoperative anemia.
Few studies have investigated the mechanisms underlying HBL after hip fracture surgery [22, 23]. Foss et al. [5] suggested that HBL may be due to persistent postoperative bleeding, gastrointestinal tract bleeding, and initial traumatic bleeding; they also suggested that the use of anticoagulants may aggravate postoperative bleeding. Wang et al. [24] performed a retrospective analysis and found that age, medical diseases such as diabetes, operation time, and time from trauma to operation may be associated with changes in Hb and Hct levels in IF patients during the early postoperative period after intramedullary nailing treatment. Liu et al. [25] reported that an at-admission albumin level < 30 g/L was associated with a greater likelihood of HBL. In the present study, 20 variables were included in the multiple regression analysis to explore the factors that possibly influence HBL. The results showed that AO/OTA type 31-A2.2–A3.3 fractures, male sex, operation time > 60 min, and right-sided injury were positively correlated with the amount of perioperative HBL, while tranexamic acid treatment was negatively correlated with the amount of perioperative HBL.
The influence of fracture type on blood loss was mainly limited to the preoperative HBL; the blood loss on operation day and after the operation was not correlated with fracture type. The preoperative HBL was greater among patients with AO/OTA types 31-A2.2–A3.3 fractures than among patients with AO/OTA types 31-A1.1–A2.1 fractures (median 580.10 vs. 294.40 mL; P = 0.004), which is consistent with the severity of trauma. The Hb levels on admission day and 1 day before surgery were significantly lower in patients with AO/OTA types 31-A2.2–A3.3 fractures than in patients with AO/OTA types 31-A1.1–A2.1 fractures. Most patients with AO/OTA types 31-A2.2–A3.3 fractures developed mild-to-moderate anemia before the operation, and 55% of these patients required perioperative blood transfusion. These results suggest that AO/OTA types 31-A2.2–A3.3 fractures are a strong predictor of anemia and blood transfusion.
Miao et al. [26] investigated HBL and its influencing factors among patients undergoing total hip arthroplasty using multiple regression analysis, and found that female patients had a higher risk of increased HBL than male patients (P = 0.033). However, in the present study, we found that HBL was significantly higher in male patients than in female patients; however, no significant difference was found between the sexes when HBL was quantified according to the patient’s total blood volume (18 ± 10% vs. 19 ± 11%, P = 0.920). Thus, the higher HBL in male patients may be attributable to their significantly greater total blood volume. In contrast, it is remarkable that female patients had a lower Hb level and higher transfusion rate than male patients both before and after the operation.
Our study did not find a correlation between perioperative HBL and timing of surgery, which may be due to the fact that a considerable proportion of patients with delayed surgery were hospitalized a few days later after injury. The blood loss before hospitalization could not be included in HBL for comparison. However, patients operated over 5 days had lower Hb values and higher preoperative transfusion rates, suggesting that delayed surgery may increase preoperative blood loss.
In this study, 65 patients received intravenous injection of 15 mg/kg body weight of tranexamic acid 15 min before the surgical incision was made and then again 3 h later, and 21 patients received an intramedullary injection of 1 g tranexamic acid intraoperatively. HBL was significantly lower in the patients who received tranexamic acid than in those who did not (530.20 ± 327.64 vs. 674.28 ± 384.63 mL, P = 0.010). Several randomized controlled trials published in recent years have confirmed that tranexamic acid reduces blood loss in the treatment of IF [27,28,29,30].
Curiously, in our study, HBL was significantly higher in patients with IFs of the right limb than in patients with IFs of the left limb. To our knowledge, no study has reported a significant right–left difference in the amount of blood loss during hip fracture surgery. The cause and mechanism of this difference are not clear. We speculate that perhaps there was a significant difference in the proximal femoral blood supply between the two sides, which may be due to variations in the anatomy of the iliac artery and its branches or due to a difference in the severity of arteriosclerosis between the two sides. However, this finding of our study should be interpreted with caution.
Miao et al. [25] showed that blood transfusion can increase HBL after total hip arthroplasty, which may be related to hemolysis. However, in our study, blood transfusion had no significant effect on HBL.
Our research has the advantage of prospective design and data collection, which may ensure the accuracy of measurements and avoid bias due to case selection. However, our study also has several limitations. First, the infusion volume administered perioperatively was not controlled, and this may have affected the calculation of the total perioperative blood loss. Second, a considerable number of patients were hospitalized more than 1 day after the injury, and in these patients, the actual amount of bleeding would have been greater than the calculated amount. Third, because some patients’ weight could not be measured on admission, it was estimated using a formula. The use of the estimated weight would have directly affected the calculation of preoperative blood volume. Finally, the preoperative use of aspirin has been reported to significantly increase HBL [5]. In our study, only five patients used aspirin before the surgery, so we did not include aspirin in the analysis of the influencing factors. In our study, no patients received low-molecular-weight heparin preoperatively, but all patients received it postoperatively. Therefore, it was impossible to analyze whether anticoagulant therapy affected HBL.
In conclusion, IFs in elderly patients undergoing intramedullary fixation surgery were associated with significant perioperative HBL and anemia. Persistent HBL occurred before the operation and on the first few postoperative days. Fracture types AO/OTA 31-A2.2–A3.3, male sex, operation time > 60 min, and right-sided injury were independently associated with increased perioperative HBL. Shortening preoperative time may help to reduce preoperative blood loss. Surgeons should pay more attention to preoperative HBL in patients with fracture types AO/OTA 31-A2.2–A3.3 and regularly monitor Hb levels preoperatively to avoid anemia. We believe that these measures will improve surgical safety and postoperative rehabilitation.
References
Niu E, Yang A, Harris AH, Bishop J (2015) Which fixation device is preferred for surgical treatment of intertrochanteric hip fractures in the United States? A survey of orthopaedic surgeons. Clin Orthop Relat Res 473:3647–3655. https://doi.org/10.1007/s11999-015-4469-5
Hou GJ, Zhou F, Zhang ZS, Ji HQ, Tian Y (2013) Analysis of the blood loss in perioperative period of femoral intertrochanteric fracture in old patients treated with different internal fixations. Beijing Da Xue Xue Bao (Health Sciences) 45:738–741 (article in Chinese)
Sehat KR, Evans R, Newman JH (2000) How much blood is really lost in total knee arthroplasty? Correct blood loss management should take hidden loss into account. Knee 7:151–155
Wei J, Wang J, Gao M, Wang M (2015) Analysis of perioperative blood loss in treatment of senile hip fractures. Chin J Orthop Trauma 17:104–107. (article in Chinese)
Foss NB, Kehlet H (2006) Hidden blood loss after surgery for hip fracture. J Bone Joint Surg Br 88:1053–1059
Sim YE, Sim SD, Seng C, Howe TS, Koh SB, Abdullah HR (2018) Preoperative anemia, functional outcomes, and quality of life after ipH fracture surgery. J Am Geriatr Soc 66:1524–1531. https://doi.org/10.1111/jgs.15428
Sanz-Reig J, Salvador-Marín J, Pérez-Alba JM, Ferrández-Martínez J, Orozco-Beltrán D, Martínez-López JF (2017) Risk factors for in-hospital mortality following hip fracture. Rev Esp Cir Ortop Traumatol 61:209–215. https://doi.org/10.1016/j.recot.2017.03.003
Bielza R, Mora A, Zambrana F, Sanjurjo J, Sanz-Rosa D, Thuissard IJ, Arias E, Neira M, Gómez-Cerezo JF (2018) Impact of a patient blood management program within an orthogeriatric care service. Transfus Apher 57:517–523. https://doi.org/10.1016/j.transci.2018.05.029
Mayhew D, Mendonca V, Murthy BVS (2019) A review of ASA physical status - historical perspectives and modern developments. Anaesthesia 74:373–379. https://doi.org/10.1111/anae.14569
Roberts KC, Brox WT, Jevsevar DS, Sevarino K (2015) Management of hip fractures in the elderly. J Am Acad Orthop Surg 23:131–137
Nadler SB, Hidalgo JU, Bloch T (1962) Prediction of blood volume in normal human adults. Surgery 51:224–232
Gross JB (1983) Estimating allowable blood loss: corrected for dilution. Anaesthesiology 58:277–280
Yu W, Zhang X, Wu R, Zhu X, Hu J, Xu Y, Yi J, Liu Y (2016) The visible and hidden blood loss of Asia proximal femoral nail anti-rotation and dynamic hip screw in the treatment of intertrochanteric fracture of elderly high-risk patients: a retrospective comparative study with a minimum 3 years of follow-up. BMC Musculoskelet Disord 17:269. https://doi.org/10.1186/s12891-016-1143-3
Tang P, Hu F, Shen J, Zhang L, Zhang L (2012) Proximal femoral nail antirotation versus hemiarthroplasty: a study for the treatment of intertrochanteric fracture. Injury 43:876–881. https://doi.org/10.1016/j.injury.2011.11.008
Shander A, Javidroozi M, Naqvi S, Aregbeyen O, Caylan M, Demir S, Juhl A (2014) An update on mortality and morbidity in patients with very low postoperative hemoglobin levels who decline blood transfusion (CME). Transfusion 54:2688–2695. https://doi.org/10.1111/trf.12565
Espinosa KA, Gélvez AG, Torres LP, García MF, Peña OR (2018) Pre-operative factors associated with increased mortality in elderly patients with a hip fracture: a cohort study in a developing country. Injury 49:1162–1168. https://doi.org/10.1016/j.injury.2018.04.007
Vochteloo AJ, van der Borger BL, Mertens B, Niggebrugge AH, de Vries MR, Tuinebreijer WE, Bloem RM, Nelissen RG, Pilot P (2011) Outcome in hip fracture patients related to anemia at admission and allogeneic blood transfusion: an analysis of 1262 surgically treated patients. BMC Musculoskelet Disord 12:262. https://doi.org/10.1186/1471-2474-12-262
Li B, Li J, Wang S, Liu L (2018) Clinical analysis of peri-operative hidden blood loss of elderly patients with intertrochanteric fracture treated by undreamed proximal femoral nail anti-rotation. Sci Rep 8:3225. https://doi.org/10.1038/s41598-018-21703-4
Yang X, Wu Q, Wang X (2017) Investigation of perioperative hidden blood loss of unstable intertrochanteric fracture in the elderly treated with different intramedullary fixations. Injury 48:1848–1852. https://doi.org/10.1016/j.injury.2017.06.017
Cai L, Wang T, Di L, Hu W, Wang J (2016) Comparison of intramedullary and extramedullary fixation of stable intertrochanteric fracture in the elderly: a prospective randomised controlled trial exploring hidden perioperative blood loss. BMC Musculoskelet Disord 17:475
Smith GH, Tsang J, Molyneux SG, White TO (2011) The hidden blood loss after hip fracture. Injury 42:133–135. https://doi.org/10.1016/j.injury.2010.02.015
Millar NL, Deakin AH, Millar LL, Kinnimonth AW, Picard F (2011) Blood loss following total knee replacement in the morbidly obese: effects of computer navigation. Knee 18:108–112. https://doi.org/10.1016/j.knee.2010.03.002
Bao N, Zhou L, Cong Y, Guo T, Fan W, Chang Z, Zhao J (2013) Free fatty acids are responsible for the hidden blood loss in total hip and knee arthroplasty. Med Hypotheses 81:104–107. https://doi.org/10.1016/j.mehy.2013.03.038
Wang J, Wei J, Wang M (2015) The risk factors of perioperative hemoglobin and hematocrit drop after intramedullary nailing treatment for intertrochanteric fracture patients. J Orthop Sci 20:163–167. https://doi.org/10.1007/s00776-014-0667-3
Liu Y, Sun Y, Fan L, Hao J (2017) Perioperative factors associated with hidden blood loss in intertrochanteric fracture patients. Musculoskelet Surg 101:139–144. https://doi.org/10.1007/s12306-016-0447-7
Miao K, Ni S, Zhou X, Xu N, Sun R, Zhuang C, Wang Y (2015) Hidden bood loss and its influential factors after total hip arthroplasty. J Orthop Surg Res 10:36. https://doi.org/10.1186/s13018-015-0185-9
Drakos A, Raoulis V, Karatzios K, Doxariotis N, Kontogeorgakos V, Malizos K, Varitimidis SE (2016) Efficacy of local administration of tranexamic acid for blood salvage in patients undergoing intertrochanteric fracture surgery. J Orthop Trauma 30:409–414. https://doi.org/10.1097/BOT.0000000000000577
Lei J, Zhang B, Cong Y, Zhuang Y, Wei X, Fu Y, Wei W, Wang P, Wen S, Huang H, Wang H, Han S, Liu S, Zhang K (2017) Tranexamic acid reduces hidden blood loss in the treatment of intertrochanteric fracture with PFNA: a single center randomized controlled trial. J Orthop Surg Res 12:124. https://doi.org/10.1186/s13018-017-0625-9
Tian S, Shen Z, Liu Y, Zhang Y, Peng A (2018) The effect of tranexamic acid on hidden bleeding in older intertrochanteric fracture patients treated with PFNA. Injury 49:680–684. https://doi.org/10.1016/j.injury.2018.01.026
Mohib Y, Rashid RH, Ali M, Zubairi AJ, Umer M (2015) Does tranexamic acid reduce blood transfusion following surgery for intertrochanteric fracture? A randomized control trial. J Pak Med Assoc. 65:S17–S20
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Luo, X., He, S., Li, Z. et al. Quantification and influencing factors of perioperative hidden blood loss during intramedullary fixation for intertrochanteric fractures in the elderly. Arch Orthop Trauma Surg 140, 1339–1348 (2020). https://doi.org/10.1007/s00402-019-03311-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-019-03311-7