Abstract
Background
The actual total blood loss after a hip fracture has been found to be considerably larger than that observed during surgery and collected in drainage postoperatively. However, no previous studies have offered reasonable explanations for the deficit between a large hemoglobin drop and a small intraoperative blood loss. The aim was to quantify blood loss associated with hip injuries and surgery, and to identify the relative risk factors for perioperative hidden blood loss.
Materials and methods
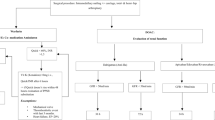
Eighty-nine patients with a femoral intertrochanteric fracture were operated on between August 2012 and October 2013. The patients were accepted to undergo DHS (AO/ASIF) surgery or PFN-a (AO/ASIF) surgery and were randomly assigned to one of the two groups according to whether they had a wound drain or not. Admission information collected included: age, gender, body mass index (BMI), the American Society of Anesthetists system (ASA grading), plasma albumin (ALB), specific gravity of urine (SGU), fracture type (FT), surgery type (ST), and time from admission to surgery in hours (TAS). Blood samples for HB (hemoglobin) analysis were obtained upon admission, at 1 h preoperatively, and at successive postoperation days. The hidden blood loss was calculated by deducting the observed perioperative blood loss from the calculated total blood loss based on the hematocrit changes.
Results
A total of 82 patients with a mean admission lapse time of 4 h after injury remained for the final analysis. One-way analysis of variance (ANOVA) of HBL shows the significant difference was observed in BMI subgroups, ALB subgroups, SGU subgroups, and ST subgroups, but no difference was observed in other subgroups. A multivariate linear regression investigating the relationship between HBL and all factors show that decreased albumin at admission and PFN-a surgery were variables associated with increased HBL.
Conclusions
Several readily available preoperative factors in the form of non-drainage, BMI < 25 kg/m2, admission specific gravity of urine >1.020, surgery type PFN-a, and admission albumin <30 g/L were associated with a greater likelihood of more HBL. In addition, the latter two are independent risk factors for greater HBL in patients with intertrochanteric fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The actual total blood loss after a hip fracture has been found to be considerably larger than that observed during surgery and collected in drains postoperatively [1]. Previous studies have speculated that significant proportion of the blood loss was associated with initial trauma or extravasations of the blood into the tissues during the operation, or also occurred during the entire hospitalization with ongoing blood loss [2, 3]. However, neither one offers a reasonable explanation for the deficit between a large hemoglobin drop and a small intraoperative blood loss. Patients with a hip fracture, who are usually frail and elderly, suffer accompanying anemia and hypovolemia, which should be investigated as potential factors associated with blood loss due to inadequate fluid resuscitation on admission [2, 4]. However, a large proportion of these patients also suffer from hypoproteinemia, which has not been taken into consideration in the literature as a risk factor associated with blood loss following hip fracture. The aim was to quantify blood loss associated initially with a hip injury and subsequent surgical procedure, and to evaluate the characteristics of blood loss over time. Secondly, to identify the relative risk factors for perioperative hidden blood loss (HBL) in patients with a femoral intertrochanteric fracture.
Methods
Participants
Eighty-nine patients who met the criteria (see below) and were operated on between August 2012 and October 2013 in one orthopedic department were enrolled in this prospective, randomized study. The study was conducted after obtaining approval from the hospital institutional review board and informed consents were obtained from all patients.
Inclusion criteria
The inclusion criteria were patients over 65 years old with an intertrochanteric fracture and with no concurrent fracture or injury. The exclusion criteria consisted of pathologic fractures, open fractures, taking drugs that possibly impact blood coagulation (e.g., aspirin, vitamin K antagonists, or platelet inhibitors), non-steroidal anti-inflammatory drugs, alcohol abuse, history of hematopathy or secondary anemia, admission to hospital 12 h or more after trauma, or surgery which was performed three weeks or more after the trauma.
Procedure
The patients were accepted to undergo either DHS (AO/ASIF) surgery or PFN-a (AO/ASIF) surgery within approximately 48 h, and the surgeries were performed under epidural anesthesia. The subjects were randomly assigned to one of the two groups according to whether they underwent a wound drainage or not. The randomization procedure was completed with a computer-generated random allocation sequence. Low molecular weight heparin (enoxaparin, 40 mg subcutaneously once daily) was administered after surgery. Standardized fluid therapy, consisting of Ringer’s solution, was administered on admission. Intraoperative infusion of isotonic saline supplemented by 6% hydroxyethyl starch 130/0.4 was performed with symptoms of hypovolemia, and postoperative intravenous fluids were only administered if the patients’ oral intake was less than 1500 mL per day or when exhibiting signs of hypovolemia. The patients with hypoproteinemia were given a diet supplemented with protein drinks each day, or alternatively were given intravenous supplements of human blood albumin for anorexia. Blood loss was replaced with 6% hydroxyethyl starch 130/0.4 at a rate of 1:1 until the hemoglobin (HB) fell below 90 g/L, at which point transfusion of red blood cells was initiated under the standard allowance.
Data collection
Information collected upon admission included: age, gender, chronic medical conditions, body mass index (BMI), the American Society of Anesthetists system (ASA grading), plasma albumin (ALB), specific gravity of urine (SGU), fracture type (FT), surgery type (ST), and time from admission to surgery in hours (TAS). Blood samples for HB analysis were obtained upon admission, at 1 h (h) preoperatively, and at 1 h, 1 day, 2 days, 3 days, 4 days, and 5 days postoperatively. Drainage was recorded and the drainage tube was removed if the drainage was less than 50 mL.
Blood loss calculation
The HBL was calculated according to a previous study method [5] by deducting the measured blood loss from the calculated total blood loss. The formula used was:
To calculate the total blood loss, we first had to estimate PBV (patient’s blood volume) in milliliters. This was estimated according to the formula [6]:
where k1 = 0.3669, k2 = 0.03219, and k3 = 0.6041 for men, and k1 = 0.3561, k2 = 0.03308, and k3 = 0.1833 for women. The total blood loss was calculated according to the Gross formula [7]:
where Hctadm is the HCT value on admission, Hctfin is the final recorded HCT value on postoperative day five, and Hctave is the average of the Hctadm and the Hctfin.
If transfusions were performed, the total blood loss calculated from the change in Hct was smaller than what it should be in reality, because transfusion renders the patient with a higher Hct than they would have had without a transfusion. Thus, the total blood loss is equal to the loss calculated from the change in Hct plus the volume transfused. The formula is as follows:
The measured blood loss included intra- and postoperative wound drainage. Intraoperative blood loss was evaluated by the measured suction amount plus gauze. Blood loss in saturated gauze is gauze weight difference before and after using/1.05 [8].
Statistical methods
The tests for significant differences between normally distributed data samples were performed using Student’s t test for independent samples. HBL is shown as the mean with 95% confidence intervals, and differences between the groups were analyzed using a one-way analysis of variance (ANOVA). Multivariate linear regression analysis was performed to determine relative factors associated with HBL. A p value <0.05 was considered as statistically significant. All statistical analyses were performed using SPSS version 18 (SPSS Inc., Chicago, IL, USA).
Results
Of the 89 consecutive patients, one was eliminated because of changing to hemiarthroplasty, two because of transferring to another department for treating morbidities postoperatively, and four because of insufficient collection of data. A total of 82 patients with a mean admission time of 4 h after injury remained for the final analysis. Intertrochanteric fracture patients had a mean total blood loss of 1187 ± 165 mL. Their calculated hidden loss was 998 ± 138 mL (rewrit), which was 84% of the total blood loss. The perioperative HB data are presented in Figs. 1 and 2. Intraoperative transfusions were administered to 15 patients and 11 patients received transfusions on the first postoperative day and 10 on the second postoperative day. The mean HB value before transfusions was 92 g/L, which was above the transfusion threshold. The overall transfusion rate was 43.9% and the mean number of units of red blood cells transfused per patient was 1.8. There was a statistical difference in the mean HB value between the transfusion group and non-transfusion group (p < 0.05) in the entire perioperative period, except for at admission and 1 h pre-surgery. Table 1 shows the characteristics of the patients and the HBL variation within different factors: The significant difference of HBL was observed in terms of BMI, ALB, SGU, and ST.
Reduction in hemoglobin admission to surgery, post-surgery and the total (to clarify figure, the reduction in HB was observed in patients receiving transfusion and without transfusion at different time. In the first time period, from trauma to preoperation, HB fell 14 and 13 g/L, respectively, in patients with and without transfusion; in the second period, postoperation, HB drops to 25 and 20 g/L, respectively, in patients with and without transfusion; from trauma to postoperation, HB drops to 39 and 33 g/L, respectively, in patients with and without transfusion)
Whether drainage or a ST had an impact on HBL and total blood loss was analyzed using a factorial design analysis, which is presented in Table 2. (1) The HBL in the patients who had drainage was less than in non-drainage tube group. The difference was statistically significant, but there was no significant difference in total blood loss whether or not there is drainage. (2) In the drainage group, both blood loss during the operation and drainage in the patients with DHS surgery were more than the patients with PFN-a surgery. The results showed sharp reversals in HBL, and the differences were statistically significant. However, there was no significant difference in total blood loss between two types of surgery all of which were with drainage. (3) In the non-drainage group, blood loss during the operation in the patients with DHS surgery was more than that of patients with PFN-a surgery. The results showed sharp reversals in HBL and the differences were statistically significant. However, there was no significant difference in total blood loss between two types of surgery all without drainage.
A multivariate linear regression investigating the relationship between HBL and all factors that could potentially be causatively related to blood loss is shown in Table 3. Decreased albumin at admission and PFN-a surgery were the only variables associated with increased HBL.
Discussion
Historically, the focus of research has been on blood loss during surgery which accounted for transfusion requirements. However, an increasing number of studies have shown that blood loss during surgery is only a small portion of total blood loss during the perioperative period in patients having orthopedic surgery.
Foss [2] assessed 546 hip fracture patients and estimated that the blood loss associated with a hip fracture was six times that occurred in surgery. They hypothesized the “hidden loss” could originate from postoperative hemorrhaging, anti-coagulation, and bleeding from other sources such as the gastrointestinal tract.
Gross reported an average HB decrease post-trauma and also HB prior to intracapsular and extracapsular surgery in a retrospective study of 168 patients with an operative delay of >48 h. Compared to other studies that looked at post-surgery HB, they conjectured that hip fracture patients showed a large drop in HB that was associated with the initial trauma rather than the operation [3, 9].
In this study, all patients on drugs potentially impacting on blood coagulation, and all patients with either a history of hematopathy or secondary anemia that cause intermittent bleeding were excluded. Taking into consideration the decrease in HB in the first hours after injury failed to reflect accurate blood loss due to trauma. Therefore, a series of dynamic observations of HB were performed during the entire perioperative period to identify characteristics of blood loss at different stages.
The study showed that the average HB reduction in the values for the transfusion group and non-transfusion group was 14 and 13.2 g/L, respectively, in the time of post-trauma prior to surgery. However, the values were 25 and 19.2 g/L, respectively, post-surgery (to clarify, the units of measure are not wrong. Those mentioned above are the reduction form one time to another). Deducting the intraoperative blood loss and postoperative drainage from the total blood loss is the generally accepted way of calculating HBL. According to this method, however, the blood loss due to trauma was artificially included in the category of HBL and was unable to be measured precisely. The view is that trauma and surgery should be taken into account simultaneously in the calculation of HBL. Considering the difficulty of measuring blood loss directly and accurately due to trauma timelines, for calculation convenience, we assumed that trauma leading to blood loss included blood loss from admission to pre-surgery, and postoperative hidden blood loss equaled the calculated total hidden blood loss minus the trauma blood loss.
In this study, the mean preoperative HBL was 350 mL and the mean postoperative HBL was 550 mL. Therefore, both trauma and surgery are crucial and are initial reasons for blood loss in patients with intertrochanteric fractures.
The results showed that a BMI < 25 kg/m2, ALB > 30 g/L, SGU > 1.020, and PFN-a surgery were all significantly associated with an increased HBL in the univariate analyses. The same pattern was observed in the multivariate analyses, but BMI and SGU were no longer significantly associated with HBL, though ALB and ST showed a significant relationship with increased HBL.
Although plasma albumin failed to be associated with blood loss in previous studies, the study showed hypoalbuminemia was associated with HBL. It is well known that the reduction in plasma colloid osmotic pressure due to a decrease in plasma albumin causes plasma extravasations, effective circulating blood volume reduction, and fluid accumulation in the tissue chamber. Attention was given to improving perioperative anemia in hip fracture patients who are old and frail. However, hypoalbuminemia status was not considered due to insufficient protein intake or protein synthesis function. This underlines the need for the orthopedic staff to be vigilant about hypoalbuminemia in frail patients even when HB was apparently normal on admission.
To summarize, the present study showed no significant difference in total blood loss between the PFN-a group and DHS group. However, both blood loss during the operation and drainage in the DHS group was more than in the PFN-a group, which had been demonstrated in previous research [10–12]. The results showed sharp reversals in HBL, and in addition, HBL in the PFN-a group was obviously greater than in the DHS group, which was confirmed in the multivariate model analysis as well.
We speculate that soft tissue bleeding occurring in the muscle chamber and part of the drainage from intramedullary bleeding may be relatively limited in the procedure of DHS surgery. Also, in the process of implanting a PFN-a, intramedullary reaming in the proximal femur with an increased bleeding area, the procedure may provide a wide range of storage associated with ongoing bleeding, and also relatively higher pressure in the medullary cavity. The fatty acids produced during intramedullary enlargement might promote the capillary bed opening abnormally, leading to a decrease in the effective circulating blood volume. The total blood loss may be a result of more HBL in the PFN-a group and more intrasurgery blood loss in the DHS group.
Around 33% of the incidence of dehydration in hip fracture patients is quite similar to a group of healthy volunteers aged between 15 and 69 years. Moreover, the increased incidence of dehydration was especially associated with comorbidities before surgery [13]. A trauma reaction could affect the SGU, which reflects renal conservation of water [14]. Ylinenvaara et al. reported that the blood loss and number of transfusions tended to be slightly higher among those who were dehydrated, and blood was transfused in 27% of the euhydrated group compared to 40% of the dehydrated group in a study of 45 patients undergoing acute hip fracture surgery [15].
When patients were admitted to the hospital with insufficient blood volume, we established the impact of dehydration in patients. The pulsing weighted dehydration was 10% on admission. The final data were collected with a methodology to eliminate the perfusion fluid retention effect on fifth day postoperation, which is when a biased estimation of blood loss due to increased perfusion capacity, and hemoglobin dilution might offset each other. Using this calculation method, the results showed the mean HBL in the dehydration group was significantly greater than in the non-dehydration group, although a linear relationship between the SGU and HBL was not established in the multivariate linear regression model. It is suggested that the blood loss in the dehydration group might be overstated according to these calculations, but both chronic dehydration secondary to the initial trauma and the delayed redistribution due to insufficient fluid or acute blood loss could present false HB readings.
Hrnack et al. [16] reported obesity was not correlated with increased intraoperative blood loss in a TKA or THA group. Other studies reported that obesity is one of the risk factors for increased blood loss in patients that had TKA surgery [17, 18]. Previous studies have focused on the influence of obesity on blood loss post-surgery, without an analysis of the relationship between BMI and blood loss following surgery.
This study showed the mean HBL for BMI < 25 kg/m2 was significantly higher than the other two BMI groups and the patients that had hypoalbuminemia had mean HBL values of 23, 12, and 10, respectively, in patients with BMI < 25 kg/m2, BMI that was 25–28, and BMI > 28 kg/m2. It was not uncommon for the patients with hypoalbuminemia to have malnutrition, which showed a linear relationship with BMI [19].
It is inferred that the influence of hypoalbuminemia on blood loss previously, suggesting that reduced plasma globulin and clotting factors might be associated with increased blood loss. Therefore, it is speculated BMI < 25 kg/m2 indicated increased HBL during trauma and the perioperative period. A correlation between BMI and clotting factors during the perioperative period is not obvious, which is one of the limitations in the study. In addition, a linear relationship between BMI and HBL in multiple regression analysis because of the small sample size and large variations in BMI and blood loss could not be established.
The biggest limitation of the present study was that it included few variables that affected blood loss in the model and dehydration influenced bleeding. Another limitation includes the detection of dehydration based on urine analysis that should ideally be based on more than one index. This study showed that several readily available preoperative factors in the form of non-drainage, BMI < 25 kg/m2, admission specific gravity of urine >1.020, surgery type PFN-a, and admission albumin <30 g/L were associated with the greater likelihood of more HBL. In addition, the latter two are independent risk factors for greater HBL in patients with intertrochanteric fractures.
References
Sehat KR, Evans RL, Newman JH (2004) Hidden blood loss following hip and knee arthroplasty: correct management of blood loss should take hidden loss into account. J Bone Joint Surg Br 86B:561–565
Foss NB, Kehlet H (2006) Hidden blood loss after surgery for hip fracture. J Bone Joint Surg Br 88(8):1053–1058
Smith GH, Tsang J, Molyneux SG (2011) The hidden blood loss after hip fracture. Injury 42(2):133–135
Frost SA, Nguyen ND, Black DA (2011) Risk factors for in-hospital post hip fracture mortality. Bone 49:553–558
Sehat KR, Evans RL, Newman JH (2004) Hidden blood loss following hip and knee arthroplasty. Correct management of blood loss should take hidden loss into account. J Bone Joint Surg Br 86:561–565
Nadler SB, Hidalgo JU, Bloch T (1962) Prediction of blood volume in normal human adults. Surgery 51:224–232
Gross JB (1983) Estimating allowable blood loss: corrected for dilution. Anaesthesiology 58(3):277–280
Nadisauskiene RJ, Kliucinskas ML, Dobozinskas P et al (2014) The impact of postpartum haemorrhage management guidelines implemented in clinical practice: a systematic review of the literature. Eur J Obstet Gynecol Reprod Biol 178:21–26
Kumar D, Mbako AN, Riddick A, Patil S, Williams P (2011) On admission haemoglobin in patients with hip fracture. Injury 42(2):167–170
Anglen JO, Weinstein JN (2008) American Board of Orthopaedic Surgery Research Committee. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am 90(4):700–707
Barton TM, Gleeson R, Topliss C, Greenwood R (2010) A comparison of the long gamma nail with the sliding hip screw for the treatment of AO/OTA 31-A2 fractures of the proximal part of the femur: a prospective randomized trial. J Bone Joint Surg Am 92(4):792–798
Matre K, Vinje T, Havelin LI, Gjertsen JE, Furnes O, Espehaug B, Kjellevold SH, Fevang JM (2013) TRIGEN INTERTAN intramedullary nail versus sliding hip screw. J Bone Joint Surg Am 95(3):200–208
Hahn RG, Waldréus N (2013) Urine analysis to detect dehydration. Sport Nutr Exerc Metab 23:303–311
Bartha E, Arfwedson C, Imnell A et al (2013) Randomized controlled trial of goal directed haemodynamic treatment in patients with proximal femoral fracture. Br J Anaesth 110:545–553
Ylinenvaara SI, Elisson O, Berg K (2014) Preoperative urine-specific gravity and the incidence of complications after hip fracture surgery. Eur J Anaesthesiol 31:85–90
Hrnack SA, Skeen N, Xu T, Rosenstein AD (2012) Correlation of body mass index and blood loss during total knee and total hip arthroplasty. Am J Orthop 41(10):467–471
Bowditch MG, Villar RN (1999) Do obese patients bleed more? A prospective study of blood loss at total hip replacement. Ann R Coll Surg Engl 81:198–200
Foss NB, Kehlet H (2005) Mortality analysis in hip fracture patients: implications for the design of future outcome trails. Br J Anaesth 94(1):24–29
Tamura BK, Bell CL, Masaki KH (2013) Factors associated with weight loss, low BMI, and malnutrition among nursing home patients: a systematic review of the literature. J Am Med Dir Assoc 14(9):649–655
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Liu, Y., Sun, Y., Fan, L. et al. Perioperative factors associated with hidden blood loss in intertrochanteric fracture patients. Musculoskelet Surg 101, 139–144 (2017). https://doi.org/10.1007/s12306-016-0447-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-016-0447-7